|
Table of Content - Volume 17 Issue 2 - February 2021
A comparative study of efficacy of oral clonidine and oral pregabalin before induction on rate pressure product
Irukulla Avanthi1, Karri Laxmi Priyanka2*
1Assistant Professor, Department of Anaesthesia, Kamineni Institute of Medical Sciences Sreepuram, Narketpally, Nalgonda District, Telangana State, INDIA. 2Assistant Professor, Department of Anaesthesia, Kamineni Academy of Medical Sciences and Research Centre, Lb Nagar, Hyderabad, Telangana- 500068, INDIA. Email: priyacheez@gmail.com
Abstract Background: Airway instrumentation by direct laryngoscopy and tracheal manipulation are powerful noxious stimuli causing adverse hemodynamic responses. In general pregabalin is used in patients with normal blood pressure undergoing operation for controlling the response of the pressor in nature. There are few studies which have been carried out to study efficacy of pregabalin and clonidine in controlling responses to instrumentation of the airway in patients with controlled hypertension. Aim: A comparative study of efficacy of oral clonidine and oral pregabalin before induction on rate pressure product. Material and Methods: A total of 60 patients undergoing elective surgery were selected. Thorough pre anaesthetic evaluation was done for all the patients. Group C. Tab CLONIDINE (0.3mg) and Group P : Tab PREGABALIN (150mg) received drugs 60 minutes before the expected time of induction of anaesthesia. Baseline, Pre induction, Post induction at 1,3,5 and 10 minutes and post extubation SBP, DBP, MAP, HR were recorded. Results: There was no statistically significant difference between the two groups in baseline and preinduction readings. Whereas there was statistically significant difference between the two groups (p value =0.002) post induction. After intubation there was rise in mean rate pressure product in Pregabalin group. Also, At 1 minute (p value <0.001), at 3 minutes (p value = 0.005), at 5 minutes (p value = 0.009), at 10 minutes (p value = 0.014), there was significant difference between mean rate pressure product of two groups Conclusion: Clonidine was found to be more effective than Pregabalin in lowering of blood pressure and heart rate changes associated with laryngoscopy and endotracheal intubation. Keywords: Clonidine, Pregabalin, Rate pressure product, Efficacy.
INTRODUCTION Laryngoscopy and endotracheal intubation are routine procedures of modern balanced general anesthesia technique. Forbes and Dally (1970) described the circulatory response to laryngeal and tracheal stimulation following laryngoscopy and tracheal intubation as reflex sympathoadrenal stimulation2. Although increase in heart rate and blood pressure due to sympathoadrenal response is short lived they may have detrimental effects in high risk patients especially those with cardiovascular diseases, increased intracranial pressure or anomalies of cerebral vessels3. Clonidine suppresses induced central noradrenergic hyperactivity to attenuate reflex cardiovascular response to tracheal intubation and to improve stability during surgery4. Clonidine premedication is to produce sedation and blunt the stress response to intubation. Pregabalin acts by decreasing the synthesis of neurotransmitter glutamate to act on the central nervous system and possess analgesic, anticonvulsant and anxiolytic activity5. It was observed that it attenuates pre-operative anxiety and stress response to intubation. But, there are very few randomized controlled trials to prove the same. Hence the present study is undertaken to compare oral pregabalin with oral clonidine on blunting haemodynamic stress response to laryngoscopy and endotracheal intubation during general anaesthesia.
MATERIAL AND METHODS Present clinical study was conducted in Kamineni Institute of Medical Sciences, Narketpally, Nalgonda District, Telangana state. After approval from the hospital ethics committee, study was conducted during the period between October 2016 and September 2018. It was a prospective study. A total of 60 patients undergoing elective surgery were selected. Inclusion Criteria
Exclusion Criteria
A total of 60 patients were divided into two groups of 30 each, group C (clonidine), and group P (pregabalin). Thorough pre anesthetic evaluation was done for all the patients. Written, valid informed consent was obtained both for conduct of study as well as for surgery and anesthesia. Patients were kept nil by mouth from midnight before surgery and Tab. Alprazolam (0.25 mg) was administered. Nil per oral status confirmed in the morning and patient’s baseline Systolic blood pressure (SBP), Diastolic blood pressure (DBP) and heart rate were recorded. During this period, 60 patients were selected. They were divided into two groups : GROUP C (n=30): Tab CLONIDINE 0.3mg. GROUP P (n=30): Tab PREGABALIN 150mg. Both groups received drugs 60 minutes before the expected time of induction of anaesthesia. Anaesthetic Technique Patients in each group received respective drugs as per timing and dose mentioned earlier. On arrival in the operating room, patient’s basal parameters- Heart Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MBP), Rate Pressure Product (RPP) are monitored using, pulse oximetry, non-invasive blood pressure (NIBP).Intravenous access using 18G cannula was established and an IV infusion of ringer lactate was started. All patients were pre oxygenated with 100% oxygen for 3 minutes before induction with a tight fitting face mask. All the patients were premedicated with intra venous metoclopramide 10mg, Glycopyrrolate 0.2 mg, and Fentanyl 2mcg/kg.After preoxygenation, patients in each group was induced with thiopentone sodium 5mg/kg IV slowly till the loss of eyelash reflex. This was followed by Vecuronium bromide 0.1mg/kg IV.Patient’s lungs were manually ventilated with 100% oxygen before orotracheal intubation. Direct laryngoscopy performed after 3 minutes by using appropriate sized Macintosh blade and tracheal intubation performed within 15 seconds using appropriate cuffed endotracheal tube. Cases where more than one attempt at laryngoscopy was made were excluded from the study. The patients lungs was mechanically ventilated with tidal volume 6-8ml/kg and respiratory rate of 12/minute to maintain end tidal PaCo2 at around 30-35 mm of hg.Anaesthesia was maintained with Oxygen 33%, Nitrous Oxide 66% and Isoflurane 1% on controlled ventilation. Muscle relaxant was given in intermittent doses of Vecuronium Bromide and supplemental analgesia intravenous fentanyl 1mcg/kg was given. All the parameters of the study was recorded at the following stages. • Preoperative(baseline) • On arrival in the operating room(preinduction) • Post induction • Immediately after induction • At 1 minute, 3 minute, 5 minute, 10 minutes after induction. At the end of surgery reversal was given with Glycopyrrolate 10 µg/kg IV and Neostigmine 0.05 mg/kg IV. Extubation done when the patient was completely awake and shifted to the recovery room. SBP, DBP, MAP, HR were recorded post extubation. Any untoward effects related to the drug and Anaesthesia were noted and attended to appropriately. A fall in mean blood pressure by 30% from the baseline was treated with Ephedrine 6 mg boluses. A fall in the heart rate less than 40/min was treated with Inj Atropine 0.6 mg. analgesia if deemed necessary was supplemented with Inj Fentanyl 1µg/kg IV. Patients were followed up postoperatively at hourly basis till 8 hours from drug administration. Any untoward effects were observed for noted and treated.
STATISTICAL ANALYSIS Univariate analysis of change in these parameters at baseline, after premedication, after induction, during intubation, and at 1, 3, 5 and 10 minutes after intubation are carried out by paired t-tests for within the group comparisons. The probability of error and a value less than 0.05 is considered statistically significant. RESULTS Table 1 : Comparison Of Mean Rate Pressure Product (Mean±SD) Between Groups (N=60)
p value < 0.05 – significant.
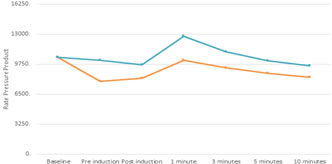
Graph 1: Comparison of mean rate pressure product between groups
Baseline: There was no statistically significant difference between the two groups (p value = 0.92). Pre induction: There was no statistically significant difference between the two groups (p value =0.08). Post induction: There was statistically significant difference between the two groups (p value =0.002). After Intubation: There was rise in mean rate pressure product in Pregabalin group. At 1 minute, there was significant difference between mean rate pressure product of two groups (p value <0.001). In Pregabalin group 21% rise from the baseline compared to 2.8% fall from baseline in clonidine group. At 3 minutes, there was significant difference between mean rate pressure product of two groups (p value = 0.005). At 5 minutes, there was significant difference between mean rate pressure product of two groups (p value = 0.009). At 10 minutes, there was significant difference between mean rate pressure product of two groups (p value = 0.014). Electrocardiogram: No ST-T changes were observed in ECG of any the patients throughout the study period. No arrhythmias were noted in any of the patients throughout the study period. SpO2: Spo2 was maintained 98% and above in all the patients.
DISCUSSION Induction of general Anaesthesia, direct laryngoscopy and endotracheal intubation induce marked cardiovascular changes as well as autonomic reflex activity6.The response may be particularly hazardous for patients with cerebral and cardiovascular diseases7. Attenuation of these haemodynamic responses is of great importance in prevention of peri-operative morbidity and mortality. Variation of heart rate changes decrease with increasing age. Young patients show more extreme changes8. Marked fluctuations in haemodynamic response are often seen in geriatric patients9,10. In this study, we selected an optimal age range of 18 to 50 years. Patients on antihypertensive drugs may exhibit a decrease in pressor response. We excluded the patients on antihypertensive medications from our study. A variable combination of drugs used for premedication, induction, relaxation and maintenance of anaesthesia can influence the sympathetic response to laryngoscopy and intubation. Premedication with benzodiazepines has no effect on sympathetic response to laryngoscopy and intubation. Glycopyrrolate premedication can be moderately increase the heart rate. IV Metoclopramide is used as premedication as anti-emetic for the prevention of post-operative nausea and vomiting. Thiopentone was selected for induction since it still continues to be the most popular agent for induction. In normovolemic patients’ Thiopentone 5mg/kg i.v transiently decrease 10-20mm Hg of blood pressure and increase the heart rate by 15-20 beats/min. There was an increase in catecholamine levels, both nor adrenaline and adrenaline10. Vecuronium a non-depolarizing neuromuscular blocking agent was used in this study which is devoid of cardiovascular side-effects at the generally used doses11. Within the last decade, several studies have reported the successful use of oral Clonidine premedication to prevent hyper adrenergic and hyper dynamic cardiovascular responses to endotracheal intubation12. Pregabalin had been shown to be effective in neuropathic pain, diabetic neuropathy, acute post-operative pain and reducing the postoperative opioid requirements. Till now not many studies have been done on pregabalin premedication to attenuate the pressor response to tracheal intubation13. However, there are not many studies comparing oral Clonidine and oral Pregabalin premedication prior to induction of anaesthesia. The present study was aimed to investigate the effect of clonidine and pregabalin on the changes in blood pressure and heart rate observed during laryngoscopy and tracheal intubation. The present study was done in 60 patients under ASA Grade I and II. The purpose of conducting this study in healthy patients was to generate data to be used in a future study in those with a history or risks of coronary artery disease with ST-T monitoring in whom beneficial effects of clonidine and pregabalin are likely to outweigh adverse effects. There were no differences between the two groups regarding demographic profile like age, sex and weight. Rate Pressure Product Rate pressure product (RPP) is a derived parameter, calculated as product of heart rate and systolic blood pressure. RPP = HR X SBP It is also called Robinson Index. It is a major determinant of cardiac oxygen consumption. Therefore in cardiac patients it is not only necessary to decrease the blood pressure but also the heart rate; so as to reduce myocardial oxygen consumption (MVO2). In patients with angina pectoris there is described relation of heart rate and systolic blood pressure to the onset of pain. Roy et.al (1979)14 found that RPP more than 22,000 was associated with changes in ECG in healthy volunteers. It was found that in patients with heart disease coming for stress test, the critical limit of RPP for angina to appear was 12,000. However, Bedford (1980)15 found RPP above 20,000 without changes in mild hypertensive patients. Results from the study of Gobel et al (1978)16 indicate that HR X BP, are valid predictors of MVO2 during exercise in a population of men with heart disease and is therefore the critical one in defining the response of the coronary circulation to myocardial metabolic demands. Both Gobel et.al (1978)16 (in awake, normal subjects) and Bailer et.al (1980)17 (in awake patients with coronary disease) have reported close correlations of RPP and MVO2. Siegelova et.al (2000)18 concluded that RPP (24-hour profile) correlates well with incidence of myocardial infarction and sudden cardiac death. They also concluded that blood pressure and RPP may be appropriate tools for optimal strategies for anti-hypertensive therapy as well as for prognosis. Laryngoscopy and endotracheal intubation increases systemic blood pressure, heart rate, cardiac work and myocardial oxygen requirement. The healthy heart may be able to sustain the demand for oxygen by increased cardiac output and coronary vasodilatation whereas these effects may be detrimental in patients with coronary insufficiency and other cardiac diseases. In the present study, after laryngoscopy and endotracheal intubation, there was a rise in RPP in Pregabalin group. Maximum rise in RPP was noticed at 1 minute after intubation, i.e. 12766±2727 (21.59% increases over baseline) in Pregabalin group, 10171.9±1832.78 (2.8% decreases from baseline) in Clonidine group. RPP was subsequently declined to 9551.53±2018.89 and 8325.25±1519.45 in Pregabalin and Clonidine groups respectively at 10 minutes. RPP was significantly higher in Pregabalin group as compared to Clonidine group from post induction, up to 1, 3,5,10 minutes after intubation (p value<0.05). Rate pressure product (an indicator for myocardial oxygen demand) was significantly less in Clonidine group after intubation at 1, 3, 5,10 minutes during the study period (p value<0.05) when compared to Pregabalin group. Attenuation of maximum rise in rate pressure product by clonidine is evident and statistically highly significant when compared with Pregabalin.
CONCLUSION Clonidine was found to be more effective than Pregabalin in lowering of blood pressure and heart rate changes associated with laryngoscopy and endotracheal intubation. Pregabalin gives better postoperative analgesia, more sedation and less bradycardia as compared to Clonidine.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home