|
Table of Content - Volume 18 Issue 1 - April 2021
Subarachnoid versus intravenous clonidine for minimizing stress response in laparoscopic surgeries under general anaesthesia
Sonali A Joshi1, Daisy S Gajjar2*, Divyang V Shah3
1Assistant Professor, 2Post Graduate IIIrd Year Resident, 3Professor & HOD, Department of Anaesthesiology, Surat Municipal Institute of Medical Education And Research (SMIMER), Surat, Gujarat, 395010, INDIA. Email: daisyghayal26@gmail.com
Abstract Background: Clonidine has come up as an interesting premedication desirable in laprascopic surgery wherein significant hemodynamic stress response is seen. These changes are characterized by increase in arterial pressure, systemic and pulmonary vascular resistance seen early after the beginning of intra-abdominal insufflation with smaller change in heart rate. Clonidine is a selective alpha-2-adrenegic agonist well known to inhibit cathecholamine release. Clonidine has been used via different routes to suppress the hemodynamic stress responses associated with capnoperitoneum. Aim: The aim was to compare the effect of equal doses of intrathecal (IT) and intravenous (IV) clonidine in maintaining hemodynamic stability during capnoperitoneum under general anaesthesia. Methodology: A randomized controlled study was done in 76 patients of either sex, with ASA grade 1 and2, aged between 18 to 55, posted for laprascopic surgeries. Group C-IV(n=38) patients received 1 mcg/kg i.v. clonidine 15 minutes before induction. Group C-IT(n=38) patients received the same dose intrathecally just before induction. Intraoperative hemodynamic parameters, post-operative pain and sedation were assessed. Patients who required nitroglycerine (NTG) to keep mean arterial pressure (MAP) below 20% of baseline were noted. Result: Intraoperative heart rate; systolic, diastolic and mean arterial blood pressures at intubation, pneumoperitoneum and extubation were significantly reduced in group C-IT compared to group C-IV. Rescue analgesia was less required in Group C-IT compared to Group C-IV in first two hours after surgery. There was no statistically significant difference in the sedation score between both groups. Conclusion: IT clonidine is more effective than IV clonidine in suppressing hemodynamic stress response to capnoperitoneum at the dose of 1 mcg/kg. Early post-operative analgesia was achieved in both IT and IV clonidine without causing much sedation. Keywords: laproscopy; physiological stress response; clonidine; spinal anaesthesia
INTRODUCTION The creation of pneumoperitoneum with carbon dioxide (co2) which causes stimulation of sympathetic nervous system leads to pathophysiological changes like increase in arterial pressure, systemic and pulmonary vascular resistance, change in heart rate are seen after carbon dioxide insufflation. Clonidine, an alpha-2-adrenoreceptor agonist, causes reduction in sympathetic outflow and induce analgesia by performing at brain, brain stem, spinal cord and peripheral nerves. Clonidine which is an imidazoline derivative, a potent antihypertensive causes reduction in the heart rate, blood pressure, systemic vascular resistance and cardiac output. clonidine increases the cardiac baroreceptor reflex sensitivity to raise systolic blood pressure, and thus stabilizes blood pressure. And it is also having several benefits like sedation, analgesia, reduction in anaesthetic drug requirement and minimizing stress response. Release of cathecholamines and vasopressin are inhibited by this drug which modulates the hemodynamic changes caused by pneumoperitoneum in laproscopic surgeries. Various routes can be used to administer clonidine like oral, intramuscular (IM), intravenous (IV), intrathecal and epidural with dose range from 1-8 mcg/kg. AIM AND OBJECTIVE The major aims of the study were to compare the intraoperative hemodynamic response to intubation, pneumoperitoneum and extubation. Primary objective was to assess the number of patients requiring NTG to maintain mean arterial pressure (MAP) within 20% of baseline. Secondary objectives were to assess the post-operative pain and sedation.
MATERIAL AND METHODS A prospective randomized study was carried out in 76 patients, aged between 18 to 55 years, of either sex, who belonged to American society of anaesthesiologists grade 1 and 2 posted for elective laproscopic general surgeries lasting less than or equal to 2 hours. patient’s refusal for spinal, laproscopic surgeries demanding steep head low or head up positions, A-V conduction block, HR<55/min, hypertensive patients, patients with contraindication to spinal anaesthesia, known allergy to clonidine were excluded from study. Patients who included in the study were kept nil by mouth for at least 6 hours and premedicated with inj glycopyrrolate 0.2mg iv and inj ondansatrone 4 mg iv. In the pre-operative holding area, before administration of study drug, baseline HR and blood pressure were recorded. In the C-IV group, in 100 ml normal saline 1 mcg/kg clonidine was given over 15 mins in the pre-operative holding area under monitoring. Patients were shifted to operation theatre after infusion and general anaesthesia was given. In the C-IT group, preservative free clonidine was given in L3-L4 intervertebral space at 1 mcg/kg (maximum 75 mcg), diluted with 1.5 ml cerebrospinal fluid (CSF) which followed general anaesthesia. In OT, electrocardiography, non-invasive blood pressure, pulse oximetry, temperature, end tidal CO2, TOF for neuromuscular blockade were started and baseline cardio-respiratory parameters were noted. Patients were pre-oxygenated with 100% oxygen for 3 mins, induced with inj fentanyl 2 mcg/kg, inj propofol 2 mcg/kg and inj. Vecuronium 0.1 mcg/kg. when TOF count was 0, tracheal intubation was done. After conformation of tracheal tube placement, intermittent positive pressure ventilation was given with 8 ml/kg tidal volume. Fresh gas flow with O2, N2O ratio of 50:50 and 1.5% concentration of isoflurane. Isoflurane was adjusted to achieve minimum alveolar concentration (MAC) of 1.0 throughout surgery and not altered based on hemodynamics. Intra-abdominal pressure (IAP) was maintained at 12 mm hg during laprocopy. Hemodynamic parameters were recorded at baseline, at premedication, induction, endotracheal intubation, pneumoperitoneum, after pneumoperitoneum (30 min) and extubation. When TOF count was 2, intermittent boluses of inj vecuronium 0.02 mg/kg was administered. Inj fentanyl 0.02 mcg/kg repeated hourly. An increase in MAP beyond 20% of baseline value was treated with NTG infusion 0.3µg/kg/min and titrated with 0.1µg/kg/min increments every 5mins till it was within limits. Any fall in systolic blood pressure (SBP) below 80mmHg or MAP below 60mmHg, was treated with 3mg boluses of mephenteramine. Once initiated, NTG was tapered and stopped only when MAP fell below the baseline MAP level. A decrease in HR to less than 50/min was treated with 0.3mg of i.v. atropine. When TOF count was 2, reversal of neuromuscular blockade was done at the end of the surgery. Tracheal extubation was done after adequate respiration, muscle power and tone.Patient’s sedation scores were noted according to Ramsay sedation scores at pre-induction and during postoperative period. Ramsay Sedation Scale is as given below
Pain were assessed on 10 point visual analogue score (VAS) at the end of surgery at 30 min.,60 min., 90 min. and 120 min. Patients were observed in the post-operative room till VAS score of 4. Rescue analgesia in the form of injection Diclofenac sodium 75 mg IV first and inj. Tramadol 2mg/kg IV was given as second line of analgesic. Figure 1: OBSERVATION AND RESULTS Data was expressed as mean and standard deviation. The homogenecity in 2 groups of mean and standard deviation was analysed using MS excel. Comparisons amongst the groups were done using student- T test. A ‘p value’ of less than or equal to 0.05 was considered as statistically ‘significant’. There were no significant differences between the two groups with regard to demographic data such as age, sex, ASA grade, duration of pneumoperitoneum and duration of surgery (Table 1).
TABLE 1: Demographic data
Table-2 shows comparison of heart rate in 2 groups of patients, significant difference was seen throughout the intraoperative period except for baseline and at the time of premedication values, where there was no significant difference. In group C-IV, heart rate was significantly higher at intubation and extubation (100.3 ± 7.52 and 101 ± 7.18 respectively).
Table 2: shows perioperative mean heart rate (beats/min) among 2 groups
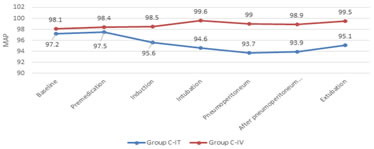
Figure 1: Heart rate (Beats/Minutes) Table-3 shows comparison of mean arterial pressure between 2 groups, significant variation was observed throughout the intraoperative period except for the baseline and before induction values where there was no significant difference. In group C-IV mean arterial pressure was significantly higher at intubation, pneumoperitoneum and at extubation (99.6 ± 4.69, 99.0 ± 5.47 and 99.5 ± 3.27).
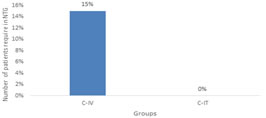
Figure 2: Percentage of patients requiring NTG between two groups In group C-IV, total 6 patients out of 38 required NTG (15%) than the patients of group C-IT. There was a statistically significant difference in number of patients who required NTG between group C-IT and group C-IV.
Table 3: changes in mean arterial pressure (MAP) in two groups
Figure 3: Trends of mean arterial pressure
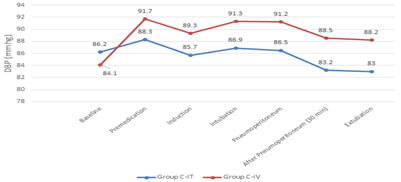
Table-4 suggestive of systolic arterial pressure was higher in group C-IV significantly at intubation, pneumoperitoneum and at extubation (except baseline, at premedication values). After pneumoperitoneum, no episode of hypotension was found in any of the groups. Table 4: changes in systolic arterial pressure in two groups
Figure 4: Trend of systolic blood pressure table-5 shows diastolic arterial pressure was significantly higher in group C-IV.
Table 5: changes in diastolic arterial pressure in two groups
Figure 5: Trends of diastolic blood pressure
At the end of the surgery, the mean VAS of group C-IT differed and lower significantly as compared to group C-IV in the early first two hours of surgery according to table-6.
Table 6: shows postoperative VAS score amongst 2 groups in first 2 hours of surgery
Significantly a smaller number of patients in group C-IT required rescue analgesia than group C-IV. The demand for rescue analgesia was 50% on group C-IV and 22% in group C-IT in the first two hours of surgery. All the patients were either ‘awake and comfortable’ or ‘asle ep and arousable’. All our patients were awake within first 1 hour of surgery. There is no statistically significant difference in the sedation score between groups. (p=0.352). No patients were deeply sedated at the extubation. (table-7)
Table 7: shows the mean difference of ramsay sedation score among 2 groups
DISCUSSION The anaesthetic technique for abdominal laparoscopic surgery is generally limited to general anaesthesia with neuromuscular blockade, tracheal intubation, and mechanical ventilation. Pneumoperitoneum during laparoscopic surgery leads to significant hemodynamic changes such as an increase in MAP and systemic vascular resistance (SVR) and a decrease in cardiac output. The decline in cardiac output and venous return can be attenuated by volume infusion before pneumoperitoneum. Increased intra-abdominal pressure due to insufflation of gas may compress venous capacitance vessels causing an initial increase followed by a sustained decrease in preload as venous return decreases, while arterial compression may increase after-load and systemic vascular resistance.11 Joris et al.12 found a 35% increase in mean arterial pressure, a 65% increase in systemic vascular resistance, a 90% increase in pulmonary vascular resistance, while there was a 20% decrease in cardiac output at intrabdominal pressure of 15 mm hg. Ishizaki et al.13 tried to determine the safe range of intra-abdominal pressures during laparoscopic surgery. At 16 mm Hg of intraabdominal pressure, significant fall in cardiac output was observed. However, at 12 mm Hg of intra-abdominal pressure, hemodynamic alterations were not observed. During laparoscopy, intra-abdominal pressure should be as low as possible as per current guidelines. In this present study, mean intra-abdominal pressure was maintained at 12 mm Hg throughout the duration of surgery. Pharmacological agents like β-blocker, opioids, increasing concentration of inhalational anaesthetic agents, nitroglycerine, and α-2 adrenergic agonist have been used to minimize these hemodynamic derangements during laparoscopy with varied results. Clonidine, with an elimination half life of 6 to 10 hours, is a centrally acting selective partial α - agonist. It is known to induce sedation, decrease anesthetic drug requirement and improve perioperative hemodynamics by decreasing blood pressure and heart rate responses to surgical stimulation, and protecting against perioperative myocardial ischemia.7 Clonidine can be administered via various routes – oral, intramuscular, intravenous, epidural, intrathecal etc. In our study, we have avoided the use of local anaesthetics through spinal route to prevent motor blockade thereby helping in early ambulation of the patients. Therefore, combination of two anaesthesia techniques was chosen to add to their advantages and limit the side effects of a drug and making it useful in a day care surgery in this study. Kalra et al. used clonidine 1 µg/kg intravenously over a period of 15 minutes before pneumoperitoneum and clonidine group patients showed significantly better hemodynamic control than control group.7 However, higher doses of clonidine resulted in significant bradycardia and hypotension. While R sripriya et al. showed that patients were hemodynamically more stable in C-IT group than C-IV and control group.4 In our study, we observed that the mean of HR, SBP, DBP and MAP were better with intrathecal clonidine for pneumoperitoneum. Filos et al. compared 150, 300 and 450µg IT clonidine as a sole agent for post op analgesia following caesarean section and observed a decrease in MAP of more than 20% from baseline with 150µg clonidine.2 We have not observed any hypotension in our study with 1µg/kg IT clonidine. This can be due to our patients being introduced to a surgical stress and capnoperitoneum that countered the vasodilating properties of clonidine or due to the smaller dose of clonidine used. IT clonidine is commonly used as an adjuvant to spinal local anaesthetics to prolong the duration of analgesia. Only Filos et al. have used IT clonidine as a sole analgesic for post op analgesia in caesarean section patients and they observed a dose dependent increase in duration of analgesia lasting for 402 ± 75, 570 ± 76 and 864 ± 80mins when 150, 300 and 450 µg were used. They have demonstrated that less clonidine is needed IT than systemically to produce strong analgesic effect lasting for longer duration.2 We observed that IT clonidine provides good early postoperative analgesia as the number of patients who required rescue analgesia was less in group C-IT compared to the other group. Although a smaller number of patients in C-IT group required rescue analgesia, the difference was not statistically significant. R sripriya et al. discussed that demand for rescue analgesia was higher in group N and in group C-IV as compared to group C-IT in the first two hours,4 which is in favour of this study. The number of patients requiring NTG in study done by R sripriya et al. was 16% in group C-IV,0 patients in the group C-IT and 36% patients in the control group.4 No patient required NTG to maintain MAP within 20 % of baseline in group C-IT with 1 mcg/kg dose in our study. This proved, 1 mcg/kg intrathecal clonidine could achieve hemodynamic stability throughout intraoperative period than 1 mcg/ kg intravenous clonidine. VAS score was better achieved with intrathecal clonidine (1 mcg/ kg) than intravenous clonidine (1 mcg/kg) as observed in our study. According to Surekha C et al., the duration of postoperative analgesia is significantly greater in Group CL (10.30 ± 1.24 hours) in comparison to Group CF (5.53 ± 1.11 hours).5 Tripathi et al. have also observed that even with 2µg/kg of i.v. clonidine, none of their patients were deeply sedated.1 R sripriya et al. studied that no patients were deeply sedated at extubation in any of the group.4 In our study, both treatment groups were having no statistically significant difference which proved that none of the route of clonidine prolong recovery.
CONCLUSION 1 mcg/kg intrathecal clonidine provides better hemodynamics during carbon dioxide insufflation and maintainance of pneumoperitoneum than an equal dose of intravenous clonidine in patients undergoing laproscopic surgeries under general anaesthesia. Both of the routes provide early postoperative analgesia. None of the routes causes delayed recovery or deep sedation.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home