|
Table of Content - Volume 17 Issue 2 - February 2021
A comparative evaluation of intrathecal bupivacaine and dexmedetomidine versus intrathecal levobupivacaine and dexmedetomidine in vaginal hysterectomy
Neepa S Patel1, Prayati J Shah2*, Subhash K Patel3, Divyang V Shah4
1Assistant professor, 2Resident, 3Associate professor, 4Professor & HOD, Department of Anaesthesia, SMIMER, Surat, Gujrat, INDIA. Email: prayati27@gmail.com
Abstract Background: Spinal anaesthesia provides faster onset with effective sensory and motor block in gynecological surgeries. Isobaric Levobupivacaine (0.5%), pure S (-) enantiomer of racemic hyperbaric Bupivacaine (0.5%) has less cardiotoxicity and neurotoxicity than Bupivacaine (0.5%). Dexmedetomidine, a specific, alpha-2 adrenergic agonist, when used as an adjuvant provides prolonged blockade with post-operative analgesia. The aim of study was to evaluate intrathecal Dexmedetomidine as an adjuvant to hyperbaric Bupivacaine (0.5%) and isobaric Levobupivacaine (0.5%) in vaginal hysterectomy with respect to sensory and motor blockade, hemodynamic stability and post-operative analgesia. Material and method: The prospective, observational study was conducted on 44 adult female patients of ASA physical status 1 and 2 of age group 35-60 years; posted for elective vaginal hysterectomy. The patients were randomly allocated into two groups, namely Group BD and Group LD(n=22),who received 3 ml(15 mg) hyperbaric Bupivacaine (0.5%) with 10 mcg Dexmedetomidine and 3 ml(15mg) isobaric Levobupivacaine (0.5%)with 10 mcg Dexmedetomidine intrathecally at L2-L3 or L3-L4 intervertebral space. Onset and duration of sensory and motor block and hemodynamic stability associated with these drugs were observed. Result: Demographic parameters and duration of surgery were comparable in both groups. Onset and duration of sensory and block was faster in group LD as compared to group BD(p-value<0.05).Although time of onset of complete motor block (min) was almost similar between two groups, time for regression to bromage1(min) was statistically significant (p value<0.01) and duration of analgesia was also prolonged in group LD. Data was analysed using Chi-square test and Unpaired T-test. Conclusion: We conclude that isobaric Levobupivacaine(0.5%) plus Dexmedetomidine provide early and prolonged duration of sensory and motor block as well as post-operative analgesia with stable hemodynamics. Key Words: Vaginal Hysterectomy, Spinal anaesthesia, Levobupivacaine, Bupivacaine
INTRODUCTION The use of spinal anaesthesia in gynecological surgery has shown to provide rapid onset of anaesthesia, adequate muscle relaxation with excellent and comfortable intraoperative condition. Supplementation of adjuvant to local anaesthetic reduces the dose of local anaesthetic, minimizes side effects and prolongs the duration of anaesthesia and analgesia. Racemic hyperbaric Bupivacaine (0.5%), is the most common local anaesthetic used intrathecally in gynecological surgery. Recently, isobaric Levobupivacaine (0.5%), pure S(-)enantiomer of racemic Bupivacaine is used for lower abdominal and lower limb surgery because it has less cardiotoxicity and neurotoxicity. Dexmedetomidine, a specific α-2 adrenergic agonist, exerts its analgesic effect by depressing the release of C-fiber, neurotransmitters and hyperpolarization of post-synaptic dorsal neuron in regional anaesthesia. It prolongs both sensory and motor blockade and has anti-nociceptive action for visceral and somatic pain and proved as a potential adjuvant to local anaesthetic agents in previous studies.[12] It has an alpha 2/alpha 1 selectivity ratio of 1600:1 which is 8 times greater than that of Clonidine.7 The aim of this study was to compare hyperbaric Bupivacaine (0.5%) with Dexmedetomidine(10µg) and isobaric Levobupivacaine (0.5%) with Dexmedetomidine(10µg) intrathecally with respect to assessment of sensory and motor blockade, hemodynamic changes and duration of analgesia.
MATERIALS AND METHODS After taking approval by the Institutional and Ethical Committee (SMIMER/ICE/OUT/NO.7), the study was conducted on 44 ASA I and II patients undergoing vaginal hysterectomy in the age group of 35-60 years under spinal anaesthesia. Sample size was calculated with open epi software version 4.0 with power of 80% and confidence interval of 95% from visual analogue score for post-operative analgesia suggested by Kataria A.P. et al.12 Detailed pre-anaesthesia check-up was done on all patients and relevant hematological, biochemical, and radiological investigations were carried out. Patients with known relative and absolute contraindications for spinal anaesthesia or with cardiovascular, neurological or metabolic disorders were excluded from this study. All the patients were informed about procedure and complications of spinal anaesthesia, drug reaction. Written and informed consent was taken day before surgery. All patients were reviewed pre-operatively. The patients were divided into two groups Group BD and Group LD. (n=22) Group BD patients received 3 ml 0.5% hyperbaric Bupivacaine (15 mg) and Dexmedetomidine (10 μg) Group LD patients received 3 ml of 0.5% isobaric Levobupivacaine (15 mg) and Dexmedetomidine (10 μg) intrathecally. After confirming preoperative fasting, baseline vitals were noted. Intravenous line was secured and patients were preloaded with 10 ml/kg of inj. ringer lactate.Inj. Glycopyrrolate (0.004mg/kg) IM given as a premedication. In operating room, standard monitoring like non-invasive blood pressure, pulse oximeter and electrocardiogram (ECG) leads were attached to patient. After taking all aseptic precautions spinal anesthesia was given using 25-gauge Quinke’s spinal needle, with midline approach in L2-L3 or L3-L4 intervertebral space in sitting position. After confirming free flow of clear CSF study drugs were administered intrathecally according to their group. Intraoperative assessment was carried out by onset of sensory block at T12 (in minutes) by Pinprick method,maximum sensory block level at T8,time to achieve maximum sensory block level (in minutes) and time to achieve complete motor block (in minutes)which was assessed by Modified Bromage Scale.Heart Rate, systolic blood pressure, diastolic blood pressure and SpO2 were measured at 0 min , 5 min, 10 min, 15 min, 20 min, 25 min and every 10 min there after upto 60 min. Time to 2 segmental regression, time for regression to Bromage 1 and time to sensory level regression to S1 were assessed postoperatively. Visual analogue scale (0-10) was used for post-operative pain assessment. Time to first rescue analgesia (Inj. Diclofenac sodium 75 mg i.v.) - time between injection of study drug to the first complain of pain (VAS≥4) was also recorded. Vital parameters assessed for 24hr and any side effects like nausea, vomiting, shivering, headache, dizziness,dry mouth or respiratory depression were observed.
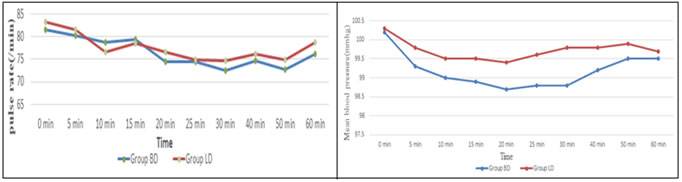
RESULTS Patient demographic data that includes age, height, body weight, duration of surgery and haemodynamic parameters were comparable between two groups (p value>0.05).Time for onset of sensory block at T12 level (min) was slower in Group BD than Group LD, which was statistically significant (p value=0.03),but time to achieve maximum sensory block at T8 (min) was not statistically significant between both groups. Duration of two segment regression of sensory block (min) was shorter for Group BD than Group LD, which was statistically significant (p value=0.003). Time of onset of complete motor block (min) was almost similar between two groups, whereas time for regression to bromage 1(min) was longer for Group LD than Group BD which is statistically significant (p value<0.01) with total duration of analgesia longer for group LD(p-value<0.05).
TABLE 1: DEMOGRAPHIC DATA
TABLE 2: CHARACTERISTICS OF SENSORY BLOCK
TABLE 3: CHARACTERISTICS OF MOTOR BLOCK
FIGURE 1: COMPARISON OF INTRAOPERATIVE PULSE RATE FIGURE 2: COMPARISON OF INTRAOPERATIVE MEAN BLOOD PRESSURE
CHART 1: ONSET OF SENSORY BLOCK AT T12 (MIN) CHART 2: DURATION OF TWO SEGMENT REGRESSION OF SENSORY BLOCK (MIN)
CHART 3: TIME FOR REGRESSION TO BROMAGE 1(MIN) CHART 4: TIME OF FIRST REQUEST FOR POST OP ANALGESIA (MIN)
DISCUSSION Hysterectomy is the second most common gynecological surgery after caesarean section. Nearly 40% of women undergo hysterectomy before the age of 60 years. In this era of opioid free anaesthesia, regional anaesthesia using adjuvant other than opioid has proved safe and beneficial. Levobupivacaine being less cardiotoxic and neurotoxic appears to be an attractive alternative to racemic Bupivacaine.Since many decades hyperbaric Bupivacaine has been used most commonly for spinal anesthesia, but it can cause sudden cardiac arrest after spinal anaesthesia due to extension of the sympathetic block[14][18] and may cause hypotension or bradycardia after mobilization, especially with abrupt position changes. The use of truly isobaric solutions may prove less sensitive to position issues; its baricity offers an advantage of providing a less position sensitive block.[16] We decided to compare Levobupivacaine with Bupivacaine for following reasons: 1.)It is isobaric to CSF[15] 2.)Although hyperbaric solutions have faster onset of time;they have shorter duration of surgical time as compared to isobaric solution.Luck et al..[11] and colleagues also observed that Levobupivacaine and Bupivacaine were clinically same while Ropivacaine had shorter duration of sensory and motor block.11 Alpha 2 adrenergic agonists have both analgesic and sedative properties when used as adjuvant in regional anaesthesia. Dexmedetomidine, a highly selective, α2-adrenergic agonist, has analgesic, sedative, and anaesthetic-sparing effects when used in systemic route. In previous studies, it was concluded that addition of Dexmedetomidine to Levobupivacaine produces effective analgesia and prolongs the duration of motor and sensory block along with better postoperative analgesia and fewer side effects.[4] In our study,we also observed that early onset of sensory block and prolonged duration of post-operative analgesia in group LD than group BD(p-value<0.05); resulting in reduction of requirement of rescue analgesia. Incidence of side effects like nausea, vomiting, bradycardia, hypotension were lesser with Levobupivacaine. In present study,we selected patients undergoing vaginal hysterectomy and the study demonstrated adequate surgical anaesthesia with comparable intraoperative hemodynamic changes in both groups;duration of surgery was nearly 2 hours in our institute. In 2016, Amio Kumar Deori et al. [1] studied intrathecal 2.5 ml 0.5% isobaric levobupivacaine with 2.5 ml 0.5% hyperbaric bupivacaine in spinal anaesthesia for lower segment caesarean section in 150 pregnant women.He found that duration of sensory and motor blockade was longer with Bupivacaine group,but Levobupivacaine had lesser side effects and patient remained more stable hemodynamically than Bupivacaine group. Amar Parkash et al. 12 has studied isobaric Levobupivacaine (0.5%)3 ml along with isobaric Levobupivacaine(0.5%)3 ml with Dexmedetomidine 0.3 ml(3 μg) in infraumbilical surgeries under spinal anaesthesia.. The two groups were compared with respect to the onset and duration of sensory and motor block and hemodynamic stability. Group Levobupivacaine and Dexmedetomidine had early-onset and prolonged duration of sensory and motor block and longer duration of postoperative analgesia than Group Levobupivacaine alone.This results are in accordance to our study.
CONCLUSION This study conclude that both groups are effective in providing surgical anaesthesia and hemodynamic stability,but Levobupivacaine provides early onset of sensory and motor blockade with cardiovascular safety than Bupivacaine.Addition of Dexmedetomidine prolongs the duration of blockade,provides longer duration of post-operative analgesia.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home