|
Table of Content - Volume 20 Issue 2 - November 2021
Does MRI of different regions lead to different temperature changes in children done under anaesthesia? – A cross sectional study
Anusha Elizabeth Ben1, Merlin Shalini Ruth S2*
1Junior Resident, 2Associate Professor, Department of Anaesthesia, Chettinad Hospital and Research Institute, Kelambakkam, Tamil Nadu. Email: merlin5shalini@gmail.com
Abstract Background: Both general anaesthesia and low-ambient temperature in the magnetic resonance imaging (MRI) suite makes the paediatric patient vulnerable to fall in body temperature. But the radiofrequency radiations cause increase in body temperature. Studies have shown both increase and decrease in body temperature in children undergoing MRI under anaesthesia. But previously done studies have not shown if there is a difference in temperature changes because of different MRI scan regions. Aim: To determine if MRI of different regions cause different temperature changes in children undergoing MRI under anaesthesia and to find the predominant direction of temperature change. Setting: Prospective observational cross-sectional study. Methods: Two hundred and fifty children of age between birth and 16 years of age scheduled for MRI under anaesthesia were recruited. A baseline (pre-scan) and post-scan axillary temperature was recorded with the digital thermometer before and after the scan respectively both in the induction room. Results: There is a decrease in axillary temperature in children undergoing MRI under anaesthesia The median temperature fall in children across different MRI regions range from 0.8 to 1.1°C. Different MRI scan regions do not cause significant differential temperature changes. Keywords: paediatric, MRI, scan regions, axillary temperature.
INTRODUCTION Magnetic resonance imaging (MRI) has become a quintessential diagnostic tool, especially in children, because it is a nonionizing technique for accurately diagnosing soft tissue abnormalities. For a child it is a nightmare as the position in the gantry cause claustrophobia. In addition to this, the long scan duration time which requires the child to stay immobile, necessitates anesthesia/sedation. General anesthesia per se and low ambient temperature requirements for the functioning of MRI scanner makes children vulnerable to hypothermia while in the MRI suite.1,2 Sedation/anesthesia causes loss of thermoregulatory control which can cause significant drop in the core body temperature.3,4 Conversely, the MRI scanner generates radio-frequency radiation (RFR), which is absorbed by the patient. Due to differential specific absorption rate of different regions, the different body parts get heated differentially which is more likely to be more exaggerated in children.5,6,7 Studies done previously in children have shown mixed results with core temperature showing both rise and fall8,9 but hardly few studies are there to compare temperature changes across MRI of different regions. Monitoring temperature during MRI scans can be challenging, and active warming equipment and MRI compatible monitoring systems are both expensive. This makes temperature control for children in the MRI suite a complex process. We aim to determine whether MRI of different regions cause different temperature changes due to differential specific absortion rate. METHODOLOGY This is an observational cross sectional study done in a tertiary care teaching institute in south India. After getting approval from the institutional review board, (IRB no. 10907) we recruited consecutive 250 children of age between birth and 16 years scheduled for MRI under anesthesia during the 7-month period between October 2017 to April 2018. Children having hyperthermia of temperature of greater than 37.2°C or hypothermia of temperature less than 36°C, were excluded. Written informed consent was obtained from all parents/guardians. None of the patients were given sedative premedication prior to the procedure. All eligible patients were subjected to inhalational induction in the anesthesia room of the MRI suite. Intravenous access was achieved following which anesthesia was maintained with propofol total intravenous anesthesia (TIVA) or LMA with inhalational anaesthetic according to the preference of the consultant anaesthesiologist. The dose of propofol used was 100–150 mcg/kg/min. A baseline axillary temperature (pre-scan) was recorded by the consultant anaesthesiologist with the digital thermometer after induction holding it in the armpit in an immobile anaesthetised child for a minute. All patients were wearing light clothing and were covered with a single blanket before, during, and after the scan. The MRI room temperature was maintained between 20 and 24°C. MRI of various regions was done either with 1.5T or 3T (Philips, Achieva) scanners. Once the MRI scan was over, the patient was shifted to the anesthesia room for recovery, wherein post-scan axillary S temperature was immediately measured and the scan region was noted. If the child was found to be hypothermic, additional blankets were used. Descriptive statistics were given as frequencies for sex, age less than/equal to 6 years or greater than 6 years, weight less than/equal to 20 kg or greater than 20 kg. The temperature change across different regions during MRI were given as median and interquartile range. Box plot were used to show graphically. All statistical output was done using R software.
RESULTS The demographic characteristics of the study population are given in Table 1. The majority of the children belonged to the <6year age group, male sex, and less than 20 kg weight category. The mean age was 4 (±2.6) years and weight was 14.83 (±6.78) kg. The average duration was around one hour. Table 1: Patient Demographics
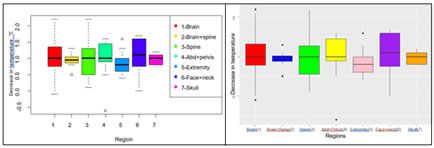
1 2 3 4 5 6 7 -0.5 0.0 0.5 1.0 1.5 2.0 Figure 1:Distribution of decrease in temperature in different regions Region Decrease in temperature 1-Brain 2-Brain+spine 3-Spine 4-Abd+pelvis 5-Extremity 6-Face+neck 7-Skull
Table 2: Temperature decrease in different regions of MRI
Figure 1: Distribution of decrease in Figure 2: Distribution of decrease in temperature temperature in different regions among different MRI regions
We studied if there was any difference in the temperature change across the MRI of different regions. All regions showed an overall decrease in axillary temperature except for three cases which showed an increase in temperature. Those children had an of MRI brain done.
DISCUSSION Our study shows that there is a median fall in temperature of range 0.8 to 1.1 degree celsius across different regions in children undergoing MRI under anaesthesia. The results concur with those of Lo et al. who showed mean temperature fall of 0.3 degree celsuis in anesthetized children.8 Bryan et al. and Machata et al. showed a significant rise in core temperature (tympanic membrane temperature) by 0.5°C and 0.2°C, comparing between 1.5T and 3T MRI scanners, respectively.9,10 In our study only 3 patients showed increase in temperature and it was too of the degree of o.3 degree Celsius. Isaacson et al. and Acar et al. showed mixed results with majority showing increase in temperature though not clinically significant in the former and decrease in temperature in the latter.11,12 But none of the studies showed as large an effect as our study. These studies have analysed the temperature changes, some even comparing the 1.5 T and 3T scanners but not across different regions. The strength of our study lies in the fact that large number of children were observed for the temperature change for MRI of different regions. Limitations of the study were that we could only measure the axillary temperature because of easy accessibility and ease of measurement. More number in the MRI scan of regions other than brain would have helped us to make a statistical analysis.
CONCLUSION MRI of different regions cause changes in temperature, especially a fall in temperature of varying degrees in children undergoing MRI under anaesthesia. Taking precautions to prevent fall in temperature would go a long way in preserving the homeostasis in children.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home