|
Table of Content - Volume 21 Issue 1 - Januray 2022
Ultrasound-guided combined interscalene-superficial cervical plexus block in clavicular fractures for surgical anesthesia: A retrospective observational study
Manuel Shaji Shara Azikakath1, Dhara Tanna2*, Neha Parikh3, Neeta Bose4, J C Vasava5
1,2Assistant Professor, 3 Tutor, 4Associate Professor, 5Professor & HOD, Department of anaesthesiology, GMERS Medical College and Hospital, Gotri, Vadodara, Gujarat, INDIA. Email: shajimanual@yahoo.co.in, dr.dharatushar@gmail.com, drnehaparikh2007@gmail.com, neetabosenayak@hotmail.com, jc.vasava@yahoo.in
Abstract Background: Clavicular fractures are common among young males, mainly due to trauma. The anaesthesia of choice had been General Anaesthesia in order to provide satisfactory surgical conditions. Considering the advantages of ultrasound guided regional anaesthesia over general anaesthesia, combined blocks are now being practised for upper limb surgeries. We present our retrospective observational findings regarding the use of ultrasound-guided combined interscalene-cervical plexus block (ISC-SCPB) as a sole anesthetic technique in routine clavicular fracture surgeries. Materials and Methods: We retrospectively reviewed the charts of patients, who underwent clavicle fracture surgery by ultrasound-guided combined interscalene-cervical plexus block. Interscalene Block was given by 20 ml of Local Anesthetic mixture (Lignocaine 2% and Bupivacaine 0.5%) and Superficial Cervical Plexus block 6 ml of local anesthetic mixture with in plane technique using linear probe. Time to achieve sensory and motor blockade, average duration of surgery, duration of sensory and motor block, block success and complications were evaluated. Results: 30 patients (100%) were operated successfully for clavicular fracture under ultrasound guided combined interscalene-superficial cervical plexus block without conversion to general anaesthesia. The sensory and motor effect were achieved at an average of four and six minutes respectively. The sensory analgesic effect lasted for an average of five hours providing an added advantage of immediate post-operative pain relief. No acute complications related to block or surgical complication were noted. Conclusions: Ultrasound guided combined interscalene-cervical plexus block is a successful and effective anesthesia technique in clavicular fracture surgeries and also provides excellent immediate post-operative analgesia. Key words: Upper limb blocks, combined interscalene cervical plexus block, clavicular fractures.
INTRODUCTION Fractures of the clavicle represent 2.6–4% of all fractures, is common in young males and elderly individuals often resulting from direct trauma to the shoulder.1 Displaced fractures are mainly treated surgically for a better functional outcome. Traditionally, General Anesthesia (GA) is preferred as it provides satisfactory surgical conditions. Advantages of GA being completely relaxed and unaware patient, there are some disadvantages like multi-drug usage, post operative nausea, vomiting, headache, risks of raised haemodynamic stress response and airway complications, which makes regional anesthesia techniques more preferable.2Regional anaesthesia has the advantage of being relatively cheap, superior analgesia with early ambulation and sparing from the unwanted side effects of GA. Inspite of the wide use of regional anaesthesia in a variety of upper limb surgical procedures, there are very few reports regarding its use in clavicle surgical fixation of clavicular fractures.3 The sensory innervation of clavicle is controversial, receiving sensory branches from supraclavicular, subclavian and/or suprascapular nerves,4 which may lead to unsatisfactory surgical anesthesia with interscalene blocks (ISB).5 Taking into consideration this variation in innervation, interscalene block combined with cervical plexus block seems to be an effective and a promising method for adequate surgical anesthesia.3,6 Ultrasound guided technique is more advantageous over the landmark-based technique as we are able to visualize the spread of local anesthetic in the correct plane, thus increasing the success rate. The use of Ultra Sonography (USG) guided regional anaesthesia routinely as a sole anaesthetic technique for surgical fixation of clavicle has not been well established.7 So, we aim to retrospectively observe and present our findings regarding the use of ultrasound-guided combined interscalene- cervical plexus block (ISB-CPB) as a sole anesthetic technique in patients posted for routine clavicular surgeries.
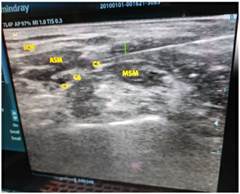
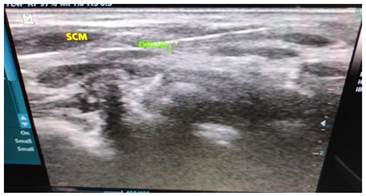
MATERIALS AND METHODS We retrospectively reviewed charts of 30 patients, who underwent clavicle fracture surgery under regional anesthesia (Interscalene and superficial cervical plexus block) from January 2021 to July 2021. Informed consent for the surgery and anesthesia procedure were obtained from all patients after informing them about the surgery and anaesthesia methods in detail. Anesthesia method: All the blocks were performed by a team of anaesthesiologists with good experience in USG guided nerve blocks. The procedure was performed in operation theatre after checking a pre-procedural safety checklist, applying standard monitoring and intravenous line. All resuscitative measures were kept ready. Taking all aseptic precautions, with sterile drapes, gloves and transducer cover, the block was performed with ultrasound guidance using a high frequency linear transducer (Mindray Diagnostic Ultrasound System model Z6). The ultrasound transducer probe marker was placed facing medially on related side across the lateral neck of the patient in transverse orientation in supraclavicular fossa to identify subclavian artery, first rib and the brachial plexus trunks. Using the ‘‘traceback’’ method by sliding the transducer cephalad, the brachial nerve roots were identified in the interscalene groove, by visualizing the spotlight sign. After confirming the identity of anterior scalene, middle scalene, the C5, C6 and C7 roots within the interscalene groove and probe position, a 1.5-inch 23 G hypodermic needle was inserted from lateral side of probe using in plane technique, and advanced with visualisation of tip and shaft through the middle scalene entering the fascia into the interscalene groove avoiding injury to the neighbouring structures. (Figure 1) The brachial plexus at this level appears as three to five hypoechoic circles. After careful aspiration for nonappearance of blood, local anesthetic 0.5% bupivacaine and 2% lignocaine combined together (total 20 ml) was injected continuing intermittent aspiration, redirected if resistance felt and hypoechoic spread was noted adjacent to and surrounding the plexus.8 Now the transducer was directed and placed at posterior border of sternocleidomastoid muscle at level of thyroid cartilage in transverse orientation. The needle was inserted from lateral side of probe in plane from lateral to medial and the tip positioned in fascia deep to sternocleidomastoid muscle and local anaesthetic (bupivacaine, lignocaine) 6 ml was injected and spread noted9,10 (Figure 2) Sensory blockade was checked by pinprick at the surgical site and motor blockade by loss of shoulder abduction. The effect was also checked for pain with mobilization of the arm and palpation of the clavicle. Where there was no conversion to general anaesthesia, the block was considered successful. Surgery was conducted in supine position. All the patients received injection Midazolam 1 mg iv, injection Ondansetron 4 mg iv and injection Dexmedetomidine 0.5 microgram/kg over 15-20 minutes after induction. Time to achieve sensory and motor blockade, duration of sensory and motor block, block success and complications like, pneumothorax, respiratory distress, Horner’s syndrome, phrenic nerve palsy, accidental arterial puncture, hematoma formation and signs of local anaesthetic toxicity were evaluated from the records. The need of any additional sedative and analgesic drugs were also evaluated. Statistical analysis: All the data was entered in microsoft Excel. Continuous quantitative data were expressed as number, mean, median and standard deviation as appropriate, and qualitative data were expressed as number and percentage. Descriptive statistics was calculated and analysed using GraphPad version 2.0
OBSERVATIONS AND RESULTS Total 30 patients who underwent clavicle surgery were studied. Patients were ASAI and II risk. Patients’ demographic characteristics are shown in Table 1. About 73.33% were male and 26.67% were female with around 83.33% having lateral 1/3rd fracture and 16.67% mid shaft fracture. Four patients underwent nail insertion, three reconstruction with autograft and 23 patients had open reduction with plating. Among the patients, one patient had liver disease, two were hypertensive and one was hypertensive with diabetes and ischemic heart disease. All other patients were without any co-morbidities. Two patients needed injection ketamine 50mg iv as they complained of pain on manipulation. These patients were not considered in block failure as no repeat dose of ketamine or general anesthesia was needed and surgery went on uneventfully. Average duration of surgery was 80 minutes with sensory and motor effects achieved at average of four and six minutes respectively. The duration of sensory analgesia lasted for average five hours and motor effects for average period of six and half hours. No complication related to block or surgical complication occurred. The surgeons were satisfied with the anaesthesia method and were in favour of its use in high-risk patients. Outcome of surgery and anaesthesia is shown in Table 2.
Table 1: Patient demographic characteristics
Table 2: Anaesthesia and surgery outcomes
Figure 1 Figure 2 Figure 1: Showing the cervical nerve roots (C5,C6,C7) in the interscalene groove the anterior scalene muscle(ASM),middle scalene muscle(MSM) ,the sternocleidomastoid muscle(SCM) and the needle; Figure 2: Shows drug spread below the facia deep to sternocleidomastoid
DISCUSSION Our findings in this retrospective observational study demonstrated that regional anesthesia technique with USG guided interscalene and superficial cervical plexus block was reliable and effective in clavicular fracture surgeries. Ultrasound guided regional anaesthesia is safe both in terms of technique, reducing the number of attempts and dose of local anaesthetics used thus enabling the performance of multiple blocks. Its advantages over the landmark-based technique includes the ability to visualize the nerves (structures) directly and the spread of local anesthetic in the correct plane, thus increasing the success rate, and avoiding inadvertent puncture of neighbouring structures and related complications.11,12 Compared to general anaesthesia regional anaesthesia shortens the hospital stay length and gives early postoperative functional outcomes.13 Tran et al. conducted a review of literature to understand the sensory innervation of the clavicle and they suggested the supraclavicular, subclavian, and long thoracic/suprascapular nerves, alone or together, may be responsible for pain transmission after clavicular fracture and surgery, the exact role of the individual nerves still remains controversial. As per the authors, SCPB, ISB or combined ISB- SCPB can be used for analgesia for clavicular surgeries.4 The cervical plexus is formed by the ventral rami of the upper four cervical nerves (C1-C4). Various approaches are suggested for cervical plexus block. Telford and Stoneham et al. suggested that the SCPB is a subcutaneous injection of local anaesthetic drug along the posterior tapering border of sternocleidomastoid muscle.14 Pandit JJ et al., in an anatomical study, described intermediate cervical plexus block as an injection of local anesthetic deep to sternocleidomastoid, under investing facia of neck. And deep cervical plexus block as an injection of local anesthetic below the deep cervical facia, close to cervical transverse process. however, the superficial cervical space communicates with the deep cervical space and thus leading to spread of drug in superficial blocks to structures beneath the deep cervical fascia thus explaining the efficacy of superficial cervical plexus blocks.10,15 There are a few observational studies suggesting usefulness of ISB combined with SCPB as a sole anesthetic technique for clavicle surgeries.3,7 Potsangbam et al. conducted an observational study to establish the efficacy of SCPB with lanmark technique combined with USG guided ISB as a sole anesthetic technique for clavicular surgery. The authors used 10 ml of LA in SCPB and 20 ml in ISB. In contrast, we used only 6 ml of LA for SCPB as with USG guidance, the desired effect can be achieved with less volume of LA drug.7 Krishna Arjun et al. conducted a randomised controlled study comparing ISB with either SCPB or ‘Intermediate’ cervical plexus block with USG guidance for clavicular surgeries. They found ISB combined with ‘intermediate’ cervical plexus block had better success, with fast sensory block and increased duration of postoperative analgesia as compared to ISB combine with SCPB16 While performing ultrasound guided cervical plexus block we aimed at placing the needle tip under the sternocleidomastoid muscle below the investing cervical fascia of the neck and not subcutaneous as per anatomical study reports10,17 and interscalene block by locating the spot light sign. Due to fear of block failure, in anaesthesia practice, general anaesthesia appears to be widely preferred in clavicular surgeries. This fear has been overcome by use of ultrasound guided regional blocks with improved block success rate.11 Hence we could change our routine institutional practice of general anaesthesia for clavicular surgeries to regional anaesthesia techniques Limitations: The limitation to our study is that it is retrospective in nature and doing a prospective study on this topic would provide a real time information. Compared to other fractures clavicular fractures are not so common so studied cases are few. Details during the procedure like time taken, number of attempts and long-term complications were not evaluated. Comparing the regional technique with general anesthesia in a randomised control study can be planned.
CONCLUSIONS From our study, we propose that combined interscalene-cervical plexus block can be practiced as a sole anesthesia technique in clavicular fracture surgeries and also provides excellent immediate post-operative analgesia. Definitely prospective randomized trials would determine the best option.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home