|
Table of Content - Volume 18 Issue 1 - April 2021
Comparison of success rate of inguinal approach versus classical pubic approach for obturator nerve block in patients undergoing trans-urethral resection of bladder tumours
Carolin Von Mullai A¹, Mohamed Shahid H²*, Sivabalan³
1Senior Assistant Professor, ³Assistant Professor, Department of Anaesthesiology, Institute of Anaesthesiology and Critical Care, RGGGH, Madras Medical College, Chennai, Tamil Nadu, INDIA. ²Assistant Professor, Department of Anaesthesiology, Government Vellore Medical College, Vellore, Tamil Nadu, INDIA. Email: mullai.md@gmail.com
Abstract Background: Transurethral resection of bladder tumour (TURBT) is usually carried out under spinal anaesthesia. During electrical resection of the lateral wall mass, violent adductor contractions may occur and lead to bladder perforation. Therefore, obturator nerve block (ONB) is mandatorily followed after spinal anaesthesia to avoid this complication. Aim of the study: Comparing the success rate and efficacy of an inguinal approach with pubic approach for ONB using nerve stimulator. Methods: Sixty patients who required ONB undergoing TURBT with spinal anaesthesia were included in this study. After spinal anaesthesia, ONB was performed with inguinal approach (Group I, n = 30) or pubic approach (Group P, n = 30) using a nerve stimulator. If the adductor contraction had not occurred by the 3rd attempt, it was defined as a failed block. Number of attempts, needle depth, performance time, success rate and the presence of adductor contraction during operation were evaluated. Results: The success rate of ONB was higher in group I compared to group P (90% vs. 73.3%, P = 0.0067). The required needle depth was lower in group I than in group P (3.00 cm vs. 6.04). The performance time was quicker in group P compared to group I (3.96 minutes vs, 2.45 minutes, P=0.006). There is no significant difference in the number of attempts. Conclusions: The inguinal approach for ONB appears to be technically easier and offers certain anatomical advantages compared to the pubic approach which is quicker to achieve. Key words: Inguinal approach, Obturator nerve block, TURBT
INTRODUCTION Urinary bladder mass resections are commonly performed under subarachnoid block which offers many advantages such as technical ease of performing the procedure, reduced risk of bleeding, and early recognition of bladder perforation. The only shortcoming with subarachnoid block is sparing of the obturator nerve with a potential complication of bladder rupture or injury secondary to adductor muscle contraction from obturator nerve stimulation (obturator reflex) during transurethral resection of bladder tumour (TURBT)1 TURBT is widely used surgical technique for both diagnosis and treatment of bladder cancer. This surgery cannot be carried out effectively due to sparing of obturator nerve which courses on the lateral wall of bladder where it can be easily get stimulated by the electrical current passed through the loop during resection with an intense involuntary response from adductors (adductor longus, brevis, magnus, gracilis) and external rotation (obturator externus) of hip.2,3 Adductor jerk or obturator reflex is associated with a serious injury such as vessel wall laceration with profuse bleeding, bladder wall tear or perforation, and even incomplete resection due to frequent distractions and interruptions to the operating surgeon.6 The obturator nerve is derived from the 3rd to 4th lumbar nerves with a minor contribution from L2.4 The obturator nerve along with vessels pass from pelvic cavity where it runs close to prostatic urethra, bladder neck, and inferolateral bladder wall and exit to thigh through a canal where it can be easily blocked.5 The obturator nerve block was first applied by Gaston Labat in the year 1922. Much of the works in obturator nerve block followed a few years later when Gaston Labat and Victor Pauchet, stated that obturator nerve block combined with blocks of the sciatic and femoral nerves provided complete anesthesia of the entire lower limb. With the introduction of modern nerve stimulators and ultrasound guidance selective block of the obturator nerve has become more reliable and successful.5,7 Selective obturator nerve block has also been used in the diagnosis and treatment of chronic pain states secondary to knee arthrosis or pelvic tumours resistant to conventional analgesic approaches. In this study, we compared the success rate of the inguinal and pubic approach in Obturator nerve block using a nerve stimulator under spinal anaesthesia for transurethral resection of bladder lateral wall tumours.
METHODS After obtaining the institutional ethics committee approval and written informed consent, sixty patients of ASA physical status I, II or III undergoing elective Transurethral Resection of Bladder tumour were included in this study. Patients belonging to age group 30 to 70 years of both the sex were included in this prospective, randomized, double blinded clinical study which was completed over a period of 6 months. This study was done in the Institute of anaesthesiology and Critical care, Madras Medical College, Chennai Patients were excluded from the study if they refused, had advanced cardiac and respiratory insufficiency, allergy to local anaesthetics, pre-existing neurologic deficits, skin infections involving pubic area, prior surgeries involving the hip and the inguinal region and bleeding tendency. Obturator nerve block was performed in the patients in whom the block was needed. Most of this was demanded by urologists because of invasive lateral bladder wall tumour. And these patients were randomly allocated to the conventional pubic approach group (Group P) or new inguinal approach group (Group I). On arrival to the operating room, standard anaesthetic monitors were applied and 0.9% normal saline 300 ml was given intravenously. A spinal block was performed with a 25G Quincke’s needle at the L3-4 or L4-5 interspace. After confirming free flow and clear CSF, 0.5% hyperbaric bupivacaine was administered to attain desired level of block, accordingly. In a supine position, sympathetic and sensory blocks were checked with an alcohol swab and pin-prick test. When the sensory level block reached above T12, obturator nerve block was performed according to group assignment. All obturator nerve block were performed by 2 investigators separately for both the approaches and they were not involved in further treatment of those patients. obturator nerve block was performed using a nerve stimulator (Medilogix Inc. Nerve stimulator, 18 G Braun Teflon insulated needle). Nerve stimulation was applied using a current of 0.5 mA at 1 Hz only. Obturator nerve block Pubic approach: The patient was placed in a supine position with the legs slightly abducted and externally rotated. After identification of the pubic tubercle, a needle was inserted perpendicularly to the skin 1.5 cm lateral and 1.5 cm inferior to the tubercle. When the needle made contact with the inferior border of the superior pubic ramus, the needle was withdrawn short of the tip and then slipped along the anterior pubic wall. After this, the needle was redirected anteriorly or posteriorly and slightly withdrawn again and advanced cephalically and laterally at an angle of 45 degrees until contraction of the thigh adductor muscles were observed. When the adductor muscle was contracted, 10 ml of 1% lignocaine was administered after confirmation so that no blood was present after negative aspiration. If there were no responses of adductor muscles after the third attempt, 15 ml of 1% lignocaine was instilled evenly and the needle was withdrawn and this was defined as a failed obturator nerve block.
Inguinal approach: The patient was placed in a supine position with the legs slightly abducted and a line marked the inguinal crease. After identification of the adductor longus tendon in the medial part of the thigh, a mark on the skin was made in the inguinal crease at the midpoint of the line drawn between the femoral arterial pulse and the inner border of the adductor longus tendon. This approach was performed in 2 stages. First, the needle was inserted 0.5 cm below the mark in the cephalad direction with a 30 degree angle to the skin until adductor muscle (adductor longus or gracilis) contractions were elicited. After identification of the contractions (anterior side of the inner thigh and the medial part of the knee), 5 ml of 1% lignocaine dose was administered (anterior branch block). Then the needle was advanced deeper about 0.5-1 cm and 5 degrees laterally. When the contraction of the adductor magnus muscle occurred (i.e. noticeable hip adduction), 5 ml of 1% lignocaine was injected (posterior branch block). If there were no contractions of the adductor muscles after the third attempt, 15 ml of lignocaine was instilled evenly and this was defined as a failed obturator nerve block. Also, if the obturator sign occurs during the procedure, in cases with successful adductor contraction in the obturator nerve block, that case was defined as a failed case. The number of needle attempts, the needle depth, performance time were recorded. An independent observer who was blinded to the approach evaluated the obturator signs during surgery. We planned to administer a general anaesthesia with laryngeal mask airway (LMA) when the obturator sign occurred during surgery. Statistical analysis The collected data were analysed with IBM.SPSS statistics software 23.0 Version. To describe about the data descriptive statistics frequency analysis, percentage analysis were used for categorical variables and the mean and S.D were used for continuous variables. To find the significant difference between the bivariate samples in Independent groups the Unpaired sample t-test was used. To find the significance in categorical data Chi-Square test was used similarly if the expected cell frequency is less than 5 in 2×2 tables then the Fisher's Exact was used. In all the above statistical tools the probability value .05 is considered as significant level.
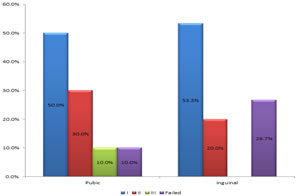
RESULTS In our study, according to the statistical analysis, the demographic variables were found to be equally distributed among the two groups and we proceeded with the comparison of other variables. Majority of the subjects in Pubic group got successful location of obturator nerve in first attempt (n=16,53.3%) compared to inguinal group (n=15,50%). P value Chi Square test 0.116. Also the number of failed attempts is higher in the pubic approach (n=8, 26.7%) compared to that of inguinal approach (n=3,10%) p value is 0.067
Figure 1: Number of attempts to group
Table 1:
There is no significant difference in the required number of attempts in achieving the obturator nerve block in both the groups. However there is significant higher failure rate in the inguinal approach.
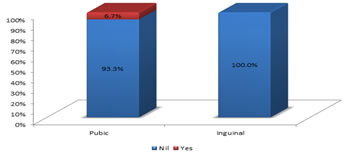
ADDUCTOR SPASM DURING SURGERY
Figure 2: Adductor spasm during surgery with groups
Table 2:
The adductor spasm occurred in 2 of the 3 failed block cases in pubic group and no spasm occurred in 8 of the failed cases in Pubic group. p value Chi square test = 0.492 The occurrence of adductor spasm is more in the pubic group compared to the inguinal group, that too occurred in failed cases of obturator nerve block.
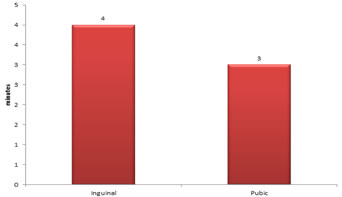
PERFORMANCE TIME Figure 3: Performance time
Table 3:
The mean block performance time in Inguinal group is 3.96 minutes compared to 2.86 minutes in Pubic group. The p value (unpaired t test) is 0.006 which is highly significant. The Obturator Nerve block can be achieved considerably earlier by inguinal approach compared to that of Pubic approach.
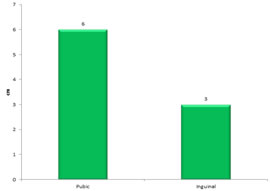
NEEDLE DEPTH Figure 4: Needle depth
Table 4:
The mean needle depth in Pubic approach is 6.04 cm compared to 3.00 cm in inguinal group. p value unpaired t test is 0.0005. The Obturator nerve is identified at a superficial level in Pubic area and can be identified relatively easier according to our study. Table 5:
DISCUSSION In this study we have compared the success rate of two approaches for obturator nerve block using nerve stimulator. The results of our study show that the block can be achieved in a reasonably quicker time (2.45 minutes versus 3.96 minutes) in inguinal approach while the success rate of achieving the block is higher in the pubic approach (failure rate inguinal 26.7% versus pubic 10.0%) During Transurethral Resection of Bladder tumour surgery, when the bladder is distended with irrigation fluid, the obturator nerve becomes very close to the lateral wall of the bladder and the electrical currents from the electrosurgical resector can stimulate the obturator nerve which leads to violent contraction of adductor muscles of the thigh.2,8 Venkatramani et al.9 compared monopolar with bipolar cauterization for TURBT and concluded that bipolar TURBT was not superior to unipolar TURBT with respect to obturator jerk, bladder perforation, and hemostasis are concerned. Gupta et al.10 eliminated nerve stimulation with the use of current of power as low as 50 W and 40 W for cutting and coagulation, but these settings have been reported to be too low for satisfactory resection. Obturator nerve block combined with subarachnoid anaesthesia can only be an effective modality in the TURBT which can easily be accomplished. Various methods have been described in literature to block obturator nerve. Prentiss et al.2 and later Parks and Kennedy described nerve stimulation technique with a success rate between 83.8% and 85.7%. More recent studies have reported that the use of sonography is associated with higher success rates of 97.2% in ultrasound-guided obturator nerve block procedures. This is technically more advanced than nerve stimulation technique. Though advanced ultrasonographical identification of obturator nerve is available, a blind anatomical approach using a nerve stimulator has been widely used. According to Augspurger and Donohue,1 effectiveness of abolishing obturator jerk with blind anatomic approach was 83.8% which is lower than nerve stimulation and ultrasound-guided techniques. As per Gasparich et al.5 and Kobayashi et al. with nerve stimulation, the effectiveness reaches between 89.4% and 100%. Although various methods have been used in an effort to increase the success rate of obturator nerve block, a blind approach using nerve stimulators is still a common technique. With the available clinical data, the success rate of obturator nerve block with the classical pubic method varies from 60.5% to 91.7%. A study evaluated the Interadductor approach to obturator nerve blockade for spastic conditions of adductor thigh muscles.11 It evaluated the efficacy of the block achieved in terms of its success rate, the degree of alleviation of muscle spasm, the improvement of gait in the patients with multiple sclerosis, and the facilitation of nursing hygienic care in bedridden patients. The study concluded that the interadductor approach is a new approach based on the anatomy of the obturator nerve trunk, which, though in the obturator canal, is shielded by its osseous part from the anteroposterior perspective of the traditional approach. The interadductor approach allows needle positioning inside the obturator canal through a mediolateral perspective, thus facilitating the blockade of the obturator nerve trunk before it branches immediately outside the canal. The new approach was successful. Another study by Yutaka Taira et al.10 compared the interadductor approach of obturator nerve block with the traditional approach in terms of the insertion-adductor contraction interval (ICI), success rate and completion of the block. The ICI with the interadductor approach was significantly shorter than that with the traditional approach. The success rate, completion of the block, and plasma lignocaine concentrations were similar with both approaches. The interadductor approach can provide faster identification of the obturator nerve than the traditional approach. In our study none of the complications related to Obturator nerve block has occurred, even though a safe approach is mandatory with this technique to avoid the damage to surrounding structures and vessels. In comparison, the inguinal approach is performed at a safer distance from the pelvis and the major vessels. Thus, this technique minimizes the risk of the complications and allows compression in the case of hematoma. We have defined a block as successful when any adductor muscle contraction occurred within the third needle attempt and the adductor contraction did not occur during the surgical procedure. A study Compared inguinal approach with classical pubic approach for obturator nerve block and concluded that the inguinal approach for obturator nerve block appeared to be technically easier and offered certain anatomical advantages when compared to the pubic approach.15Motor neurons carry Aα fibers which are thicker in diameter. For an effective obturator block, the local anaesthetic concentration must exceed that for pain and temperature sensations, which are carried by thin Aδ and C fiber, by 2-fold. Thus the concentration of lignocaine used must be greater than 1% for an effective motor block.13 We found out that bilateral obturator nerve block may be performed safely and effectively with 2% lignocaine 10 ml with the aid of a peripheral nerve stimulator in patients undergoing transurethral resection procedures with spinal anaesthesia. In this study, the rate of obtaining a successful block in the first attempt was 50.0% in pubic approach versus 53.3% in the inguinal approach with the p value of 0.116. This was found to be statistically insignificant. The results show that the mean needle depth of attaining the obturator nerve block is 3.00 cm for inguinal group compared to 6.04 cm in pubic group. This can be attributed to the relatively superficial anatomical location of obturator nerve in the inguinal area. In our study, the mean time for obtaining the obturator nerve block 2.45 minutes for inguinal approach compared to 3.96 minutes for pubic group with a p value of 0.006 which is statistically significant. The block failure occurred in 26.7% of the cases in inguinal group compared to 10.0% of the cases in pubic group with a p value of 0.0067 which is statistically significant. This is attributed to the availability of definitive bony landmarks in the classic pubic approach compared to the arbitrary surface anatomical landmark in the inguinal approach. The adductor muscle contraction occurred in 2 of the failed block cases in inguinal approach and in none of the cases in pubic approach with a p value of 0.492 which is statistically insignificant.
CONCLUSION The inguinal approach for obturator nerve block seems to be technically easier and offers certain anatomical advantages in comparison with the pubic approach, the classical pubic approach is more successful in providing the reliable blockade of the obturator nerve in Transurethral resection of Bladder tumours.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home