|
Table of Content - Volume 21 Issue 2 - February 2022
Compare study on incidence of PDPH using 25g QUINCKE and 25g WHITACRE needles undergoing elective surgery by spinal anaesthesia
S Premkumar1, M Senthil Marappan2*, K Viveka3, V A Sabapathy Appavoo4, Prabhu Thilaak4, Varshitha Kumar5,6
1Assistant Professor, 2Associate Professor, 3Postgraduate, 4,5Professor, Department of Anaesthesia and Critical Care, Vinayaka Missions Kirupananda Variyar Medical College and Hospital, Vinayaka Missions Research Foundation to Be University, Salem, Tamil Nadu, INDIA. 6Senior Resident, Department of Anaesthesia and Critical Care, Sri Venkateshwara Ramnarain Ruya, Hospital, Tirupati, Andhra Pradesh, INDIA. Email: marappansenthil@gmail.com
Abstract Background: Spinal anesthesia is relatively a safe procedure compared to general anesthesia. It provides good muscle relaxation and avoids fetal as well as maternal risks of general anesthesia. Requires minimum postoperative anesthesia care and provides adequate postoperative analgesia. Aim And Objective: To compare and study the incidence of PDPH using 25G Quincke and 25G Whitacre needles undergoing elective surgery by spinal anesthesia. Methods: this is a comparative study of 50 patients divided into two groups of 25 each. Patients were assessed daily for four consecutive days following surgery for post-Dural puncture headache at Vinayaka Missions Kirupananda Variyar Medical College, a Tertiary Care Hospital in Salem 2019. Results: Eight percent of the study population had a headache in the WHITACRE group while 16% of the study. the population had a headache in the QUINCKE group. The incidence of headache in the QUINCKE group is twice that of the WHITACRE group. The result is not statistically significant. One patient (4%) had a headache in the QUINCKE group on day one while none had in the WHITACRE group. The observation is not statistically significant. Two patients (8%) in the WHITACRE group had a headache while three patients (12%) in the QUINCKE group had a headache on day two. In other words, 40% of the study population had a headache in the WHITACRE group while 60% had headaches in the Quincke group. The observation is not statistically significant. One patient (4%) had nausea in the QUINCKE group on day one while none had in the WHITACRE group. Conclusion: spinal puncture is an important cause of iatrogenic morbidity in the form of post-Dural puncture headache. The incidence of these headaches can be reduced by using thin atraumatic needles in the procedure. Keywords: Quincke needle, Whitacre needle, post-Dural puncture headache, spinal anesthesia.
INTRODUCTION Spinal anesthesia has been widely practiced as it is safe, simple, economical, easy to perform, requires minimal apparatus and it’s a reliable technique that is an effective form of anesthesia used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus.1 It provides profound muscle relaxation, has minimal effect on blood biochemistry and decreases intra-operative blood loss, maintains airway, and produces excellent operating conditions. It requires minimum postoperative anesthesia care and provides adequate postoperative analgesia. Above all, patients remain conscious during surgery.2 Spinal anesthesia is a favorable alternative, when the surgical site is amenable to the spinal blockade, for patients with severe respiratory disease such as chronic obstructive pulmonary disease (COPD) as it avoids potential respiratory consequences of intubation and ventilation.3 It may also be useful, in patients where anatomical abnormalities may make tracheal intubation very difficult. Spinal anesthesia is the technique of choice for a cesarean section as it avoids intubation and the risk of failed intubation.4 In pediatric patients, spinal anesthesia is particularly useful in children with difficult airways and those who are poor candidates for general anesthesia such as increased respiratory risks or presence of full stomach. Since the introduction of spinal anesthesia by August Bier (1898), many developments and innovative alterations in the technique to attain perfection have taken place today.5 Though it is most commonly used for surgeries below the umbilicus, recently its uses have extended to some surgeries above the umbilicus as well as for postoperative analgesia. Procedures that use spinal anesthesia include Orthopedic, Vascular surgery on the legs, Endovascular, Hernia (inguinal or epigastric), Hemorrhoidectomy, Transurethral resection of the prostate and transurethral resection of bladder tumors, Hysterectomy, Caesarean sections, Pain management during vaginal birth and delivery, Urology cases, Examinations under anesthesia.6 Subarachnoid blockade (SAB) delivers the drug to the subarachnoid space and into the cerebrospinal fluid, allowing it to act on the spinal cord directly. postdural puncture headache (PDPH) has remained a well-recognized complication.7,8 This can also be used to effectively treat and prevent pain following surgery, particularly thoracic, abdominal, pelvic, and lower extremity orthopedic procedures.9,10
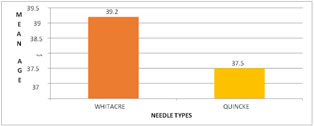
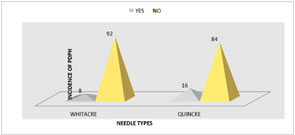
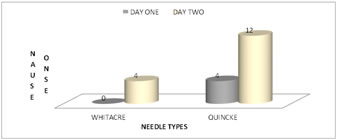
Methods this is a comparative study of 50 patients divided into two groups of 25 each. Patients in Group-A and Group-B were given spinal anesthesia with 25G Whitacre and 25G Quincke needles respectively. Patients were assessed daily for four consecutive days following surgery for post-Dural puncture headache at Vinayaka Missions Kirupananda Variyar Medical College, a Tertiary Care Hospital in Salem in 2019. Patients of ASA I - II aged between18 to 60 yrs. undergoing lower abdominal and lower limb surgeries were included. The procedure was explained to the patients during pre-op visits and a thorough preoperative assessment was done with written informed consent. Inclusion Criteria: Patients within the age group 18-60 yrs. with ASA PS I and II were admitted to the hospital for lower abdominal and lower limb surgeries. Exclusion Criteria: Patients not willing for the sub-arachnoid blockade. Patients with neurological deficits, spinal cord deformities, psychological illness, grossly obese, hypertensive or hypovolemic patients, and patients undergoing multiple pricks. Emergency lower segment caesarian section. Patients with a history of prior headaches. All patients were kept nil per oral for 10 hrs. before surgery. On the day of surgery an appropriate I.V line was secured and I.V. ranitidine 50mg was administered one hour before surgery. On arriving at the operating theatre, a 3 lead ECG monitor, pulse oximeter, and an automated noninvasive arterial blood pressure monitor were applied. Baseline pulse rate, blood pressure, and saturation were noted.10ml/kg of Ringers Lactate was preloaded intravenously before the sub-arachnoid blockade. The sub-arachnoid blockade was performed with 0.5% of Hyperbaric Bupivacaine using 25-G Whitacre in group-A and 25G Quincke needle in group-B at L3-4 intervertebral space. Only an experienced anesthesiologist performed the block. ECG, oxygen saturation and blood pressure was monitored intraoperatively continuously and were recorded every 10 minutes throughout the procedure after the administration of spinal anesthesia. Hypotension was managed with I.V. crystalloids and IV ephedrine and bradycardia with IV atropine. All patients were monitored till 150minutes after the procedure in the postoperative ward and were not mobilized from bed for the first 24 hrs. Postoperatively all the patients were visited successively for 4 days by an investigator blinded to the type and size of the needle used and patients were questioned about post-Dural puncture headache or contacted by telephone if discharged early. Statical analysis:The data obtained were tabulated and analyzed for rates, ratios, and percentages. The test of proportion was used for the incidence of PDPH. Data were analyzed using Treason’s Chi-square test and student t-test as appropriate. ResultsGraph 1: Comparison of Mean Age (Yrs)Graph 1: In the Whitacre group the mean age of patients is observed to be 39.2 years, similarly in the Quincke group also the recorded mean age was 37.5. The difference is not significant. Graph 2: Comparison of the incidence of PDPH between the two groups Graph 2: Eight percent of the study population had a headache in the WHITACRE group while 16% of the study population had a headache in the QUINCKE group. The incidence of headache in the QUINCKE group is twice that of the WHITACRE group. The result is not statistically significant. Graph 3: Comparison of onset of PDPH between the two groups Graph 3: One patient (4%) had a headache in the QUINCKE group on day one while none had in the WHITACRE group. The observation is not statistically significant. Two patients (8%) in the WHITACRE group had a headache while three patients (12%) in the QUINCKE group had a headache on day two. In other words, 40% of the study population had a headache in the WHITACRE group while 60% had a headache in the Quincke group. The observation is not statistically significant. Graph 4: Comparison of onset of nausea between the two groups Graph 4: One patient (4%) had nausea in the QUINCKE group on day one while none had in the WHITACRE group. The observation is not statistically significant. One patient (4%) in the WHITACRE group had nausea while three patients (12%) in the QUINCKE group had nausea on day two. In other words, 25 % of the study population had nausea in the WHITACRE group while 75 % had nausea in the QUINCKE group. The observation is not statistically significant.
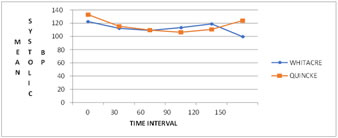
Graph 5: Comparison of mean heart rate between both the groups at different intervals of time Graph 5: There is still a small drop-in heart rate in both groups with a statistical difference of 4 beats per minute between both groups. After 60 minutes there is an increase in heart rate and both the groups have more or less similar mean heart rates (P > 0.05). At 150 minutes there is a statistical difference of 4 beats per minute. Graph 6: Comparison of mean systolic blood pressure between both the groups at different intervals of time Graph 5: At baseline there is a mean difference of 10mmHg which is statistically significant. There is a fall in systolic blood pressure in both groups at the 30th minute. The fall is 8% for the Whitacre group, while there is a 13.2% fall in the quincke group at the 30th minute. There is a nonsignificant mean difference of 3 mm hg between both groups. Still, there is a drop in blood pressure in both the groups at the 60th minute, and the difference is too small between both the groups. After one hour of the start of the procedure, there is an increase in blood pressure and the difference in the increase in significance between both the groups after one hour. Since there is a statistical difference in mean systolic blood pressure between both the groups at baseline, the statistical difference in mean score throughout the study must be read with caution. Graph 6: Comparison of mean diastolic blood pressure between both the groups at different intervals of time Graph 6: When the difference in diastolic blood pressure is measure with the groups, there is not much variation of mean diastolic blood pressure in the Whitacre group through the study. But there is a great fall in mean diastolic blood pressure in the quick group. There is nearly a 20 % drop in diastolic blood pressure in the Quincke group at the 90th minute while there is only a 4 % drop in systolic blood pressure in the Whitacre group. DiscussionSub-arachnoid blockade (SAB) is one of the most commonly used techniques in anesthesia. It is the most common, safe, easy, and needs less sophisticated anesthetic equipment, drugs, and post-operative care. Hence it is preferred over general anesthesia and it is most popular because of profound analgesia and muscle relaxation. The incidence and degree of a headache depend on the size and persistence of the size of the hole in the dura.11 Choosing smaller diameter non-cutting spinal needles will reduce the incidence of post-Dural puncture headache (PDPH). During the last two decades, more refined and thinner needles of 24-28G have been used to reduce the incidence of PDPH preserving the quality of sensory and motor blockade. Leakage of CSF from the punctured sites produces low pressure which in turn results in intracranial dilatation resulting in an increase in intracranial volume in an upright position.12 This results in a difference in CSF volume and the pressure difference between the intracranial and intravertebral parts of the subarachnoid space. Pain arising from the tentorium cerebelli is transmitted via the fifth cranial nerve and from the structures on or below the inferior structures is transmitted via the ninth, tenth, and upper cervical nerves. PDPH caused due to the low pressure of CSF is differentiated from other headaches as it aggravates sitting, standing, moving around, coughing, and straining. Inadequate fluid intake and conditions like diarrhea, vomiting, hemorrhage, sweating, lactation leading to profound dehydration tend to make the condition worse.13 In our observation, we consider that the size of the needle is the most important factor in the development of PDPH. However, extremely thin spinal needles would enhance the failure rate of spinal anesthesia, resulting in multiple Dural punctures and increased incidence of PDPH. Apart from the size of the spinal needle, the shape of the spinal needle is the most important modifiable risk factor of PDPH.14 Pencil point needles are considered to be the most effective way to decrease the incidence of PDPH. The frequency and severity of PDPH are directly related to the rate of CSF leakage through the hole in the dura created by the spinal needle. So in high-risk subjects, the use of thinner needles is advisable.15 Even as the incidence of headache is 0-2% with 29G Quincke needle the failure of spinal anesthesia is common with the use of thinner gauge needle due to technical difficulties (Anirban,2011). Therefore,25G Quincke and Whitacre needles are in use widely and most frequently. We have selected 25G Quincke and Whitacre needles because they are technically easy to use and insert.16 Kang S B and his colleagues Faramarz Mosaffa et.al noted that PDPH was severe enough to require an epidural blood patch. The therapy of epidural blood patches is cumbersome, invasive, and hazardous. Thus, there is no doubt that prevention is a better option than a definitive therapy in the case of PDPH.17 Where in this procedure a small amount of the patient’s blood is injected at the site of puncture into the epidural space, which aids in sealing the meningeal leak. The procedure carries the risk of a Dural puncture. But the release of clotting factors of the blood closes the hole in the dura. In the past 50 years, the development of fine-gauge spinal needles has enabled a significant reduction in the incidence of PDPH. In this study, we compared two different lumbar puncture needle designs with smaller needle diameters.18 This study was an attempt to compare the role of two needles that is 25G Quincke and Whitacre 25 G needles concerning the incidence of PDPH. In this study, the mean age was 39.2±10.87 years in the Whitacre group whereas in the Quincke the mean age was 37.5±9.87 years, where the difference in the mean age group was not statistically significant. There is more or less equal age distribution in both the study groups.19 Although in the elderly age group the incidence of post-Dural puncture headache was not statistically significant when both the needles 25G Quincke and 25G Whitacre were compared, in the young age group the incidence was statistically significant when it came to the type of the needle.20 In the present study, the incidence of PDPH occurred was one female out of a total of 25 patients (4% ) who has aged 30 years and three females out of a total of 25 patients (12%) all the 3 happened to be aged 45 in Whitacre and Quincke groups respectively; whereas one male in each group of a total of 25, each (4%) and both the males happened to be aged about 40 years old. High-level evidence supporting this efficacy.21 In our study 6 out of 50 subjects had PDPH. Among them, 4 out of 6 (66%) women had PDPH, which implies that females are about twice at a higher risk than male subjects (2/6 i.e., 33%). Considering both the groups with 25G Quincke and Whitacre needles in each group the women affected with PDPH are 3 and 1 respectively. Similarly in our study over all who had PDPH was 6.22 In the Quincke group, one patient had a headache on the 1st day and three patients had a headache on the 2ndday.In the Whitacre group, 2 patients had a headache on the 2nd day. Comparing all the studies in most of the cases the onset of PDPH is within 48hrs.In a study conducted by Kuntz KM, et.al there were 60 patients in each group and all groups were comparable about ASA physical status, age, BMI, baseline data, MAP, HR, saturation, and level of block similar to our recordings in our study. The mean heart rate in 25G Quincke needle groups was 85±7post operatively after 150 minutes. Whereas in our study the mean heart rate was 74.46±3.568 postoperatively after 150 minutes in the 25Gquincke group and 71.64±7.38 after 150 minutes in the 25G Whitacre group. After half an hour of the start of the surgery, there was a fall in heart rate in both groups. After 60 minutes there is an increase in heart rate(p>0.005). At 150 minutes there is a statistical difference of 4 beats per minute. Within 3 hrs. for all the patients it was noted that the heart rate came back to normal, so it can be interpreted that the discussion on heart rate is not of much clinical significance.23 Many of the researchers recorded systolic and diastolic blood pressures and found them to be clinically and statistically significant. In our study too we have recorded systolic and diastolic blood pressures at intervals of 0,30,60,90,120,150 minutes, there is no clinical and statistical significance. In a systematic review of studies, the authors have reported that bed rest of any duration after a lumbar puncture has not been shown to decrease the incidence of post–lumbar puncture headache. However, in the present study, the patients who manifested headaches were instructed to remain in the supine position for 24 hrs. which resulted in relieving PDPH. Once the patient had a headache, he was instructed to take complete bed rest.24 All the patients received Inj. Diclofenac Sodium, intramuscular (75-mg) 8 hrly, and hydration therapy with 5 % dextrose 500 ml as an additional fluid within a period of one hr. All the patients responded with this treatment and did not complain of headaches after 24 hrs. While discussing other remedial options epidural blood patch is one of the best treatment modalities for PDPH.25
CONCLUSION Spinal puncture is an important cause of iatrogenic morbidity in the form of post-Dural puncture headache. The incidence of these headaches can be reduced by using thin atraumatic needles in the procedure. Use of Whitacre needle was associated with reduced incidence of post-Dural puncture headache in our study. It is technically difficult to introduce a 25G Whitacre needle. There is a high degree of acceptance on part of the patient with the use of Whitacre needles. 23G and 25G Whitacre needles are associated with a low incidence of post-dural puncture headaches. The cost of the Whitacre spinal needle has to be balanced against the risk of PDPH, the associated cost of longer hospital stays, and the hazardous therapy (Epidural Blood Patch). Thus, there is no doubt, that prevention is a better option than definitive therapy.
References
Policy for Articles with Open Access
|
|
 Home
Home