|
Table of Content - Volume 18 Issue 1 - April 2021
A comparative study of efficacy of ketamine - propofol admixture and lignocaine - propofol admixture in reducing propofol injection pain in paediatric patients
K K Jadhav1, S B Patil2*
1,2Associate Professor, Department of Anaesthesiology, B.K.L.Walawalkar Rural Medical College, Sawarde, INDIA. Email: dockashi@gmail.com
Abstract Background: Normally Lignocaine is used either as a pre- treatment or Lignocaine – Propofol admixture is used to reduce the Propofol injection pain. Ketamine though a commonly used drug, only a few studies have been conducted to study the effectiveness of Ketamine in reducing the Propofol injection pain in pediatrics. Hence the present study was undertaken to assess and compare the effectiveness of i.v. Ketamine-Propofol admixture with i.v. Lignocaine-Propofol admixture in reducing Propofol injection pain in paediatric patients. Objectives - To compare the analgesic efficacy of Ketamine – Propofol admixture and Lignocaine-Propofol admixture in reducing Propofol injection pain in paediatric patients. Material Methods - A randomised double blind study was conducted in 70 children of age 1-10 years with ASA grade I or II. A informed written consent was taken from parents/ guardians of all the children. The Institutional Ethical committee approval was taken. The block randomisation method was used. Group K patients received i.v. Ketamine 1mg/ml in Propofol 10mg/ml admixture while Group L patients were injected with i.v. Lignocaine 1mg/ml in Propofol 10mg/ml admixture. After giving 25% of the calculated dose of Propofol 10 sec pause was taken during which the pain of Propofol injection was assessed using a Three point scale. Later the remaining dose of Propofol was injected. The sample size was calculated with alpha error of 0.05 and 80% power of study. Statistical analysis was done using unpaired student t - test and Chi Square test (p value <0.05). Result - The incidence of no pain was 54.28% in Ketamine group and 45.71% in Lignocaine group. The incidence of moderate and severe pain in Ketamine group was 22.85% each and in Lignocaine group was 28.57% and 25.71% respectively. Conclusion - Ketamine-Propofol admixture is as effective as Lignocaine- Propofol admixture in reducing Propofol injection pain in pediatric patients. Keywords: Injection pain, Ketamine, Lignocaine, Pediatric, Propofol,
INTRODUCTION Propofol is a widely used drug for procedural sedation. It is considered very effective and safe in adults as well as paediatric patients too.1,2 One of its major side effect is pain on injection and less frequently hypotension.3 The incidence of pain on Propofol injection is around 28-90%.4 But the incidence and severity of Propofol pain is reported significantly higher in young children.5 Normally Lignocaine is used either as a pre- treatment or Lignocaine – Propofol admixture is used to reduce this pain. There are a few studies which proved that Ketamine is significantly effective in reducing the Propofol injection pain as compared to Lignocaine in adults.6,7 Ketamine is most commonly used drug in paediatric anaesthesia because of its analgesic effect and preservation of airway reflexes. But only a few studies have been conducted to study the effectiveness of Ketamine in reducing the Propofol injection pain in paediatric patients and moreover their findings are also contradictory. Hence the present study was undertaken to study the effectiveness of Ketamine-Propofol admixture in preventing Propofol injection pain. Aim: The aim of this study was to assess and compare the effectiveness of intravenous ( i.v.) Ketamine-Propofol admixture with i.v. Lignocaine-Propofol admixture in reducing Propofol injection pain in paediatric patients. Objectives: The primary objective was to compare the analgesic efficacy of i.v. Ketamine – Propofol admixture with i.v. Lignocaine-Propofol admixture in reducing Propofol injection pain by three point pain score in paediatric patients. The secondary objective was to look for any adverse events like hypotension, hypertension, desaturation and laryngospasm.
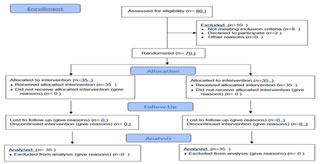
MATERIALS AND METHODS A randomised double blind study was conducted in 70 children of age 1-10 years posted for lower abdominal surgeries under sedation with caudal anaesthesia from June 2019 to December 2020 in a tertiary care hospital. Inclusion criteria – Children posted for lower abdominal surgeries like Inguinal Hernioplasty, Undesended testis, Circumcision, Hypospadias repair requiring sedation with caudal anaesthesia having ASA grade I and II. Exclusion criteria - Children of American Society of Anaesthesiologist (ASA) grade IIIand IV, patients with fever, airway obstruction, allergic to Propofol, Ketamine or Lignocaine. A well informed written consent was taken from the parents/ guardians of all the children. The approval from The Ethical committee of Institution was taken. All the patients were kept nil by mouth (2 hrs for liquids and 6 hrs for solids) before surgery and received i.v. Glycopyrolate 0.004mg/kg as premedication pre - operatively. Local anaesthetic cream (EMLA) was applied on the site of i.v. line insertion and after an hour; 22 guage i.v. line was inserted. Patients were then taken to the operating theatre where standard ASA monitoring like ECG, pulseoximeter, non-invasive blood pressure monitor were connected to the patient. Later the allotment of the group was done under the vigilance of one of the researcher by block randomisation method. If the patient belonged to Group K he received i.v. Ketamine 1mg/ml in Propofol 10mg/ml admixture while Group L patients were injected with i.v. Lignocaine 1mg/ml in Propofol 10mg/ml admixture. The respective Propofol admixtures were given for over 10 sec by the other researcher until the loss of eyelash reflex. After the 25% of the calculated dose of Propofol had been given,10 sec pause was taken during which another observer who was blinded to the study groups, assessed the pain of Propofol injection using a Three point scale. Later the remaining dose of Propofol was injected. Pain of Propofol injection was defined by using Three point scale.8
Table 1: Three point scale to assess Pain of Propofol injection
Hemodynamic parameters like mean arterial pressure (MAP), heart rate were monitored. Any hypotension( decrease in MAP ˃20 % of baseline), hypertension (increase in MAP˃20 % of baseline) or any adverse events like laryngospasm, desaturation (Spo2<92 %) were noted. Later on caudal anaesthesia was given in lateral position at the rate of 0.5ml/kg volume using 0.25% Bupivacaine. The sample size was calculated using data from Fahringer et al study which estimated 66% incidence of Propofol pain with alpha error of 0.05 and 80% power of study.9 The calculated minimum sample size was 29 in each group but for the possibility of dropouts we included 35 patients in each group. The statistical analysis was done using Microsoft Excel 2010 Software. Unpaired student t - test was used for comparing quantitative variables while Chi Square Test was used to compare qualitative variables. P value <0.05 was considered significant.
RESULTS Table 2 shows the demographic characteristics of the patients included in the study. Both the groups were comparable. Table 3 – 19 out of 35 patients in the K group (54.28%) while 16 out of 35 patients in L group (45.71%) experienced no Propofol injection pain. While the incidence of moderate and severe pain in K group was 22.85% each as compared to the incidence of 28.57% of moderate pain and 25.71% of severe pain in L group patients. On analysis by Chi- square test, to compare the results in both the groups, showed no statistical significance. Table 4 - There was no incidence of hypotension, hypertension or desaturation event in both the groups but two children in L group had laryngospasm. Table 2: Demographic Characteristics
Table 3: Propofol injection Pain Score (chi square test)
Table 4: Incidence of Adverse outcomes
Figure 1: CONSORT flow diagram
Figure 2: Propofol injection pain score in both the groups
DISCUSSION This randomized double blind study was conducted on 70 paediatric patients with demographic characteristics as mentioned in Table 2. Only paediatric patients with ASA grade I and II, posted for lower abdominal surgeries requiring sedation with caudal anaesthesia were included in the study. We found that 54.28% children in K (Ketamine-Propofol admixture) group and 45.71% in L (Lignocaine-Propofol) group were free from Propofol injection pain while the incidence of moderate and severe pain in K group was 22.85% each as compared to the incidence of 28.57% of moderate pain and 25.71% of severe pain in L group patients. Though the difference in efficacy of both the admixtures in reducing the Propofol injection pain was not statistically significant the percentage incidence of patients with no pain was increased with Ketamine-Propofol admixture as compared to Lignocaine-Propofol admixture. Moreover the percentage incidence of moderate and severe pain experienced by the patients on Propofol injection was also less in K group as compared to L group. No adverse events like hypotension, hypertension, desaturation or laryngospasm was seen in K group whereas 2 children out of 35 in L group had laryngospasm. (Table 3 and4) Fig 2. In contrary to our results, Kaabachi et al. in their study found that Ketamine-Propofol admixture was significantly less effective in reducing Propofol injection pain than Lignocaine-Propofol admixture in children aged 1-12 years.10 They found that the incidence of pain in Ketamine group was 45% whereas it was only 22% in Lignocaine group. But they too reported an adverse event of laryngospasm in 1 patient in Lignocaine group. Our results showed some similarities with Barbi et al. study where they compared pretreatment with Ketamine and Lignocaine Propofol admixture in reducing Propofol injection pain. They concluded that only 8.1% patients in Ketamine group experienced pain as compared to 38.7% patients in Lignocaine group. Hence they too concluded that pain experienced by the patients was less in Ketamine group as compared to Lignocaine group. The enhanced effectiveness of Ketamine in their study was, may be due to the difference in dose of Ketamine administered. Barbi et al. used a dose of 0.5 mg/kg of Ketamine which is approximately double the dose we used in our study ie.0.2 mg/kg.8 CH Tan et al. in their study found 26% incidence of pain in Ketamine group while Suzuki et al. in their study observed 33% of incidence of pain in Ketamine group in adults. But in both these studies they used pretreatment of Ketamine in adults while we studied the efficacy of Ketamine-Propofol admixture in pediatric patients.7,6 Hence according to our findings, Ketamine Propofol admixture can be effectively used in reducing Propofol injection pain The possible reason for the effectiveness of Ketamine to reduce Propofol injection pain, may be due to its NMDA receptor antagonist action on vascular endothelium, We used 0.2 mg/kg dose of Ketamine which is very low dose for its central analgesic action, hence it is its peripheral action that is contributing in reducing Propofol injection pain. Another possible reason as suggested by Hwang et al. study is the change in pH of Propofol injection due to addition of Ketamine. The pH of 1% Propofol is 7.86 while the pH of 1% Propofol-Ketamine admixture is 5.84 which contributes in reducing the Propofol injection pain.11 Moreover Propofol-Ketamine admixture showed statistically similar efficacy as Propofol –Lignocaine admixture in reducing Propofol injection pain without causing any adverse events. Further studies need to be conducted to find the minimum effective dose of Ketamine to increase its efficiency.
CONCLUSION Ketamine-Propofol admixture is as effective as Lignocaine Propofol admixture in reducing propofol injection pain. But Ketamine is safe, affordable and easily available; hence it can be used as an alternative to Lignocaine in reducing Propofol injection pain in children.
ACKNOWLEDGEMENT We are very thankful to the children and their parents/gaurdians for their immense co-operation and support towards the successful completion of this study.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home