|
Table of Content - Volume 21 Issue 2 - February 2022
Comparative study to assess the efficacy of bupivacaine with and without dexmeditomidine in ultrasound guided erector spinae plane block in patients undergoing unilateral breast surgery
Priyangadevi S1*, Subbalakshmi Sundaram2, Ragul3
1Junior Resident, 2Professor, 3Assistant Professor, Department of Anaesthesiology, Rajah Muthaiah Medical College and Hospital, Annamalai University, Chidambaram, Tamil Nadu, INDIA. Email: sowmiyadevi123@gmail.com
Abstract Background: Dexmedetomidine a selective α-2 adrenergic agonist has been demonstrated to be safe and efficacious in prolonging the duration of post operative analgesia when added as an adjuvant to local anesthetics in nerve blocks. This study was conducted to assess the efficacy of bupivacaine with and without dexmedetomidine in ultrasound guided Erector spinae plane block in patients undergoing unilateral breast surgeries. Methodology: A prospective randomized double blinded experimental study of forty American Society of Anesthesiologists physical status I and II patients posted for elective unilateral breast surgeries were divided into two groups of twenty each as B group and D group, after satisfying the inclusion criteria. Results: In the present study, demographic data were comparable between both the groups. The duration of analgesia was longer in D group (12.60±2.30 hours) compared to B group (10.72±1.46 hours) and was statistically significant, p<0.05. The mean number of doses of rescue analgesia given in first 24 h was higher in B group (1.50±0.68gms) as compared to the D group (1.05±0.68gms) and was statistically significant, p<0.05. The mean VAS score was higher in B group compared to D group and the difference was statistically significant. Conclusion: This study concludes that patients receiving Bupivacaine with dexmedetomidine in ESP block has prolonged duration of analgesia, lower pain scores, lower total analgesic consumption during first 24 hr. compared to patients receiving plain bupivacaine alone. Key Words: Dexmedetomidine, Erector spinae Plane block, Brest surgery, ultrasound.
INTRODUCTION Breast surgery is one of the commonest surgeries among female population.1 Among those patients only less than half of the population gets adequate pain control. Inadequate pain control will lead to chronic postoperative pain.2 Ultrasound (US)-guided erector spinae plane block (ESPB) is a newer novel analgesic technique introduced by Forero et al.3. Erector spinae plane block provided good postoperative analgesia in patients undergoing breast surgeries as an alternative to other regional techniques like paravertebral block and thoracic epidural.4,5,6 Plain local anesthetics provide postoperative pain relief for only a short duration, and insertion of catheter may not be a viable solution as most of these surgeries are done on a daycare basis. There has been considerable interest in adding adjuncts to local anesthetics, such as clonidine, epinephrine, dexamethasone, tramadol, and midazolam, to prolong the duration and improve the quality of analgesia and hence provide better postoperative pain relief.7 However, only dexmedetomidine has been evaluated as an adjuvant for postoperative pain relief in Erector spinae plane block. Dexmedetomidine a selective α-2 adrenergic agonist has been demonstrated to be safe and efficacious in prolonging the duration of post operative analgesia when added as an adjuvant to local anesthetics in nerve blocks.8,9The present study was planned to compare the postoperative analgesic efficacy of Dexmedetomidine as an adjuvant combined with Ultrasound guided Erector spinae plane block in patients undergoing unilateral breast surgeries. The primary outcome of the study was to measure the duration of analgesia. The secondary outcome includes VAS score, total amount of analgesic requirement for 24 hours following surgery.
METHODOLOGY Our study was conducted as a randomized experimental double blinded study in patients undergoing unilateral breast surgeries at the department of anesthesiology, Rajah Muthiah Medical College, Annamalai university, Chidambaram, Tamil Nādu. The study protocol was approved by the ethics committee for human experiments and informed consent was taken from each of the patients. Forty ASA I and II patients aged 18–60 years undergoing unilateral breast surgery under General Anesthesia were assigned to one of the two groups each containing twenty patients. Group B (Bupivacaine group): patients received 20ml of 0.25% Bupivacaine in ultrasound guided Erector spinae plane block. Group D (Dexmedetomidine group): patients received 20ml of 0.25% Bupivacaine containing 25 micrograms of dexmedetomidine in ultrasound guided Erector spinae plane block. Patients who have ASA >III, BMI >35, coagulation abnormalities, local skin infection, patient refusal, patients allergic to any of study medications and patients with any history of long-term opioid intake were excluded from the study. All the patients were given T. Alprazolam0.5mg, T. ranitidine 150 mg orally on the night before surgery. Glycopyrrolate 0.2 mg was given intramuscularly 45min before surgery. On the arrival to operation theatre, monitors like pulse oximeter, NIBP, ECG were attached. Baseline parameters namely BP, heart rate, SPO2 were recorded. An intravenous line was secured. All patients were preoxygenated with 100 % oxygen for three minutes and were administered 1mcg / kg of fentanyl intravenously. Thiopentone sodium 5mg/kg was used for induction and endotracheal intubation was facilitated with succinylcholine 1–2 mg/kg intravenously. Intraoperative monitoring of heart rate, systolic BP, diastolic BP, SPO2 were done. During surgery, anesthesia is maintained with nitrous oxide 66 % and oxygen 33 %, vecuronium 0.1mg kg as maintenance dose. Fentanyl 0.5 mcg / kg was given every 30 mins during surgery. End-tidal carbon dioxide was maintained at 35–40 mmHg. At the end of the surgery, ondansetron 4 mg was given for prophylaxis against post operative nausea and vomiting. Patients were positioned laterally then under aseptic condition the desired thoracic level of injection is counted from c7 spine downwards. A high frequency linear ultrasound probe is placed in a transverse orientation to identify the transverse process. Once identified, the probe is rotated to the longitudinal orientation to obtain a parasagittal view. The structures seen from above to below include; skin, subcutaneous tissue, trapezius muscle, erector spinae muscle and the tip of the transverse process. The echogenic 22 g needle is inserted in an ‘in plane’ approach from cranial to caudal direction till the needle contacts the transverse process. The correct location of the injection site is confirmed by the spread of saline in the myofascial plane above the transverse process lifting off the erector spinae muscle. Then 20ml of drug is injecting in the space. Residual neuromuscular blockade was reversed with neostigmine 0.05 mg / kg and glycopyrrolate 0.01mg/kg, Extubating was done under thorough suction. Patients were observed in the postoperative period for duration of analgesia from ‘0’ hour which was the time of block for both the groups. Patients were monitored at intervals of 15 min, 30 min, 45 min, 1 h, 4 h, 8 h, 12 h and 24 h from administration of Erector spinae plane block. The pain was quantified on a 10cm visual analog scale (VAS). Time from block administration to time for first request of analgesia was taken as duration of analgesia. At first request for analgesia or when VAS score was more than 4, patient was given Inj.Paracetamol 1gm every 6 hours for 24 hrs. Patients were also monitored for sedation evaluated using (modified Ramsay sedation scale) STATISTICAL METHODS: The results obtained from the study were presented in the following section. The data was entered into Microsoft excel 2017. The data was then imported into SPSS (Statistical package for social sciences) version 23 for analysis. Descriptive stastistics and inferential statistics included mean, proportion and percentages. Inferential statistics included unpaired ‘t’ test, chi square test and repeated measures ANOVA.
RESULTS The demographic factors and operative factors were comparable between the two groups. (Table 1) and were not statistically significant. Table 1: Demographic factors
BMI – Body Mass Index, ASA-American Society of Anesthesiologist
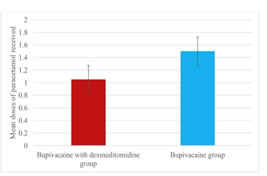
The mean duration of analgesia was longer in D group (12.60±2.30 h) compared to B group (10.72±1.46 h) and was statistically significant, ‘p’ value =0.05 (Table 2) (Fig.1). Total consumption of number of inj. paracetamol doses in first 24h was significantly higher in B group. The mean dose of inj. paracetamol consumed in B group was 1.50±0.68 gm and in D group it was 1.05±0.61gm and was statistically significant, ‘p’ value = 0.05 (Table 2) (fig 2). The mean VAS scores assessed at 4,8,12 hours were similar among both the groups whereas at the end of 24th hour B group had higher VAS score compared to D group. ‘p’ value was significant (p=0.001).
Table 2: Duration of analgesia, total consumption of analgesics in 24h and VAS scores
Figure 1: Bar graph showing duration of analgesia Figure 2: Number of rescue analgesics The hemodynamic parameters – HR, RR, SPO2, SBP, DBP were stable throughout the study.
DISCUSSION Various methods of post operative analgesia have been used in breast surgeries such as opiates, nonsteroidal anti-inflammatory agents, wound infiltration with local anesthetic agents, thoracic epidural, and paravertebral blocks, Serratus anterior block, Pecs I and II block. Erector spinae plane block is one such modality which was first introduced by forero et al. in 2016.3 These blocks are easy, reliable techniques, and are devoid of any sympathetic blockade and consequent adverse hemodynamic effects. In addition, peripheral nerve catheters may be inserted to provide prolonged or continuous analgesia but are associated with drawbacks such as dislocation.10But when a local anesthetic is given as a single shot injection the duration of analgesia may not be sufficient to overcome this researcher have found that adding adjuvant like dexmedetomidine will improve the quality and duration of analgesia.11 dexmedetomidine used in nerve blocks attenuates the bupivacaine-induced acute perineural inflammation.12Thus in this we found that bupivacaine with 25microgram of dexmedetomidine had effective post operative analgesia compared to bupivacaine alone. Kompal Jain, Vikky Jaiswal, Arun Puri (2017) done a case series of erector spine plane block for various surgeries demonstrated that it has wide applications in pain relief ranging from postoperative acute pain in breast surgeries, thoracotomies, and abdominal surgeries to chronic neuropathic pain. They have experienced that ESP block has easily recognizable son anatomy. There are no structures at risk of needle injury in immediate vicinity, making safer with lesser expertise, and no procedural complications as compared to epidural and paravertebral blocks. Swati Singh, Gunjan Kumar, Akhileshwar (2018) done Ultrasound‑guided erector spinae plane block for postoperative analgesia in modified radical mastectomy: A randomized control study shows an effective block for postoperative analgesia in breast cancer surgery. It decreases postoperative morphine requirement. They observed a decrease in postoperative morphine consumption by 65% which was statistically significant, thus establishing its role for analgesia and postoperative opioid sparing effect.13 Mohamed et al. observed that addition of dexmedetomidine 1 μg/kg to bupivacaine in paravertebral blocks for breast cancer surgery prolonged the duration of effective postoperative analgesia and reduced the requirement of analgesics.14 Shaiqa Manzoor and coworkers15 observed that addition of dexmedetomidine to bupivacaine in PECS block increased the duration of analgesia by 40%. Medha mohta16 observed that addition of dexmedetomidine prolonged the duration of local anesthetic action in thoracic paravertebral block and reduced the need of rescue anlage patients undergoing major breast cancer surgery. Helal et al. observed that addition of dexmedetomidine to bupivacaine in a femoral-sciatic nerve block significantly prolonged the duration of sensory and motor blockade by approximately 40%. Time to first analgesic request was 462.5 ± 54.3 min in bupivacaine group and 807.7 ± 112.9 min in dexmedetomidine group.17 Keplinger et al.18 observed a significant dose-dependent increase in the duration of sensory block with dexmedetomidine. Dexmedetomidine in doses ranging from 20 to 150 μg/kg has been used in peripheral nerve blocks. Higher doses of dexmedetomidine may be associated with higher incidence of bradycardia/sedation. In most studies, dexmedetomidine in fixed dose of 100 μg has been used in peripheral nerve blocks. Limitation: VAS score was not observed during movement.
CONCLUSION In conclusion dexmedetomidine prolongs the duration and improves the quality of postoperative analgesia when used as an adjuvant to bupivacaine in ultrasound guided Erector spinae plane block with no serious side effects.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home