|
Table of Content - Volume 18 Issue 1 - April 2021
Comparative evaluation of levobupivacaine and levobupivacaine with dexemedetomidine in transeversus abdominis plane block for caesarean delivery for post-operative analgesia: Randomised prospective study
Bhavika Ogariwala1*, Dipika Patel2, Divyang Shah3
1IIIrd Year Resident, 2Assistant Professor, 3Professor & HOD, Department of Anaesthesia, Surat Municipal Institute of Medical Education and Research, Surat, INDIA. Email: bhavikaogariwala@gmail.com
Abstract Background: The transversus abdominis plane (TAP) block is a regional anaesthetic technique that provides analgesia to the parietal peritoneum as well as the skin and muscles of the anterior abdominal wall (T6-L1 dermatomal area). An adjuvant like dexmedetomidine has been used to prolong duration of local anaesthetics in TAP block. We aimed to compare duration of postoperative analgesia when TAP block with levobupivacaine with or without dexmedetomidine was given following caesarean delivery under spinal anaesthesia. Methods: 54 patients were randomized into 2 different groups to receive TAP block following caesarean delivery under spinal anaesthesia (group A, group B). Group A received bilateral TAP block with 18 ml 0.25% levobupivacaine with 2ml normal saline on each side, while Group B received TAP block with same volume of levobupivacaine with 0.5µg/ kg of dexmedetomidine diluted in 2ml of normal saline after taking informed consent. Results: The duration of postoperative analgesia using visual analogue score was significantly higher in group B as compared to group A. Time to first rescue analgesia was long in Group B as compared to A. Name of statistical test: Chi-square test and Independent t-test. Conclusion: Bilateral TAP block with 0.25% levobupivacaine provides good quality analgesia for early postoperative period. Adding dexmedetomidine further improves pain control and gives higher patient satisfaction without any added side effects. Keywords: Levobupivacaine hydrochloride, Dexmedetomidine, Bupivacaine heavy, Tramadol hydrochloride, Post-operative pain
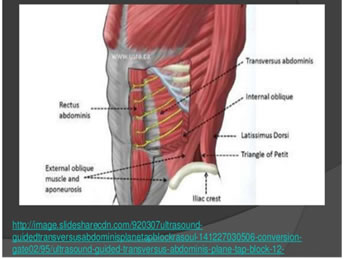
INTRODUCTION Lower section caesarean section is extensively done under spinal anaesthesia. Pain after caesarean section is moderate to severe experienced by most of patients and failure to provide adequate analgesia may affect care of baby, breastfeeding, mother-baby bonding, risk for thrombo-embolism as a result of immobility due to pain. Pain of caesarean section has somatic component (from abdominal wall incision) and visceral component (from the uterus). The postoperative analgesia should be adequate as well as safe for the breastfeeding baby, and can be provided by systemic (IV / Oral), regional analgesic technique or multimodal analgesia. Systemic opioids have side effects like nausea, vomiting, pruritus, sedation, urinary retention and respiratory depression. Regional analgesic techniques have minimum systemic side effects as drug’s site of action is peripheral. The transversus abdominis plane (TAP) block is a regional anaesthesia technique that provides analgesia to the parietal peritoneum as well as the skin and muscles of the anterior abdominal wall. (T6-L1 dermatomal area). In TAP block, local anaesthetic is given into an anatomical space between the internal oblique and transversus abdominis muscles where the anterior branches of thoracolumbar nerves originating from T6 to L1 are located. Local anaesthetics such as bupivacaine, ropivacaine, levobupivacaine is used. Levo-isomers have less systemic toxicity than the racemic compounds. Addition of adjuvants to local anaesthetics prolongs the duration of analgesia. Dexmedetomidine, a selective alpha2 adrenergic agonist is an adjuvant most commonly used in the regional techniques and causes sedation, analgesia without any delirium, or respiratory depression. The mechanism of action is unique and differs from those of currently used agents, including clonidine. This study was done to compare the efficacy of transversus abdominis plane block with levobupivacaine 0.25% versus levobupivacaine 0.25% and dexmedetomidine 0.5 mcg/kg using landmark technique for post-operative analgesia following lower segment caesarean section.
AIMS AND OBJECTIVES To compare Dexmedetomidine as an adjuvant to levobupivacaine and levobupivacaine alone in TAP block. Assessment of postoperative analgesia. Duration of analgesia. Need for first rescue analgesia. MATERIALS AND METHODS The randomized prospective study was conducted among the patients posted for Caesarean delivery admitted to SMIMER hospital, Surat. Adult parturients undergoing caesarean section was divided in two group.
Each patient was assessed at 0, 4, 8, 12, 24 hour after surgery by an independent observer for pain at rest and on movement using visual analogue scale, time of first demand for tramadol, satisfaction with pain management and side-effects.
INCLUSION CRITERIA: ASA physical status I and II requiring elective or non-urgent caesarean (where no fetal or maternal compromise existed). EXCLUSION CRITERIA: Patient’s refusal. Patients of <50 kg or >100 kg weight was excluded from the study. Patients with any contraindication to spinal anaesthesia. Patients who was allergic to local anaesthetic and study drugs. Patients who was unable to understand visual analogue score.
Figure 1: Anatomy
POST-OPERATIVE ASSESSMENT Pain was assessed by VAS score. Time of first request for Postoperative analgesia when VAS≥4. When VAS≥4 Inj Tramadol 50 mg iv was given and that time was calculated as total Duration of analgesia. Side effects like allergy, nausea, vomiting, bradycardia and hypotension were noted. VAS Score Figure 2
VISUAL ANALOGUE SCALE 0--------------------2--------------------4-------------------6--------------------8--------------------10 None annoying uncomfortable dreadful horrible agonizing
OBSERVATION AND RESULTS After studying 54 cases, observation and results were summarized in tabulated form and described below. Both groups comprised of 27 patients. Demographic Profile Table 1:
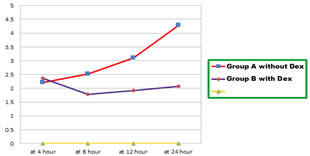
No significant difference seen in age, weight and duration of surgery among both groups. All the patients observed among both groups were under ASA grade I/II. Comparison of pulse and blood pressure in both groups Pulse and blood pressure of patients were comparable in both groups. Among which no significant difference was observed in either groups for pulse, SBP, DBP at respective pre-operative, intra-operative, post-operative, immediately after TAP block, at 4 hour, at 8 hour, at 12 hour, and at 24 hour. Post-operative VAS score at rest and on movement (mean SD) Comparison of VAS score AT REST in both study groups Pain score (VAS) at rest, at 4 hours, 8 hours, 12 hours, 24 hours timeline expressed as mean ± SD
Table 2:
Figure 3:
Comparison of VAS score AT MOVEMENT in both study groups Pain score (VAS) at movement, at 4 hours, 8 hours, 12 hours, 24 hours timeline expressed as mean (SD)
Table 3:
Figure 4: During first 4 hour, no statistical difference was observed in both groups, but after that Pain scores at rest and at movements were lower in patients who received TAP block with levobupivacaine with dexmedetomidine(Groups B) as compared to patients who received TAP block with levobupivacaine alone (Group A).
Total duration of post operative Analgesia supplement and time of first rescue analgesia in mins (mean SD)
Table 4:
Figure 5: Comparison of total duration of Post-operative analgesia in both study groups Time for first rescue of analgesia and total duration of postoperative analgesia were significantly longer in patients who received TAP block with Levobupivacaine with dexmedetomidine (Groups B) as compared to patients who received TAP block with levobupivacaine alone (Group A).
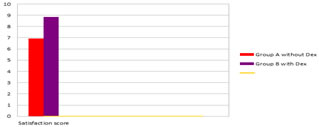
Patient satisfaction score (mean SD) at 24 hours Table 5
Figure 6: Comparison of patient Satisfaction score in both groups Patient satisfaction scores were significantly higher in patients who received TAP block with levobupivacaine with dexmedetomidine (Groups B) as compared to as compared to patients who received TAP block with levobupivacaine alone (Group A).
DISCUSSION The transversus abdominis plane (TAP) block is a simple, effective, rapidly expanding analgesic technique which significantly reduces pain associated with lower abdominal surgery where parietal pain is a significant component of postoperative pain. It involves a single large bolus injection of local anaesthetic into the TAP, an anatomical space between the internal oblique and transversus abdominis muscles. The local anaesthetic agents in TAP block provides excellent analgesia to the skin and musculature of the anterior abdominal wall. In present study, we compared Levobupivacaine and levobupivacaine with dexemedetomidine in transeversus abdominis plane block for caesarean delivery for postoperative analgesia. The prolonged duration of analgesia after TAP block may be related to the fact that transversus abdominis plane is relatively poorly vascularized, so drug clearance may be slow by reduction of absorption in to the blood stream and less risk of systemic toxicity from the local anaesthetics [2]. In this study we demonstrated that by giving bilateral TAP block with 20 ml of 0.25% levobupivacaine with 0.5µg/kg dexmedetomidine on each side in patients undergoing caesarean section, reduced pain score postoperatively and also decreased requirements of postoperative analgesia as compared to patients received bilateral TAP block with same volume of levobupivacaine alone. Various adjuvants have been used to improve the quality and the onset of action of local anaesthetic action in different regional block techniques. Dexmedetomidine, a highly selective, alpha-2-adrenergic receptor (α2-AR) agonist, used by anaesthetists in many anaesthetic techniques due to its hemodynamic-stabilizing properties and sedative, analgesic, and sympatholytic effects to local anaesthetic action. Individual patient characteristics such as age, gender, and body weight are important factors influencing any pharmacologic therapy. All the demographic parameters were comparable in both the groups and there was no statistically significant difference between two groups (p value > 0.05). The mean duration of surgery in Group A was 53.18 ± 5.18 min and 52.51 ± 4.70 min in Group B, which was comparable in both the groups in our study. There was no statistically significant difference regarding duration of surgery in both the groups (p value > 0.05). In present study, hemodynamic parameters observed were mean pulse rate, mean systolic blood pressure, mean diastolic blood pressure. No significant difference was observed in both the groups (p value > 0.05). This study correlate with P. Raghunath et al.3 , Aman Varshney et al.. [1] , in 2015 Abdelaal et al.4 studies suggesting that no significance difference found in mean pulse rate, mean systolic blood pressure, mean diastolic blood pressure. Postoperative pain assessment was done by Visual Analogue Scale (VAS) score for 24 hours. In our study, In Group A, mean VAS score at rest appeared to rise from the 9th hour and at movements appeared to rise from the 7th hour, while in Group B, mean VAS score at rest remained < 3 at 24thhour and at movements appeared to rise from the 15th hour postoperatively. There was statistically highly significant difference in postoperative mean VAS score between both the groups postoperatively (p value > 0.001). Xiao F, Liu L, Xu W, et al.6 conducted a study titled “Dexmedetomidine can extend the duration of analgesia of levobupivacaine in transversus abdominis plane block”. Patients in the Control group (n = 30) received TAP block, using 40 mL of 0.25% levobupivacaine, and patients in the Dexmedetomidine group (Dex group) received the same volume and concentration of levobupivacaine but with additional 0.5 µg/kg of dexmedetomidine for TAP block. The VAS point at rest was significantly lower in the Dex group than in the Control group at 8 and 12 hours (P < 0.05). The patient satisfaction with postoperative analgesia in the Dex group was better than in the Control group (P = 0.006). The duration of analgesia was significantly longer in the Dex group than in the Control group (905.0 ± 114.2 min vs. 741.4 ± 105.3 min, P < 0.001). Our study data is consistent with this study. Almarakbi WA, Kaki AM14 conducted a study titled “Addition of dexmedetomidine to bupivacaine in transversus abdominis plane block potentiates post-operative pain relief among abdominal hysterectomy patients”. They observed that addition of dexmedetomidine to bupivacaine in TAP block had significantly lower VAS score at rest and at movement which is consistent with our study. In our study, the mean time for first rescue analgesia in Group A was 522.62 ± 53.24 min (⁓8.7 hr) and in Group B was 977.40 ± 57.80 min (⁓16.2 hr) which was statistically high significant difference (p value < 0.05), with longest in Group B. We added dexmedetomidine in TAP block as adjuvant to levobupivacaine to prolonged the postoperative analgesia duration and we found that addition of dexmedetomidine prolonged the duration of request of first rescue analgesia. Abdelaal et al.4in 2015 done comparative study between levobupivacaine versus levobupivacaine plus dexmedetomidine for TAP in postoperative pain management after abdominoplasty. In total of 69 patients, they reported dexmedetomidine (Group M) and levobupivacaine (Group L) group had significant lower pain score as compared to control group. They observed that dexmedetomidine (Group M) and levobupivacaine (Group L) group had significant less consumption of meperidine in comparison to C group with significance of P < 0.001. Postoperatively 24 h total meperidine consumption in M group was less than in L group P < 0.01. Addition of dexmedetomidine in TAP block as an adjuvant prolonged duration of postoperative analgesia which is correlated with our study. Aman Varshney et al.1 conducted a study titled TAP block with levobupivacaine versus levobupivacaine with dexmedetomidine for postoperative analgesia following cesarean delivery. The time for the first request of analgesia was significantly longer in group D (TAP block with 20 cc 0.25% levobupivacaine +1µg/kg dexmedetomidine on each side) as compared to group L (TAP block with 20 cc 0.25% levobupivacaine on each side) and control group (no TAP block). They observed that addition of dexmedetomidine prolongs the effect till 12 hours which is correlated with our study. P. Raghunath et al.3 conducted a study to compare ropivacaine versus levobupivacaine in TAP for postoperative analgesia in patients undergoing lower abdominal surgeries. Duration of postoperative analgesia in TAP block with 0.25% levobupivacaine was 419.6±49.95 minutes and in TAP block with 0.5% ropivacaine was 2140.6±511.12 minutes (p<0.05). The study data is consistent with our data. Loane et al.16 found that the use of TAP block did not provide analgesia in comparison with “100 µg morphine” intrathecally in the first 24 h and require higher analgesic consumption due to higher pain score. Costello and colleagues 15, these investigators found no analgesic benefit from TAP block using ropivacaine 20 ml 0.375 % per side in patients undergoing caesarean section under spinal anaesthesia This is due to TAP block was performed as blind technique. We and them did not use ultrasound to visualize the anatomy, we cannot guarantee
Limitation: Plasma levels of dexmedetomidine were not monitored. The time at which the TAP block began to work could not be differentiated. The time at which the sensory effect of the intrathecal block began to wear off could not be clearly differentiated.
CONCLUSION Bilateral TAP block with 0.25% levobupivacaine provides good quality analgesia for early postoperative period. Adding dexmedetomidine further improves pain control and gives higher patient satisfaction without any added side effects.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home