|
Table of Content - Volume 17 Issue 2 - February 2021
Study of intrathecal fentanyl and midazolam for prevention of nausea and vomiting during of caesarean delivery under spinal anaesthesia in Andhra Pradesh population
Ramesh Babu Vedangi1, Anil kumar Reddy K2*
1Associate Professor, Department of Anaesthesiology, Maharajah’s Institute of Medical Sciences, Nellimarla, Vizianagaran, Andhra Pradesh – 535217, INDIA. 2Assistant Professor, Department of Anaesthesiology, Mediciti Institute of Medical Sciences, Ghanpur, Medchal-501401, Telangana, INDIA. Email: kandianil@yahoo.com
Abstract Background: Nausea, vomiting are the quite common complication during and after immediate caesarean surgery. Hence apart from relieving pain anti emetic drugs play vital role hence different anaesthetic drugs were compared to get early relief to the patient. Method: Out of 90 patients 30 patients were grouped in three – group I received intra-thecal placebo, group-II received IT midazolam 2mg and group-III received IT fentanyl 12-5mg study agents were co-administered along with 2.0m/hyperbaric pubivacine (0.5%). Results: The emetic episodes were least in group III – Nausea4 (4.4%) retching 2 (2.2%) vomiting 1 (1.1%) followed by group II had 7 (7.7%) Nausea while highest incidence was in group- I. Adverse reactions like shivering 0% in group-III 2 (2.2%) in group II, 3 (3.3%) in group I, but prurititis was 2 (2%) only in group III and neonatal effects like Apgar scores and NACS score were quite normal in neonates belong to all three group. Conclusion: Midazolam or Fentanyl significantly minimizes the incidence of nausea and vomiting during intra-operative and early post-operative period during caesarean delivery. Keywords: CS Caesarean Delivery PONV, IT-Intrathecal, Nausea and Vomiting, Apgar score, NACS score.
INTRODUCTION The most common and distressing symptoms which follow anaesthesia and surgery are pain, nausea and vomiting remain as the “big title problem” in caesarean section (CS) under spinal anaesthesia (SA)1. The causes of PONV are multifactorial and categorized in patients as risk factors, anaesthetic techniques and surgical procedure. Antiemetic drugs work on several different receptor sites to prevent and treat PONV2. Incidence of nausea vomiting during and immediately after surgery in spinal anaesthesia is high and is an annoying problem to all concerned. It is distressing to both physically and mentally to the patient and disturbing to the surgeon and anaesthesiologist vomiting can leads to multiple problems like dehydration, electrolyte imbalance, decreased patient’s satisfaction, and also causes an economic burden3. Intra operative nausea and vomiting occurs in as many as 66% of CSs and performed under regional anaesthesia. This can be distressing to the patient, and may increase the risk of aspiration contents4. Intrathecal Midazolam and fentanyl produce post-operative pain relief for women undergoing CS, while having antiemetic effect also hence these two drugs and one placebo drugs were give to three groups individually and their intra-operative complications, operative management episodes of emetic symptoms were evaluated.
MATERIAL AND METHOD 90 (Ninety) full term pregnant patients admitted at obstetrics and gynaecology department of Maharaja’s Institute of Medical Sciences, Nellimarla Vizianagram (dist), Andhra Pradesh-535217 were studied. Inclusive Criteria: Full term parturient of ASA physical status I, Scheduled for elective caesarean delivery were selected for study. Exclusive Criteria: The patients having history of hyperemisis gravidarum, Contraindications to regional anaesthesia. The patients had GIT diseases, foetal prematurity (36 weeks) or those who have received anti emetics 24 hours prior to surgery, ASA physical status II, III patients were also excluded from the study. Methods: The parturient were given 150mg Ranitidine tablet orally as premedication 90-100 minutes before surgery. The patients were attached routine monitoring devices, baseline blood pressure, heart rate, ECG and pulse oximetry values were recorded. Ringer lactate solution 20ml/kg was given I V to every patient before spinal anaesthesia. Dural puncture was performed at L3-L4 interspace with a 25 gauge spinal needle. The blocks were performed with the patient in the lateral decubitus position. The patients were randomly allocated using a random number table to receive intrathecally one of the medications. The study solutions were constituted 2ml of hyperbaric bepuvacaine (0.5%) plus 0.5ml of normal saline (Groups I), 2 mg of Midazolam (group II) 12.5µg of fentanyl (group III) Total. Volume of study agents was 2.5ml the study agents were injected IT by an Anaesthesiologist. After injection of the study solution, the patients were turned to supine position with a 15o wedge under the right hip for left uterine displacement. Oxygen (3 Litre) was administrated via face mask. The decreased in systolic blood pressure (more 20% from base line values and/or less than 90 mmHg) immediately after spinal injection was treated by increasing the rate of intra venous fluid administration, by exaggerating the uterine till and by injected ephedrine 5 to 10 mg IV. The level of analgesia was assessed by pin prick before surgical incision. The surgical technique was uniform to all patients and included exteriorization of the uterus. 10 IU of oxytocin was given intravenously after delivery of the baby and clamping of the umbilical cord. An attending paediatrician assessed the neonatal Apgar scores at 1 and 5 minutes after delivery, post-operatively, patients were observed for 3 hours and pulse rate oxygen saturation and blood pressure was monitored every 10 minutes. An urinary catheter was left in situ according to our institutional protocol and was removed after 24 hours. Intra-operative, post-delivery emetic episodes were recorded by direct questioning. Nausea was defined as a subjectively unpleasant sensation associated with awareness of the urge to vomit; retching was defined as the laboured, spasmodic, rhythmic contractions of the respiratory muscles without the expulsion of gastric contents: vomiting was defined as forceful expulsion of gastric contents from the mouth. They were assessed according to the Bellville’s score (5) (o=NO nausea 1=retching, 2=retching and 3=vomiting) Metoclopromide long was administrated as rescue antiemetic with the occurrence of two or more emetic episodes. The details of any other adverse events due o the study drug were recorded. The neonate was evaluated using the neurologic and adaptive capacity score (NACS) within 30 minutes after delivery and at 2 hours of age. The pre determined sample size was chosen by using power analysis based on the assumption that, the incidence of no emetic symptoms or signs (which will be considered as the primary end point) in patients receiving placebo will be 40%. An improvement front 40 to 75% will be considered as clinical importance with α=0.05 and β=0.2. The analysis showed that 30 patients per group will be sufficient. The duration of study was (June-2018 to July-2020) two years
Statistical analysis: To compare the incidence of emetic symptoms of three groups ANOVA test was applied, Episodes of emetic symptoms of emetics, in evidences of adverse intra-operatic events were classified with percentage. The statistical analysis was carried out in SPSS software
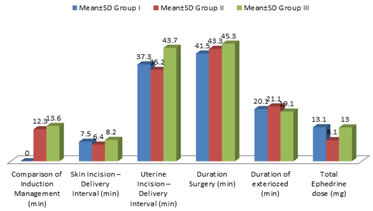
OBSERVATION AND RESULTS Table 1: Comparison of Mean parameters among study groups in operative management
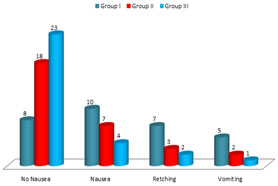
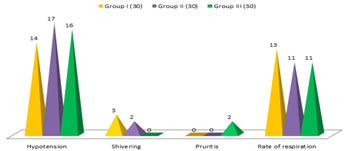
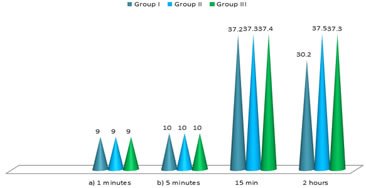
Table 2: Classification of patients as per their Emetic Episodes No Nausea 8 (8.8%) in group-I, 18 (20%) in group-II, 23 (25.5%) in group-III, Nausea– 10 (11.1%) in group-I, 7 (7.7%0 in group-II, 4 (4.4%) in group-III Retching – 7 (7.7%) in group-I, 3 (3.3%) in group-II, 2 (2.2%) in group-III Vomiting – 5 (5.5%0 in group-I, 2 (2.2%0 in group-II, 1 (1.1%) in group-III Table 3: Comparison of adverse intro-operative events Hypotension – 14 (15.5%0 in group-I, 17 (18.8%) in group-II, 16 (17.7%) in group-III Shivering – 3 (3.3%) in group-I, 2 (2.2%) in group-II, 0% in group-III Pruritis – 0% in group-I and II, 2 (2.2%) in group-III Rate of respiration – 13 in group-I, 11 in group-II, 11 in group-III Table 4: Apgar score (a) 9 (8-10) in group-I, 9 (6-10) in group-II, 9 (7-10) in group-III in 1 minute (b) 10 (9-10) in group-I, 10 (7-10) in group-II, 10 (8-10) in group-III in 5 minutes NACS scores – 15 minutes – 37.2±1.11 in group-I, 37.3±1.2 in group-II, 37.4±1.3 in group 4 – In – 2 hours – 38.2±1.1 in group-I, 37.5±1.3 in group-II, 37.3±2.0 in group-III
Table 1: Comparison of mean parameters among study groups in operative management (Total No. of patients: 90)
Table 1: Comparison of mean parameters among study groups in operative management
Table 2: Classification of patients according to their emetic episodes (Total No. of patients: 90)
Table 2: Classification of patients according to their emetic episodes
Table 3: Comparison of adverse into operative events (Total No of patients: 90)
Table 3: Comparison of adverse into operative events
Table 4: Neonatal effects (Total No of patients: 90)
NACS = Neurologic and Adaptive capacity scoring Table 4: Neonatal effects DISCUSSION Present study of Intra thecal fentanyl and midazolam for the prevention of nausea and vomiting during the caesarean delivery under spinal anaesthesia in Andhra Pradesh population. In the comparative study of mean parameters among three groups.
In the classification of patients according to their Emetic episodes No Nausea– 8 (8.8%) group-I, 18 (20%) group-II, 23 (25.5%) in group-III Nausea– 10 (11.1%) in group-I, 7 (7.7%) in group-II, 4 (4.4%) in group-III Retching – 7 (7.7%0 in group-I, 3 (3.3%) in group-II, 2 (2.2%) in group-III Vomiting – 5 (5.5%) in group-I, 2 (2.2%) in group-II, 1 (1.1%) in vomiting (Table-2) In the comparison of adverse intra-operative events –
In neonatal effects – apgar scores NACS score were quite normal (Table-4). These findings are more or less agreement with previous studies5,6,7. It is reported that, administration of combination of drugs intrathecally targets different spinal receptors resulting in prolonged and superior quality of analgesia especially in midazolam 2mg or fentanyl 10 mcg given intrathecally8,9. It was also observed that incidences of hypotension as common complication intrathecal fentanyl 20 mcg. Nausea and vomiting were reported as high incidence in placebo (group-I 75%) 40% in group II (40%) (in midazolam) 25% in group-III (in fentanyl) hence modazolam or fentanyl significantly minimize the nausea and vomiting episodes in caesarean deliver10 but shivering was higher in midazulam as compare to fentany group but higher in placebo group (11). Intrathecal midazolam or fentanyl has prolonged duration of analgesia and prolonged motor and sensory block without any significant hemodynamic compromise.
SUMMARY AND CONCLUSION In the present study of all three groups co-administration of fentanyl 12.5 mg or intrathecal midazolam 2 mg with 0.5% hyperbaric bupivacaine in the sub-arachnoid injectable to avoid intra-operative discomfort during peritoneal fraction and exteriorsation of uterus and there by reduces intra-operative and early post-delivery nausea and vomiting. There was no any significant change in hemodynamic status and side effects in any group including placebo.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home