|
Table of Content - Volume 19 Issue 3 - September 2021
The effect of perioperative esmolol infusion on the postoperative pain and nausea vomiting after middle ear surgeries
Payal P Adhiya1*, Vandana Parmar2, Vrinda Oza3*, Feny Thakkar4
1Senior Resident, 2Professor and HOD, 3,4Assistant Professor, Department of Anaesthesiology, P.D.U Medical College and Hospital, Rajkot, INDIA. Email: ppadhiya93@gmail.com
Abstract Background: Pain and postoperative nausea and vomiting are the most common postoperative complications in middle ear surgeries. Amongst the beta-blockers, esmolol is ultrashort acting cardio selective β1 receptor antagonist used for management of postoperative pain. It also contributes to the significant decrease in PONV and reduces patient distress and facilitates earlier discharge. Objective: To evaluate the effectiveness of perioperative esmolol infusion on postoperative pain relief and postoperative nausea vomiting after middle ear surgeries. Methods: After obtaining approval from Institution Ethics Committee, 70 patients of age 15 and 65 years of ASA I,II and III were allocated with randomization into two groups of 35 each. Group C: 30 ml normal saline loading dose and thereafter continuous infusion of 1ml/min and Group E:0.5mg/kg esmolol in 30ml NS loading dose and 30ug/kg/min as infusion. Results: Average duration of analgesia was about 535 min in group E as compared to 187 min in group C. For PONV requirement of inj. ondansetron in group E was after 145 min and in group C it was 20 min. Group E patients had significantly less variations in blood pressure and heart rate intraoperatively and the response to intubation was masked as compared to group C. Conclusion: Intraoperative esmolol infusion is a newer justified method to reduce postoperative pain and PONV with advantage of hemodynamic stability. Key Words: Esmolol, PONV, postoperative analgesia, middle ear surgeries, haemodynamics.
INTRODUCTION Pain and postoperative nausea and vomiting are the most common postoperative complications in middle ear surgeries.1 Beta-adrenergic antagonist activate G proteins in isolated cell membrane suggesting that this property of beta-blockers resemble the mechanism of central analgesia as induced by clonidine.2 Esmolol is a selective beta1 adrenergic antagonist, rapid and transient acting, has a short half-life.2 It is used for treatment of tachycardia and hypertension that occur during induction and tracheal intubation during surgery, on emergence from anaesthesia and in postoperative period. This beta-adrenergic antagonist has a sympathetic nerve blocking effect on postoperative nausea, vomiting and pain.1 The aim of the present study was to compare the effects of perioperative esmolol infusion and placebo on postoperative pain and nausea vomiting after middle ear surgeries. The objectives of our study were to assess the postoperative rescue analgesic requirement, incidence of postoperative nausea, vomiting and hemodynamic response.
MATERIAL AND METHODS After approval from Institutional Ethics Committee and written informed consent, a prospective randomized control study was conducted at P.D.U. Medical College and Hospital, Rajkot on 70 patients of ASA physical status I, IIandIII, age 15- 65 years, of either sex undergoing middle ear surgeries under general anaesthesia. Patients with cardiovascular, respiratory and renal co-morbidities; on drugs like beta blockers, salbutamol and diabetes mellitus, history of allergy and those on chronic intake of anti-inflammatory drugs were excluded from the study. For elimination of bias in the study double blinding (patient and observer) was done. Patients were allocated in two groups by randomization by computer generated sequence numbers; the even numbers were allocated Group E and odd numbers were allocated Group C. Group C: patients received 30 ml normal saline as loading dose and thereafter continuous infusion of 1ml/min Group E: patients received 0.5mg/kg esmolol in 30ml normal saline as loading dose and 30ug/kg/min as infusion till the end of the surgery All patients underwent a pre-anaesthesia checkup before surgery and all the routine and specific investigations were documented. The patients were kept nil per oral 6 hours prior to surgery. Standard monitors like ECG, NIBP, and pulse oximeter, BIS were applied and patients baseline parameters like pulse, blood pressure, respiratory rate, spO2 and depth of anaesthesia were recorded. An intravenous line was secured and patients were premedicated withInj.Glycopyrolate(4mcg/kg or 0.2mg),Inj.Fentanyl (1 mcg/kg) ,Inj. Ranitidine (1 mg/kg or 50 mg).In Group E Esmolol bolus 0.5 mg/kg in 30 ml isotonic saline was given and in Group C 30 ml isotonic saline bolus was given. Induction of anaesthesia was done with inj. Sodium thiopentone 5-6mg/kg i.v. and tracheal intubation facilitated by inj.Succinylcholine1.5-2mg/kg i.v. after 3min of pre-oxygenation with 100% oxygen. Maintenance of anaesthesia done with controlled ventilation with isoflurane 0.8 to 1.0% dial concentration and O2:N2O in the ratio of 40:60. Neuromuscular blockade was achieved with inj.vecuronium (0.08-0.1 mg/kg as loading and 1/5th dose as maintenance), top up dose of inj.vecuronium was given guided by neuromuscular monitoring. Group E: Esmolol started at the rate of 30µg/kg/min. Group C: Normal saline infusion given at the rate of 1ml/min. Vital parameters including HR, NIBP, SpO2 and ECG were monitored throughout the procedure. BIS Monitoring (depth of the anaesthesia) with BIS value kept between 50 to 60. When BIS value more than 60, changes in HR > 20% or mean arterial pressure >20% or above the base line for more than one minute, any presence of somatic signs or autonomic signs like lacrimation, swallowing or grimaces considering inadequate depth of anaesthesia and analgesia; the depth of anaesthesia was increased by increasing the dial concentration of isoflurane 0.2%. In case of any episode of bradycardia (HR<50 beats/min) and hypotension (fall in blood pressure more than 20% from the baseline was treated with inj. atropine and i.v.mephentermine respectively. Esmolol infusion was stopped at the end of surgery. Residual paralysis reversed with inj.Neostigmine 0.05mg/kg i.v. and inj. Glycopyrrolate 0.02mg/kg i.v. The patients were extubated when awake and monitored in the recovery room. Postoperatively nausea vomiting and pain scores were assessed. Pain was assessed by Visual Analogue Scale. Rescue analgesic inj.diclofenac sodium 1.5mg/kg was given when VAS score ≥ 4 and time was noted. Rescue antiemetic inj.ondansetron 0.06-0.08 mg/kg was given for episode of nausea, retching or vomiting and the time was noted. STATISTICAL ANALYSIS The sample size was calculated based on a previous study[2]from which parameter of pain score duration taken as guideline. Taking Zα=4.77 and Zβ =4.00 and assuming power of the study to be 80% and 95% confidence interval, a sample size of 30 in each group was calculated. Considering dropouts and failure, 35 cases in each study group were enrolled. Data were statiscally described in terms of mean±SD or frequencies when appropriate. The raw data was compiled in MS Excel sheets and statistical analysis was done by Statistical Package for Social Sciences (SPSS version 20.0). An unpaired t test was used to compare demographic variables, intraoperative haemodynamic variables (heart rate, systolic blood pressure) oxygen saturation, BIS and duration of analgesia between the groups. VAS scores of both the groups were compared. A P-value < 0.05 considered statistically significant.
RESULTS Both the groups were comparable with respect to age, sex, ASA grade II/III and duration of surgery.
Table 1: Demographic data
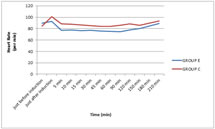
Graph 1 shows intra-operative heart rate. There was no significant difference in heart rate among both the group before induction. The heart rate decreased in group E 5 min after induction compared to group C and was statistically significant till the end of surgery (p<0.05). Graph 1: Intraoperative heart rate (per min)
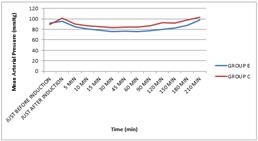
Graph 2 shows intra-operative mean arterial pressure. There was no significant difference in mean arterial pressure among both the group before induction (p>0.05). The MAP increased in group C (101.40±5.04) compared to group E (95.18±8.11) just after induction and was statistically significant (p<0.05). The MAP decreased in group E 5 min after induction compared to group C and was statistically significant till the end of surgery (p<0.05). Graph 2: Intra operative mean arterial pressure (mmhg)
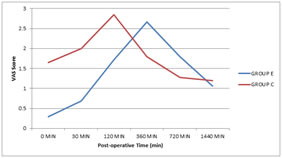
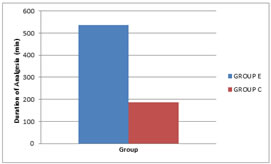
Graph 3 shows changes in mean VAS score in group E and group C in postoperative period. The mean VAS score was consistently high in group C than group E during first 4-5 hrs which was statistically significant (p<0.05). Graph 3: VAS score Graph 4 shows mean duration of analgesia in both groups. In our study, in group C mean duration of analgesia was 187.72±63.98 min and in group E it was 535.29±116.68min. This analysis shows that mean duration of total analgesia was significantly higher in group E than group C. (p value 0.0001)
Graph 4: Duration of analgesia (min) Table 2 shows mean duration at which rescue anti-emetic was given. In our study, in group C mean duration at which anti-emetic was required was 20.57±18.93 min and in group E it was 145.29±69.10 min. This analysis shows that mean duration at which rescue anti-emetic required was significantly lower in group C than group E. (p value 0.0001)
TABLE 2: TIME OF RESCUE ANTI-EMETIC IN PONV (min)
DISCUSSION Pain, postoperative nausea and vomiting are the most common postoperative complications in middle ear surgeries. Beta adrenergic antagonist activate G proteins in isolated cell membrane which indicates that beta blockers resemble clonidine in the mechanism of central analgesia.[2] Esmolol is an ultra short acting cardio selective beta-1 adrenergic receptor antagonist, it has been successfully used for perioperative sympatholysis. Perioperative esmolol administration contributes to the significant decrease in postoperative nausea, vomiting and postoperative pain, reduces patient distress and facilitates earlier discharge.1 In our study we found that there was no significant difference in heart rate among both the groups before induction. The heart rate increased in both groups, increase in heart rate was more in group C compared to group E, just after induction (approximately coinciding with the time of intubation) and was statistically insignificant (p<0.05). The heart rate decreased 5 min after induction in group E compared to group C and was statistically significant till the end of surgery (p<0.05). The attenuation of laryngoscopy reflex requires higher dose of inj.Esmolol (2mg/kg), so dose of 0.5mg/kg Esmolol at time of induction shows minimal effect on heart rate compared to control group. In our study we used esmolol loading dose 0.5mg/kg which is much less than 2mg/kg for attenuation of sympathetic response of laryngoscopy. Similar to our study T.A.R.S. Varma concluded that I.V. bolus dose of esmolol 2mg/kg is required for attenuation of sympathetic response to laryngoscopy and intubation.3 In one of the previous metaanalysis it was concluded that the preoperative mean values of HR were comparable between the two groups but after the induction of anesthesia and thereafter, there was a significant reduction in HR and MAP in the esmolol group when compared with the control group which was similar to our study.[4]There was a significant difference in the heart rate between both the groups at 60, 75, 90 and 105 min in a study by Bhawna et al.5 In our study we found that there was no significant difference in mean arterial pressure among both the groups before induction (p>0.05). The MAP increased in group C (101.40±5.04) compared to group E (95.18±8.11) just after induction and was statistically significant (p<0.05). The MAP decreased in group E 5 min after induction compared to group C and was statistically significant till the end of surgery (p<0.05). Similar to our study RitimaDhir et al. found that the baseline mean HR, MAP, mean systolic and diastolic blood pressure, were similar in both groups and statistically comparable from 0 min to 8 min. The hemodynamic parameters in Group C were significantly higher from 8th min onwards and remained higher till end of the procedure.2 In one of the previous Meta-Analysis it was concluded that after the induction of anaesthesia and thereafter there was a significant reduction in HR and MAP mean values in the esmolol group when compared with the control group.4 In our study the mean VAS score was consistently high in group C than group E during first 4-5 hr which was statistically significant (p<0.05). Similar to our study, a previous study found a significant difference in pain status based on VAS criteria between the two groups during the recovery period as well as at the third- and sixth-hours following surgery (P = 0.02, P = 0.001, and P = 0.0001, respectively). The VAS score was lower in the esmolol group at each of these monitoring time points.6 Similarly in a randomized trial by Nalan Celebi et al., they found that esmolol reduced the postoperative VAS and VRS scores, elongating the time to first analgesia and reduces the total i.v. morphine consumption and the number of patients who needed morphine.7 In our study, in group C mean duration of analgesia was 187.72±63.98 min and in group E it was 535.29±116.68 min. This analysis shows that mean duration of total analgesia was significantly higher in group E than group C (p value 0.0001). Similar to our study,InshaQureshi et al. in their study concluded that incidence of postoperative analgesia requirement over first 24 h after laparoscopic cholecystectomy is less in esmolol group compared to placebo group.9 Esmolol decreased the postoperative requirement of morphine and postoperative pain without increasing the risk of awareness in a study by G.Rajendra10 which was comparable to our study. In our study, in group C mean duration at which anti-emetic required was20.57±18.93 min and in group E it was145.29±69.10 min. Similar to our study Richard Watts et al. in their systematic review and meta-analysis found that there was a 61% reduction in the incidence of PONV in patients who received esmolol compared with placebo and presents the evidence that perioperative administration of esmolol decreases early postoperative pain intensity, opioid requirement, the requirement of rescue analgesics and PONV.11 Perioperative esmolol reduced the incidence of postoperative nausea vomiting in a study by Thiruvenkatarajan12 similar to our study. The limitations of our study is that it is a single centre study with limited number of patients. Further studies involving larger number of patients using esmolol in different doses can be studied to establish the efficacy of analgesic and antiemetic profile of esmolol. Also another limitation is preemptive administration of fentanyl could have partly contributed to the overall analgesia as well as postoperative nausea and vomiting. Hence an alternative drug to fulfill the requirement of analgesia as well as antiemetic in middle ear surgery can be searched and utilized in further studies.
CONCLUSION We conclude that intra-operative use of esmolol reduced analgesic requirements and maintained hemodynamic stability. Esmolol contributed to decreased post-operative analgesic requirements possibly by modulation of the sympathetic component of pain and its use decreased requirement of rescue antiemetic in middle ear surgeries.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home