|
Table of Content - Volume 19 Issue 1 - July 2021
Comparison of post-operative analgesic efficacy of rectus sheath catheter versus continuous wound infiltration for laparotomy surgery
S Sakthi Abirami1*, G R Rajashree2
1Assistant Professor, Department of Anaesthesiology, Pondicherry Institute of Medical Sciences, Puducherry, INDIA. 2Formerly Professor - Institute of Anaesthesiology and Critical Care, Madras Medical College and Rajiv Gandhi Government General Hospital & Medical Superintendent, Government Medical College, Omandurar Government Estates, Chennai, Tamil Nadu, INDIA. Email: s.shakthi18@gmail.com
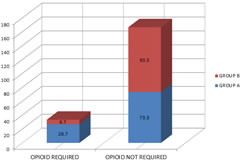
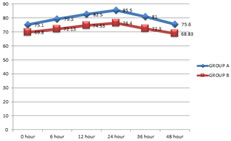
Abstract Background: The analgesic requirement of patients following laparotomy surgeries could not be met by single method. Pain, if effectively managed in the post operative period will reduce the respiratory complications, decrease the hospital stay and health care cost for the patients. Ultrasound guided rectus sheath catheter allows continuous infiltration of local anaesthetic in the post operative period. Materials and Methods: Randomised controlled trial – 60 patients who underwent Laparotomy surgery were divided into 2 groups. Group A – Bilateral wound catheter was placed subcutaneously at the end of surgery. Group B –Rectus sheath catheter was placed bilaterally under USG guidance. Both patient received bolus of 10 ml 0.25% Bupivacaine followed by infusion of 0.25% Bupivacaine at 2ml/hr for 48hrs. The hemodynamic parameters, VAS score, Post operative opioid consumption were recorded for the above mentioned period. Results: The VAS score was significantly low in Group B compared to Group A (2.2, 2.0, 1.67, 1.87, 1.7, 2.17 vs 3.93, 3.86, 3.6,3.97, 4.1, 3.8)(p <0.05) in the observed time intervals. The need for rescue analgesia with opioid was less in Group B (6.7%) compared to patients in Group A (26.7%) (p<0.05). The HR, MAP observed in Group A is increased significantly as compared to Group B at all time intervals (p<0.05). Conclusion: We concluded that USG guided Rectus sheath catheter provides better post operative analgesia in laparotomy surgeries than wound catheter infusion. Keywords: Post operative analgesia, Rectus sheath catheter, Wound catheter, Local Anaesthesia.
INTRODUCTION Effective analgesia is an integral part of postoperative management in surgical patients. The analgesic requirement of patients following laparotomy surgeries could not be met by single method. Multimodal analgesic methods were described, both intravenous and regional techniques. Each method has its own advantages and disadvantages, although all method aims to alleviate pain with minimal side effects. Off late, the use of intravenous opioids has been discouraged because of their potency to cause postoperative respiratory depression, sedation, postoperative nausea and vomiting.1 This limits the functional capacity of the patient and hence the wound healing is impaired. For the above-mentioned shortcomings, regional anaesthetic techniques were popularised. Epidural analgesia is the most widely used method of analgesia in intra – and postoperative period with a higher success rate. But in patients who are on anticoagulants or patients with anatomical spine distortion the use of epidural catheter to provide continuous analgesia is either impossible or contraindicated. Hence anaesthesia is provided by regional blocks of nerves innervating the incision site in abdominal surgeries. A continuous infusion of local anaesthetic via subcutaneously placed wound catheter has consistently shown improved analgesia in various abdominal surgeries.2 It has very low technical failure rate and less toxicity. Moreover, there is improved patient compliance with wound catheters and infection rates are not increased.3 Modified Rectus Sheath Block is in practice since 19th century. With the advent of portable Ultrasonogram machine this regional anaesthetic technique has been revolutionised. The USG provides image to localise the nerve bundles precisely, and thus avoiding the complication of like intravascular injection, local anaesthetic toxicity, damage to nerve bundles and also increases the success rate of blockade. USG guided rectus sheath block can be a single shot injection of local anaesthetic into posterior rectus sheath but the duration of analgesia is limited.4 Hence a modified rectus sheath block with catheter placement in the posterior rectus sheath allows continuous infusion of local anaesthetic in the post operative period. Unfortunately, there are limited number of studies comparing the analgesic efficacy of continuous rectus sheath catheter infusion with wound catheter infusion of local anaesthetic in midline laparotomy surgeries. We aimed to compare the analgesic efficacy of these two well known techniques of post operative analgesia.
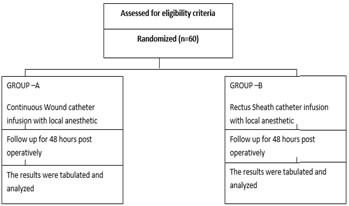
MATERIALS AND METHODS This prospective randomised control trial single blinded study was carried out in Rajiv Gandhi Government General Hospital and Madras Medical College, Chennai from September 2107 to February 2018. The study was conducted on 60 patients aged 30 – 60 years and ASA physical status I and II scheduled for elective open laparotomy surgery via midline abdominal incision. The Institutional Ethics Committee approval was obtained. A written and informed consent was obtained from each patient explaining the procedure and risks in the regional language. All the study data have been kept confidential and the results were used for scientific purpose only. Patients were excluded from study if they have coagulopathies, allergy to local anaesthetics drugs, seizures and any neurological deficit, chronic respiratory illness, renal or hepatic dysfunction. Patients who were posted for emergency surgery and had infection at block site were also excluded. 60 patients were randomised using closed envelops into 2 equal groups, each of 30 patients to receive post operative analgesia using either Rectus sheath catheter placed using an USG guidance or through subcutaneous catheter placed at the end of surgery. The participants were blinded.
Figure 1:
PREOPERATIVE:Clinical examination including airway examination was done. The following lab investigations done – complete blood count, fasting and postprandial blood sugar, Liver and Renal function tests, Prothrombin time. All patients were categorized based on American Society of Anaesthesiologists Physical Status for fitness. Patients were given premedication on the morning of surgery.INTRAOPERATIVE:Patients were connected to monitor – continuous ECG and NIBP measurements every 5 min, Oxygen saturation was done in the intraoperative period. Baseline HR, SBP, DBP, MAP and Oxygen Saturation was recorded. Preoxygenation with 100%O2 was done for 4 min. Anaesthesia was induced with Inj. Fentanyl 1 mcg/kg, Inj. Propofol 2 mg/kg followed by Inj. Atracurium 0.5 mg/kg to facilitate endotracheal intubation. Patients lung ventilated and anaesthesia was maintained with Sevoflurane 1 - 2 % and incremental doses of Inj. Atracurium 0.1 mg/kg when needed and adequate surgical relaxation achieved. Intraoperative analgesia was provided by Inj. Fentanyl 0.5 mcg/kg every 1 hour.POSTOPERATIVEAfter end of surgery according to patients group the postoperative analgesia was provided.GROUP A – Continuous Wound catheter infusion (N = 30)A multiholed catheter is placed in between the subcutaneous layer and skin on the either side of incision by the surgeon at end of surgery. Upto to 6 – 8 cm is placed inside the layer and secured to skin. Loading dose of 10 ml of 0.25% Bupivacaine is given. The catheters are then connected to infusion pump containing 0.25 % Bupivacaine. Infusion started at rate of 2 ml/hr for each side (total dose 4 ml / hr).GROUP B – Rectus Sheath Catheter infusion (N = 30)The technique was described by DJ Sanderman et al.(5). The abdomen site is cleaned with alcohol solution, draped. The probe is covered with sterile interface. The probe is placed over the skin in longitudinal orientation above the umblicus. Gently move the probe laterally to visualize the target structures – skin, subcutaneous tissue, external and internal oblique muscle, transverses abdominis muscle as well as the rectus sheath. Then 18 G Tuohy needle is introduced at an angle of 45degree to the skin just below the costal margin in an in-plane technique. The needle is advanced till it reaches the posterior rectus sheath. A bolus of normal saline was injected to ensure hydro dissection between the muscle and posterior rectus sheath. The hydro dissection is visible on the ultrasound confirming the correct position. The rectus sheath catheter is introduced through the needle into the space, 4 – 8 cm of catheter is left in space. The catheter is tunnelled laterally to avoid interference with the surgical field. The procedure is repeated on the opposite side. Analgesia was maintained with 10 ml of Inj.Bupivacaine 0.25% bolus followed by continuous infusion at 2 ml / hr on each side (total 4ml/hr)RECOVERYAfter the end of surgery and the procedure, the inhalational anaesthetics were discontinued and the muscle relaxant reversed by Inj. Neostigmine and Inj. Glycopyrollate. All patients were extubated after confirming adequacy of spontaneous ventilation. Patients were shifted to Post operative ward for observation of study parameters for 48 hours.EVALUATION Primary outcome measures – severity of pain is assessed using VAS score (0 – 10) at rest at time 0 hr, 6 hr, 12 hr, 24 hr, 36 hr, 48 hr. If VAS > 4 patient received titrated dose of Inj. Fentanyl 1-2 mcg/ kg. The dose was stopped if RR < 12/ min and SpO2 < 95%. The postoperative opioid consumption was recorded. Secondary outcome measure – Heart Rate, Mean Arterial Pressure, Opioid consumption was recorded at time of 0 hr, 6 hr, 12 hr, 24 hr, 36 hr, 48hr postoperatively.
STATISTICAL ANALYSIS All data were entered to Microsoft Excel 2010 and later these spreadsheets were used for analysis. Statistical analysis was done using SPSS version 20.0. Quantative data like age, weight, duration of anaesthesia, HR and MAP were analysed using independent t-test for comparison between two groups and expressed as mean ± SD. The non parametric data like VAS at rest were analyzed using Mann-Whitney U test for comparison between two groups. Sex, number of patients who needed supplemental injection and complications were expressed as number %. P < 0.05 was considered statistically significant.
RESULTS There was no statistical difference between groups with respect to age, sex, weight, ASA PS classification and duration of surgery. In Group B, the mean VAS score was 2.2, 2.0, 1.67, 1.87, 1.7, 2.17 in 0 hr, 6 hr, 12 hr, 24 hr, 36 hr, 48hrpost operative period respectively. In Group A the mean VAS score was 3.93, 3.86, 3.6, 3.97, 4.10, 3.8 in the observation period. This shows that the Rectus sheath Catheter group had a better analgesia in postoperative period and p value was <0.05 in all the observed time period.
TABLE 1: RESULTS OF PRIMARY OUTCOME
RESULTS OF SECONDARY OUTCOME The mean heart rate was significantly higher in Group A compared to Group B in all the observed time period.
Table 2
The MAP was significantly lower in Group B compared to Group A in the observed post operative time period as indicated by p < 0 Table 3
The number of patients requiring opioid is higher in Group A than in Group B.
Table 3:
Figure 2: VAS SCORE Figure 3: COMPARISON OF MEAN HEART RATE
Figure 4: COMPARISON OF MAP DISCUSSION The Rectus sheath block although an older method is redefined by the advent of portable USG machines. In this study we demonstrated that Continuous infusion of Local Anaesthetics via rectus sheath catheter provides superior analgesia than wound catheter infusion. The hemodynamic parameters were lower in rectus sheath catheter group in all the observed time period. The opioid requirements were also minimised significantly during the first 48 hours of post operative period. The technique of Ultrasound Guided Rectus Sheath Block was studied by Sanderman J. David et al.5. In this study 13 – 6 MHz linear array probe was used to define the rectus sheath space and catheter was placed after dissection of space with distilled water. The Ultrasound guided technique resulted in higher block success rates, shorter onset time for blocked and the total dose of local anaesthetic required was less. The assessment of local anaesthetic spread was studied and reduced complication was reported. Needle insertion was directly visualised and hence plane of block was accurate. We used a similar technique as described in this study for guiding the catheter. Alsheed et al.6 studied the case series of Ultrasound – guided rectus sheath block in children for umblical hernia repair. They observed that there was no increase in hemodynamics recorded both intraoperatively and postoperatively following an ultrasound guided rectus sheath block and none of the patient required additional opioids. We were able to produce similar results with this study in adult population with a rectus sheath catheter and continuous infusion of Local anaesthetic. MK Shah et al.7 studied the analgesic efficacy of ultrasound- guided modified rectus sheath block compared with wound infiltration on the basis of postoperative morphine consumption. This study concluded that Ultrasound – guided Modified Rectus Sheath Block does not show any significant change in morphine consumption in 24 hr postoperative period as compared to Wound infiltration in patients undergoing hysterectomy via pfannenstiel incision. This study was done as a single shot injection of local anaesthetic in the immediate postoperative period. But in our study, we placed a catheter and continuous infusion was given for 48 hrs post operative period. We were able to show a better analgesic efficacy, as evidenced by better hemodynamic parmeters and less consumption of opioids in patients undergoing midline laparotomy surgeries. AR Godden et al.8 studied the analgesic efficacy of Ultrasonography guided rectus sheath catheters versus epidural analgesia for open colorectal cancer surgery in a single centre. The study concluded that Epidural Analgesia was associated with higher incidence of hypotension than the Rectus sheath catheter group although the efficacy of pain relief was similar with both the groups. There was no change in other postoperative complications like respiratory tract infection, anastomotic leak and wound related complications. Bashandy et al.9 conducted a study on reducing Postoperative opioid consumption by adding an Ultrasound – guided Rectus Sheath block to multimodal analgesia for abdominal cancer surgery with midline incision. It was observed that the VAS score was lower in Rectus sheath block group compared with General Anaesthesia group. The morphine consumption was lower in rectus sheath catheter group throughout 48 hours of postoperative period.
CONCLUSION In summary, local anaesthetic infiltration of Ultrasound guided Rectus sheath catheter provides a better analgesic efficacy than wound catheter infiltration for 48hrs post operatively in patients undergoing midline laparotomy surgeries. The opioid consumption can be minimised by this technique. This helps to eliminate the complications associated with opioid consumption in the post operative period.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home