|
Table of Content - Volume 21 Issue 2 - February 2022
Study on evaluating adequacy of combined lumbar plexus and sacral plexus block in lower limb surgeries
Anjani Bhojani1, Deepa Gondalia2*, Sandhya Margiya3, Vandana Parmar4
1Senior Resident, 2Associate Professor, 3Resident, 4Professor And Head of Department, Department of Anaesthesiology, P.D.U Medical College And Hospital, Rajkot-360001, Gujarat, INDIA. Email: anjanibhojani179@gmail.com, gondaliadeepa@yahoo.com, sandhyamargiya@gmail.com, drvandanapithadia@yahoo.com
Abstract Background: The scope of anaesthesia has shifted from general and neuraxial anaesthesia to peripheral nerve plexus blocks for isolated limb surgeries with the advent of newer techniques such as ultrasound and peripheral nerve stimulator. The present study was aimed to assess the adequacy and suitability of simple and safe technique of combined lumbar and sacral plexus block for various lower limb surgeries using peripheral nerve stimulator. Materials and Methods: Eighty two patients belonging to ASA grade I/II/III/IV posted for lower limb surgeries were selected. Each patient was given 20ml of Inj. bupivacaine (0.5%), 20 ml of Inj. lignocaine+ adrenaline (1.5%) and 5 ml normal saline total of 45 ml of mixture equally divided in both lumbar plexus and sacral plexus block. The onset and duration of sensory and motor blockade for both blocks, intraoperative haemodynamic monitoring and duration of postoperative analgesia were observed in all the patients. Result: The perioperative heart rate and mean arterial pressure changes were not significant and within 5% of baseline values for all the patients. The duration of postoperative analgesia was 761.7 ± 158.58 minutes. The onset time of sensory and motor blocks are 12.4±2.44 and 22.6±2.78 minutes respectively. The duration of sensory and motor blocks are 518.7±146.02 and 341.7±57.88 minutes respectively. Conclusion: Combined lumbar- sacral plexus block is a safe and efficient method of anaesthesia for lower limb surgeries as it avoids the complications of general and neuraxial anaesthesia and provides stable perioperative haemodynamic and prolonged postoperative analgesia. Keywords: Lumbar plexus block, lower limb surgeries, sacral plexus block.
INTRODUCTION Patients undergo lower limb surgeries for a variety of conditions ranging from fractures, arthroscopies, vascular procedures to diabetic foot debridement and amputation. Anaesthetising these patients can be quiet challenging because of the comorbid general conditions including old age, concomitant anticoagulant administration and complications of diabetic autonomic neuropathy. General anaesthesia, when administered to these groups of patients, has higher incidence of postoperative cognitive dysfunction, pulmonary complications, postoperative nausea/vomiting, and delay in recovery. Regional anaesthesia including central neuraxial blocks and peripheral plexus blocks has been beneficial in reducing the mortality and morbidity by reducing the incidence of many complications. Among the regional blocks, subarachnoid block is the most commonly performed procedure, but is associated with complications like intraoperative hypotension which may be difficult to handle in a patient with diabetic autonomic neuropathy or dilated cardiomyopathy, post dural puncture headache preventing early mobilization, urinary retention requiring catheterization, and epidural hematoma.1 Peripheral plexus block can provide an alternative to the above-mentioned techniques and with the use of newer modalities such as ultrasound and peripheral nerve stimulator in regional anaesthesia, the scope of anaesthesia has shifted from general and neuraxial anaesthesia to peripheral nerve blocks for isolated limb surgeries. These blocks also provide postoperative pain relief which contributes to improved patient satisfaction, stable hemodynamics, early ambulation, decreased length of hospital stay and hospital cost.2 Lumbar plexus block blocks femoral nerve, obturator nerve and lateral cutaneous nerve of thigh while Sacral plexus block blocks sciatic nerve and posterior cutaneous nerve of thigh. When Lumbar plexus block and Sacral plexus block are given together, complete lower limb anaesthesia is obtained. Hence, we aimed to assess the adequacy and suitability of simple and safe technique of combined lumbar and sacral plexus block for various lower limb surgeries using peripheral nerve stimulator.
MATERIAL AND METHODS After approval from Institutional Ethics Committee-Human between September 2018 to September 2020, eighty-two adult patients aged 25-100 years belonging to ASA Grade I- IV, scheduled for lower limb surgeries under combined lumbar plexus and sacral plexus blocks in a prospective observational study in PDU Medical College, Rajkot. All patients underwent a thorough pre-anaesthetic check-up which included history taking, general examination, systemic examination and local neurological examination. Routine investigations were carried out for all patients. Written informed consent was taken from all the patients for anaesthesia as well as enrolment in the study. Benefits and likely complications of the technique used were explained to the patients and their caretakers in understandable language. Patients with known case of allergy to local anaesthetics and dexmedetomidine, local infection at site of block, morbid obesity, neuromuscular diseases, sepsis, bleeding disorders or patient on anticoagulant therapy were excluded. The day before the surgery, procedure was explained to the patient and kept nil by mouth after 10 pm. On the day of surgery, standard monitors like Electro Cardio Gram (ECG) leads, Non-Invasive Blood Pressure (NIBP) cuff and pulse oximeter were applied and patient’s baseline parameters like Pulse Rate (PR), Systolic, Diastolic and Mean Blood Pressure (SBP, DBP, MBP respectively) and SpO2 were recorded. Intravenous line was secured and patient was premedicated with: Inj. Glycopyrrolate (0.004mg/kg) iv, Inj. Ranitidine (1 mg/kg) iv, Inj. Ondansetron (0.08mg/kg) iv. Conscious sedation was achieved by giving Inj. Dexmedetomidine 0.5µg/kg loading dose over 15 minutes prior to procedure and 0.5 µg/kg/hour infusion thereafter. Supplemental oxygen was given by venti mask. Local anaesthetic mixture of 45 ml was prepared by adding 20ml of Inj. Bupivacaine (0.5%), 20 ml of Inj. Lignocaine+ Adrenaline (1.5%) and 5 ml normal saline (with due consideration of patient’s weight and maximum dose). The Lumbar Plexus block was performed using a posterior paravertebral approach at the L4 vertebral level. Patient was laid in the lateral decubitus position (Sim’s position), with the operative side facing up. The insertion site of needle was determined as follows. A line was drawn connecting the iliac crests (intercristal line). The Spinous Processes (SP) and Posterior Superior Iliac Spine (PSIS) were identified and marked. A line through the PSIS was drawn parallel to the line joining the SPs. The site of needle insertion was at the junction of the line passing through PSIS and intercristal line (L4). Under full aseptic conditions, local infiltration with 3 ml of 2% lidocaine was injected into this point subcutaneously. A PNS (Peripheral Nerve Stimulator) insulated needle of 100 -120 mm needle was inserted and connected to the nerve stimulator (Stimuplex B.Braun Medical, Germany) with a starting output of 1.5 mA and 2 Hz. The needle was inserted and directed perpendicularly to contact the transverse process of L4. After touching the process, the needle was then redirected caudally. The proximity to the plexus was identified by the contraction of the quadriceps muscle in response to electrical stimulation. Then needle was advanced until muscle twitches were elicited with currents between 0.3 and 0.5 mA at 2Hz. After frequent negative aspirations, 22-22.5 ml of local anaesthetic mixture prepared earlier was injected. The Sacral Plexus block was given via Labat’s approach. In Sim’s position, the needle was inserted under full aseptic conditions, after local infiltration with 3 ml of 2% lidocaine into this point subcutaneously at a right angle to all cutaneous planes at the caudal end of a 5cm line originating from, and perpendicular to, the middle of a line that connects the greater trochanter and posterior superior iliac spine. In each case, neural structure was identified with the help of a nerve stimulator using a stimulus of 1.5 mA at 2 Hz, while contractions of the gastrocnemius (foot plantar flexion) and/or tibialis anterior (foot dorsi-flexion) indicated proximity to the sciatic nerve and the needle was advanced until currents between 0.3 and 0.5 mA at 2 Hz elicited muscle twitches. After frequent negative aspirations, remaining 22-22.5 ml of local anaesthetic mixture was injected. Onset of nerve block, for each sensory and motor blocks was evaluated every 5 min and evaluations continued for 30 minutes after completion of the nerve blocks. In addition, signs of sensory block were also seen in the other lower extremity. Sensory evaluation was done using a blunt 24-gauge hypodermic needle that comprised of loss of pinprick sensation in the femoral (anterior thigh), lateral cutaneous (lateral thigh), obturator (medial thigh), posterior cutaneous (posterior thigh) and sciatic (sole of foot) nerve territories. The motor block was evaluated by Bromage score. Bromage Score
The onset of sensory and motor blocks were defined as the time from completion of the lumbar plexus and sacral plexus block to the occurrence of sensory block at the related nerve territories and motor block. All patients received Inj. Tramadol 1mg/kg i.v. whenever patient complained of pain and time for need of rescue analgesia was noted. Total duration of analgesia was considered as time interval between completion of block to rescue analgesic given. Total duration of sensory blockade (Time interval between onset of sensory block and complete recovery of sensation) and total duration of motor blockade (Time interval between onset of motor block and complete recovery of motor power) were also observed. An infusion of ketamine 50mg +propofol 100mg diluted to 50 ml was started at varying rate according to the requirement of some patients for sedation after starting the procedure due to positional discomfort. In our study primary outcome measures were duration of analgesia while secondary measures were onset and duration of sensory and motor blockade, patients’ and surgeons’ satisfaction with block were noted as satisfactory and unsatisfactory and evidence of any adverse drug reactions. The data was analysed by Graphpad Prism software. All the above observations were recorded and expressed as mean ± standard deviation (SD) or percentage. Intragroup comparison of intraoperative haemodynamics was done using the student’s paired ‘t’ test. P value <0.05 was considered as significant.
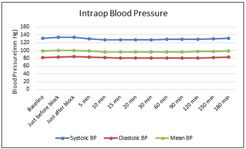
OBSERVATIONS AND RESULTS The demographic profile (age and gender), ASA grading and duration of surgery were observed (Table 1). Intragroup comparison of hemodynamic parameters was done with the baseline values which were not significant during the perioperative period (Graph 1). The mean onset and duration of sensory block and motor block are given in Table 2. Motor blockade in all the surgeries were Bromage grade 4 and 3 in 75 (91.46%) and 7 (8.54%) cases respectively. The mean duration of analgesia was 761.7 ± 158.58 minutes. Inj. Tramadol 1mg/kg was given as rescue analgesic whenever patient complained of pain. Patient’s and Surgeon’s satisfaction scores were as following: Patient’s satisfaction score: Satisfactory/Unsatisfactory – 97.56% / 2.44%. Surgeon’s satisfaction score: Satisfactory/Unsatisfactory – 98.78% / 1.22%. We observed that 1 patient had nausea, 2 patients had episode of vomiting and 1 patient developed hypotension. No other complications like bradycardia, intrathecal or epidural drug administration, local anaesthetic systemic toxicity, neuropathy or intraperitoneal injection were observed. Table 1: Demographic data, ASA Grading, Duration of Surgery
Table 2: Onset and Duration of Sensory and Motor Blocks
Graph 1: Intraoperative Blood Pressure Changes
DISCUSSION Our study used the combination of lumbar plexus block and sacral plexus block rather than either technique alone because of the more reliable blockade produced by both lumbar and sacral plexus block which has a specific site effect on only one leg and causes lesser physiologic disturbance with a comparable anaesthetic effect. Good post-operative analgesia produces a long lasting, continuous effective analgesia with minimum side effects. The benefits of adequate postoperative analgesia are clear, and include a reduction in the postoperative stress response,3 reduction in postoperative morbidity,4 and in certain types of surgery, improved surgical outcome.5 Effective pain control also facilitates rehabilitation and accelerates recovery from surgery.3,6 Some other benefits of effective regional analgesic techniques include pain intensity reduction, decreased side effects from analgesics, and improvement in patient comfort.6 Lumbar plexus and sacral plexus block require moderate volume and concentration of local anaesthetics to achieve pain relief without local anaesthetic toxicity. Whenever any block requires high volume of local anaesthetic drug, local anaesthetic systemic toxicity is always our point of consideration. If any one particular drug is used for anaesthetic management (i.e., producing sensory as well as motor blockade) we would not be able to give large volume with required higher concentration of the drug. So, we used combination of two drugs. In that way maximum allowable volume and concentration of both drugs can be used safely without any chances of drug toxicity and with benefits of adequate sensory and motor blocks.7,8,9 We used lignocaine with adrenaline for block so that may be the reason for early onset of sensory and motor blocks and also used higher concentration of bupivacaine (i.e. 0.5%) causing prolonged duration of blocks which resulted in prolonged duration of analgesia was 761.7 ± 158.58 minutes in our study.9,10,11,12 In our study, onset of sensory block and motor block was 12.43±2.44 minutes and 22.63±2.78 minutes respectively.9,10 Duration of sensory block and motor block was 518.78±146.02 and 341.71±57.88 minutes respectively.7,10Motor blockade in all the surgeries were Bromage grade 4 and 3 in 75 (91.46%) and 7 (8.54%) cases respectively.1,10 Hemodynamic parameters like pulse rate, systolic blood pressure, diastolic blood pressure and mean blood pressure were recorded and intragroup comparison with baseline parameters showed no significant difference therefore marked hemodynamic stability was noted.13,14,15 In our study, patient’s satisfaction score was 97.56% and surgeon’s satisfaction score was 97.78%. Dexmedetomidine induces sedation and enhanced motor and sensory blockade, thus can be the reason for high satisfaction rate, producing analgesia without respiratory depression.1,10,11,16 In our study, out of 82 patients, 1 patient had nausea, 2 patients had episode of vomiting and 1 patient developed hypotension. Complications that occurred can be due to other conditions related to patient’s ASA status, co-existing diseases, age, surgical stress, surgical blood loss, etc. So, these complications are not related to block and the procedure only but also on patient’s condition.10,17 The use of peripheral nerve stimulator has shown the considerable increase in the success rate of block and remains a popular technique used alone despite the use of ultrasound-guided peripheral nerve blockade.18 It allows a precise localization of nerve plexus improving the accuracy and decreasing the chances of nerve injury.19 Due to unavailability of USG in our institution, we have chosen to use peripheral nerve stimulator in our study.
CONCLUSION We concluded from our study that combined lumbar plexus block and sacral plexus block with light sedation is a simple, safe and efficient mode of anaesthesia for lower limb surgeries with the advantages of stable intraoperative haemodynamics, prolonged postoperative analgesia and with very good patient’s and surgeon’s satisfaction. If standard technique is followed, complications are minimal and not significant. Although technically more demanding and time consuming, it is a beneficial alternative to neuraxial and general anaesthesia for high-risk patients undergoing unilateral lower limb surgeries.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home