|
Table of Content - Volume 20 Issue 3 - December 2021
Comparison of efficacy of clonidine and tramadol for the control of shivering under spinal anaesthesia in Telangana Population
Rajesh Varma Alluri1, Bariki Santhosh Kumar2*, Pradeep Kode3, Deepraj Singh4
1,2Assistant Professor, 3Associate Professor, 4Professor & HOD, Department of Anaesthesia, Bhaskar Medical College, Hyderabad, INDIA. Email: bshkdr81@gmail.com
Abstract Background: Intra-operative shivering is very unpleasant and physiologically stressful can cause complications especially in patients with coronary artery disease because of associated increase in oxygen consumption. Hence anaesthetic drugs which control shivering successfully are preferred. Method: Out of 80 patients 40 patients were given clonidine, 40 with tramadol intra spinally (regionally) at L3, L4 level various grades of shivering was noted and side effects like hypotension, nausea, vomiting, bradycardia was also noted and treated efficiently. Results: Clinical manifestations were weight of the patient’s, duration of surgery in both groups was noted. Time taken shivering, incomplete response and recurrence was compared in both groups and (p<0.00) p value was higher significant. Conclusion: Both anaesthetic drugs were compared and Tramadol was proved to be better for control of intra-operative shivering under spinal anaesthesia due to rapid onset higher response rate, lesser recurrence, lesser sedation and least hemodynamic alterations than clonidine. Keywords: Spinal anaesthesia, Wrench grading, Filos scale, Tramadol, Clonidine
INTRODUCTION Intra-operative shivering occurs in 50-60% of patients undergoing regional anaesthesia.1 This may be normal thermoregulatory severing in response to hypothermic or may result from the release of cytokines by the surgical procedures. Intra-operative shivering is very unpleasant and physiologically stressful. It may also cause complications, especially in patients with coronary artery disease, because of associated increase in oxygen consumption by 1-6%.2 These complications can lead to cardio vascular and neurological deficits, as well as organ damage. Shivering of not treated may detrimentally impact patient outcomes, prolong recovery and prolong hospitalization. Intra-operative shivering also interfere intra-operative monitoring like ECG, SPO2 and blood pressure which may pose patients safety issues.3,4 Different drugs have been evaluated for preventing and treating shivering, however a gold standard drug treatment has not been defined. Therefore, the anaesthetic agents who cause least duration of shivering are preferred. Hence attempt was made to compare clonidine and tramadol for the control of shivering under spinal anaesthesia so that the present study will be a guide line anaesthesiologist to prevent shivering efficiently.
MATERIAL AND METHOD 80 (eighty) patients admitted at surgery department of Bhaskar Medical College Yenkapally, moinabad Rangareddy Hyderabad-500075, Telangana were studied. Inclusive Criteria: ASA grade I and II, aged between 18 to 40 years patients who developed intra-operative shivering post-spinal anaesthesia of grade 3 to 4 lasting for minimum 2 minutes were selected for study. Exclusion Criteria: Patients with history of fever, known sensitivity to drugs to be used shivering even before administering spinal anaesthesia requirement of supplementation of general anaesthesia were excluded from study. Method: Patients for elective lower abdominal and lower limb surgeries under spinal anaesthesia were studied. Detailed pre-anaesthetic check-up of all the patients posted for surgery was done a day prior to surgery. All the patients were kept nil by mouth for 8 hours prior to surgery. On the day of surgery the patients brought to the operation theatre. I.V. line secured, standard monitors attached and baseline parameters recorded. Base line temperature was recorded using thermometer in axilla. All the patients were pre-loaded with Ringer lactate 10 ml/kg before giving neuraxial blockade. All the fluids and drugs were stored and administered at room temperature and ambient temperature of the operating room was maintained at 22oc – 23oc. Spinal anaesthesia was performed with 23 or 25 gauge Quincke spinal needle in a sitting position at the L3-4 / 4-5 inter space (midline approach) with Bupivacaine (0.5% heavy) in dose of 3.5 ml to achieve a desirable level at T8-T10 dermatome in accordance with surgical procedure. After induction of spinal anaesthesia patients were observed for the occurrence of shivering. All patients who developed intra-operative shivering post-spinal anaesthesia of grade 3 or grade 4 lasting for minimum period of 2 minutes were included in the study. They were randomly allocated to two groups. Group A (n=40) patients received injection clonidine 50 µg IV and Group B (n=40) received injection Tramadol 50 mg iv. Grading of shivering was done as per wrench.5 It is as follows: Grade-0, No Shivering, Grade-I, one or more of the following; piloerection, peripheral vasoconstriction, peripheral cyanosis with, but without visible muscle activity, Grade-2; visible muscle activity confined to one muscle group, Grade-3 visible muscle activity in more than one muscle group, Grade-4 – Gross muscle activity involving the whole body. The study drug was administrated slowly IV as per the allotted group. The time in minutes at which shivering started after spinal anaesthesia (onset shivering) grade of shivering, time to disappearance of shivering after drug administration and response rate was recorded. Treatment that stopped shivering was considered successful. Duration of surgery was noted in both groups. Recurrence of shivering was also noted until the patient left the operation theatre. The patients who did not recurrence of shivering occurred were treated with additional dosage of clonidine (50 µg IV) or Tramadol (50 mg/IV) in the respective groups, (if required). Pulse rate, Blood pressure, Axillary temperature SPO2, were also monitored throughout, If systolic pressure (SAP) decreased more than 20% below the pre-anaesthetic value was considered as significant hypotension which was treated with injection Mephenteramine 6 mg in increments. Significant bradycardia (HR<60 bears/minutes) was treated atropine sulphate 0.6 mg intravenously. Sedation score was assessed with a four point scale as per filos (6). Awake and alert: Drowsy, responsive to verbal stimuli, Drowsy, arousable to physical stimuli unanswerable side effects and complications such as nausea, vomiting, hypotension, bradycardia, allergic reactions and sedation if present were recorded. If patients develop nausea and vomiting metaclopromide 10 mg/IV was administrated. Duration of study was July-2016 to June-2018 Statistical analysis: The results of both groups were compared with z test and some were classified with percentage. The statistical analysis was carried out SPSS software. The ratio of male and female was 2:1.
OBSERVATION AND RESULTS Table 1: Comparison of clinical manifestation both groups –
Table 1: Comparison of Clinical Manifestation in both groups
Table 1: Comparison of Clinical Manifestation in both groups
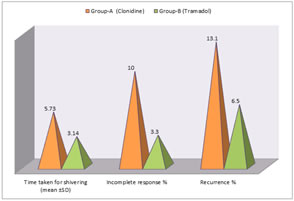
Table 2: Comparative study of Average time taken to control of shivering in complete response and recurrence in both groups. Time taken for shivering 5.73 (± 0.80) in group-A and 3.14 (± 0.77) in group-B, t test 14.7 and p value was highly significant (p<0.00). Incomplete response % - 10 (± 1.5) in group-A, 3.3 (± 0.5%) in group-B, t test was 26.8 and p value was highly significant (p<0.001). Recurrence % - 13.1 (± 0.2) in group-A, 6.5 (± 0.3) in group-B, t test was 53.3 and p value was highly significant. Table 2: Comparative study of Average time taken to control of shivering incomplete response and recurrence in both groups
Table 2: Comparative study of Average time taken to control of shivering incomplete response and recurrence in both groups
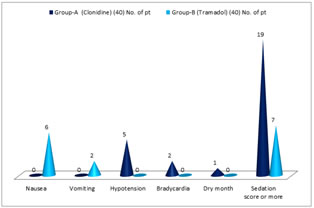
Table 3: Comparison of side effects in both groups – Nausea – 6 (15%) in group-B, vomiting 2 (5%) in group-B, Hypotension 5 (12.5%) in group-A, Bradycardia 2 (5%) in group-A, Dry month 1 (2.5%) in group-A, sedation score 19 (47.5%) in group-A, 7 (17.5%) in group-B
Table 3: Comparison of side effects in both groups
Table 3: Comparison of side effects in both groups
DISCUSSION Present study of comparison of efficacy of clonidine and tramadol for the control of shivering under the spinal anaesthesias in Telangana Population. The comparison weight in both group – 51.30 (± 1.05) in group-A and 49.25 (± 0.45) in group-B and t test was 11.3 and p value was highly significant (p<0.00) while duration of surgery less both group was more or less same hence (p>0.4) p value comparative study of Average time taken to control of shivering incomplete response and recurrence in both groups. Time taken for shivering (mean ±SD) 5.73 (± 0.80) in group and 3.14 (± 0.79) in group-B, t test was 1.47 and (p<0.000) p value was highly significant. Percentage of incomplete response was 10 (± 1.5) in group-A and 3.3 (± 0.5) in group-B, t test was 26.8 and p value was highly significant (p<0.00) percentage of recurrence 13.1 (± 0.3) in group-B, t test 53.3 and p value was highly significant (p<0.00) (Table-2). Comparative study of side effects in both groups – Nausea was observed only in group-B 6 (15%) and vomiting also in group-B, 2 (5%). But hypotension 5 (12%) bradycardia 2 (5%), dry month 1 (2.5%) and sedation score was 19 (47.5%) was observed only in group-A, 7 (17.5%) sedation score was observed in group-B, (Table-3). These findings are more or less in agreement with previous studies.7,8,9 Regional anaesthesia, either central neuraxial block or peripheral block is a safe and very popular technique used for various surgeries. However, 40% to 70% patients undergoing regional, anaesthesia develop shivering though it is also found to occur in general anaesthesia (10). Conidine is a centrally acting selective a2 agonist clonidine exerts its anti shivering effects at three levels Hypothalamus locus coeraleus and spinal card. At the hypothalamic level it decreases thermoregulatory threshold for vasoconstriction has high density of a2 adenoceptors and hence is effective in treating the established post-anaesthetic shivering. It also reduces spontaneous firing in coeruleus a pro-shivering centre in Pons. At the spinal cord level, it activates the a2 adronoreceptor and release of dynorphine. The depressor effects of these neuro transmitters at the dorsal horn11 modulate cutaneous thermal inputs clonidine is highly lipid soluble and easily crosses the blood brain barrier Due to these merits, interaction at the a2 adrenoreceptor at spinal and supra. Spinal sites occur within the central nervous system.12 Tramadol is an opoid analgesic with opoid action preferably mediated vice µ (mµ) receptor with minimal effect and kappa and delta binding sites. Tramadol also activates the mononergic receptors of the descending neuraxial inhibiting pain pathway. The anti-shivering action of Tramadol is probably mediated via its opoid or serotonergic and noradrenergic activity or both.13 In the present study It was observed that, clonidine as effective as tramadol in treating post spinal anaesthetic shivering but the time taken for shivering was quite less 3.14 (± 0.77) in tramadol while time taken for shivering in clonidine was 5.17 (± 0.80) and recurrence was 6.5 (± 0.3) in tramadol and 13.4 (± 0.2) in clonidine hence tramadol proved to be quite efficient than clonidine. Moreover hypotension, bradycardia, dry month was not observed in patients treated with tramadol and sedation score was 7 in tramadol while more than double i.e. 19 in clonidine treated patients.
SUMMARY AND CONCLUSION In the present comparative study of efficacy of tramadol versus clonidine both are effective for control of shivering under spinal anaesthesia but tramadol hydrochloride is better as compared with clonidine due to rapid onset, higher response rate, more effective control, lesser recurrence, less sedation and hemodynamic alterations though nausea and vomiting are more in tramadol group but still controllable. This study demands further neuro-muscular, patho-physiological, nutritional, hormonal, pharmacological, genetic studies because the exact mechanism which leads to shivering after regional anaesthesia is still un-clear. Limitation of study: Study owing to tertiary location of present studied hospital less number of patients we have limited research findings.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home