|
Table of Content - Volume 21 Issue 2 - February 2022
Dhanabal Da1*, R Gowthaman2, T Santhosh3
1PG, 2Professor, 3Assistant Professor, Department of Anaesthesiology, Rajah Muthiah Medical College & Hospital, Chidambaram-608002, Tamil Nadu, INDIA. Email: docdanbal@gmail.com
Abstract Background: Labour is an extremely painful process. Labour pain can have deleterious effects on the mother, on the fetus and the labor outcome. Epidural analgesia is an effective method of providing analgesia during labor. Bupivacaine and levobupivacaine in lower concentrations are the most commonly used local anesthetics. The potency of local anaesthetic agent is improved by the addition of opioids like fentanyl. Aim And Objective: The aim was to compare epidural bupivacaine and levobupivacaine in intermittent doses for labor analgesia. Materials And Methods: The study was conducted on 60 parturient of Rajah Muthiah Medical College. The study population was divided into 2 groups of 30 each. Group B received bupivacaine with fentanyl 2mcg/ml and Group L received levobupivacaine with fentanyl 2mcg/ml. Sensory and motor block were monitored along with the maternal and fetal outcomes. Results: Among those in the bupivacaine group, 83.3% had a sensory level of T10 and among those in the levobupivacaine group, 80% had an sensory level of T10. In both groups, the distribution of sensory level was similar with a P-value of more than 0.05. The mean Bromage scale among the bupivacaine group and levobupivacaine group was found to be 0.93 ± 0.45 and 0.93 ± 0.45, respectively. The mean Bromage of both the groups was found to be statistically similar with a P-value of more than 0.05. The mean VAS in stage 2 among the bupivacaine and levobupivacaine groups was 2.67 ± 1.18 and 3.10 ± 0.80 respectively. The mean VAS in stage 3 among the bupivacaine group and levobupivacaine group was found to be 1.33 ± 0.66 and 1.23 ± 0.56, respectively. The mean VAS score in stage 2 and stage 3 of both the groups were found to be statistically similar with a P-value of more than 0.05. Conclusion: Both drugs were similar in respect to hemodynamic stability, the onset of analgesia, quality of analgesia, sensory blockade, the requirement of drugs, duration of labor, neonatal outcome and incidence of side effects. Bupivacaine and levobupivacaine provide equivalent analgesia in low (0.1%) concentrations. Keywords: Bupivacaine, levobupivacaine, fentanyl, epidural labour analgesia
INTRODUCTION Labour is an extremely painful process. Labour pain can have deleterious effects on the mother, fetus and labor outcome. Among the various methods of obstetric analgesia, epidural analgesia is the most common technique, which provide the best effectiveness/safety ratio.1 Epidural anesthesia is an effective methods of providing analgesia during labor. Compared with other forms of pain relief, epidural analgesia is associated with maximal level of maternal satisfaction. Despite providing excellent pain relief in epidural labor analgesia using local anesthetic agents only produces a motor block up to 85% of parturients, reduces maternal satisfaction for analgesia and associated with a prolonged second stage and increases the instrumental delivery. Opioid using in epidurally with local anaesthetics provides analgesia in absence of motor block but when used without local anaesthetics does not provide satisfactory pain relief throughout labor.2 Adding an opioid to local anesthetic solutions can provide effective analgesia with lesser local anesthetic requirements and a reduction in the motor block. The local anaesthetics used continuous infusion or intermittent bolus drug (with or without opioid) which causes no measurable outcome differences and provide similar efficacy.3 The local anaesthetic duration and quality of analgesia in epidural is prolonged by adding opioid.4 The efficacy of epidural opioid topups alone is considered inferior to epidural local anaesthetics and the benefits of an epidural opioid should outweigh the side effects such as nausea, pruritus and sedation.5 Combination of local anaesthetics and opioid may increase the duration and quality of pain relief in labor with less motor blockade and offers the smooth progress of labor and vaginal delivery.6
Materials and Methods This study on epidural labor analgesia was conducted on 60 full-term laboring women of Rajah Muthiah Medical College and Hospital Chidambaram. After approval from the institutional human ethics committee, the study was conducted with written informed consent from all patients. Patients were randomly assigned into two groups (B group and L group) of 30 each using sealed envelope method. Subjects in group B received epidural drugs (0.1%Bupivacaine with Fentanyl 2mcg/ml) as 10ml bolus with 5ml top-ups. Subjects in group L received epidural drugs (0.1% Levobupivacaine with Fentanyl 2mcg/ml) as 10 ml bolus with 5ml top-ups. All resuscitation equipment were kept ready, IV access was secured and parturients were hydrated with 500ml of Ringer lactate and oral clear fluid were allowed intermittently. Under aseptic precautions, an epidural catheter was inserted when cervical dilatation reached >3cm with active labor using 18G Tuohy needle in L3-L4 or L4-L5 intervertebral space using the loss of resistance technique and advancing the catheter tip 4-5cm cephalad, parturient placed in supine position with left uterine displacement. The drug was prepared by an anaesthesiologist who was not involved in the study and handed over to the anaesthesiologist performing the study. The following parameters monitored were. 1.HR, NIBP, SP02, RR at 0, 5, 15, 30, 60 min and fifteen minutes thereafter.2.Time of onset of analgesia. 3. Level of sensory blockade with loss of sensation to pinprick. 4. Motor block with Modified Bromage scale 5.Visual analogue pain scale (VAS). 6. Ramsay Sedation Scale 7.Hourly Fetal Heart Rate 8. Duration of labor and mode of delivery. 9. APGAR score at 1 and 5 mins and birth weight of the baby.
STATISTICAL ANALYSIS The data collected was entered into Microsoft excel 2017 to create a master chart. The master chart was then booted into a statistical package for social sciences (SPSS version 23). In the case of quantitative variables, mean and standard deviation were used for describing the data and in the case of qualitative variables, percentages were used. To compare the distribution of qualitative variables between the experimental and control arm and if the expected count is more than 5 in all the cells, then the chi-square test was used. If at least one cell had an expected count of less than 5, fisher’s exact test was used. To compare the mean of the two groups, an independent sample t-test was applied. To analyze those variables which were measured multiple times during the study, Repeated Measures Analysis of Variance (ANOVA) was performed. If there was statistical significance, then a parameter estimate was performed to find out the difference in mean values between the experimental and control arm at various timelines. A p value of less than 0.05 was considered to be statistically significant.
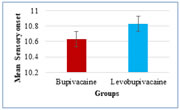
RESULTS Bar chart 1: ONSET of sensory BLOCK (mins) BAR CHART 1 The mean sensory onset among the bupivacaine group and levobupivacaine group was found to be 10.63 ± 1.75 and 10.83 ± 1.41, respectively. The mean sensory onset of both the groups was found to be statistically similar with a P-value of more than 0.05
Bar chart 2: level of Sensory block. BAR CHART 2 Among those in the bupivacaine group, 83.3% had a Sensory level of T10 and among those in the levobupivacaine group, 80% had a sensory level of T10. In both groups, the distribution of Sensory levels was similar with a P-value of more than 0.05.
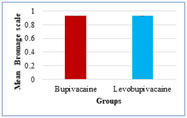
Bar chart 3: Bromage scale BAR CHART 3 The mean Bromage scale among the bupivacaine group and levobupivacaine group was found to be 0.93 ± 0.45 and 0.93 ± 0.45, respectively. The mean BR of both the groups were found to be statistically similar with a P-value of more than 0.05
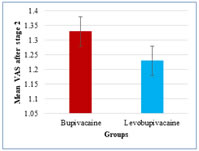
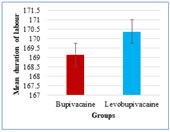
Bar chart 4: Visual analogue scale in stage 3. BAR CHART 4 The mean VAS after stage 1 among the bupivacaine and levobupivacaine groups was 2.67 ± 1.18 and 3.10 ± 0.80. The mean VAS after stage 2 among the bupivacaine group and levobupivacaine group was found to be 1.33 ± 0.66 and 1.23 ± 0.56, respectively. The mean VAS score after stage 1 and stage 2 of both the groups were found to be statistically similar with a P-value of more than 0.05. Bar chart 5: duration of labour BAR CHART:5 The mean duration of labor among the bupivacaine group and levobupivacaine group was found to be 169.13 ± 39.74 and 170.37 ± 34.93, respectively. The mean duration of labor in both the groups was found to be statistically similar with a P-value of more than 0.05.
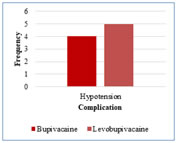
Bar chart 6: complicationS. BAR CHART 6 Among those in the bupivacaine group, 13.3% had hypotension. Among those in the Levobupivacaine group, 16.7% had hypotension. Both the groups were statistically similar concerning complications. DISCUSSION A number of methods exist to provide pain relief to the labouring parturients. Of the regional techniques, epidural analgesia is considered the gold standard among all other techniques and it is the only technique which can provide a complete and convincing pain relief making labour a pleasurable experience. In intermittent bolus dose technique the uniform spread of local anaesthetic in the epidural space leading to superior quality of analgesia allowing parturient mobility and less drugs consumption in intermittent bolus than continuous infusion. Sah N7 et al., who did the study to compare analgesic efficacy of local anaestshetic(0.125% bupivacaine, 0.125% levobupivacaine and 0.2% ropivacaine) with fentanyl in labour epidural analgesia. They found that a mean sensory level of T10 was adequate to maintain analgesia throughout the duration of labour. Purdie NL et al.8, Polley LS et al.9., Sah N et al., did the study to compare 0.1% levobupivacaine and 0.1% ropivacaine in epidural analgesia for pain scores, the results were similar between the groups before and after drug administration. Beilin Y et al.10 did the study to compare the mode of delivery using 0.0625% local anaesthetic with fentanyl 2mcg/ml found no significant difference in the operative delivery among bupivacaine, levobupivacaine and ropivacaine groups. Halpern and Walsh11 et al., did the study to, Compare bupivacaine and ropivacaine for labor epidural analgesia. They found that there was no significant difference in the incidence of spontaneous vaginal delivery and mode of delivery was similar between two groups. Writer et al., Campbell et al.12. found that total drug requirement and hourly drug requirement was similar for bupivacaine and ropivacaine in labor epidural analgesia. Benhamou D et al., Purdie NL8 et al., Beilin Y10 et al. did the study using low concentration of levobupivacaine, ropivacaine with fentanyl, found no adverse effect on neonatal outcome. Apgar score in both groups were comparable without any neonatal depression. This present study demonstrates that solutions containing 0.1% bupivacaine with fentanyl 2mcg/ml and 0.1% levobupivacaine with fentanyl 2mcg/ml are clinically comparable when used to provide epidural analgesia in labor. Demographic factors like age, height, weight is comparable between the two groups and statistically insignificant. Our study failed to show any statistically significant differences in onset and quality of analgesia, duration of analgesia, sensory and motor blockade, local anesthetic consumption, mode of delivery, neonatal outcome and incidence of side effects. The pulse rate and blood pressures (both systolic and diastolic) measured during the study in both groups were statistically not significant. In bupivacaine group 3 parturients went for instrumental delivery and 3 parturients went for caesarean section compared to levobupivacaine group 4 parturients went for instrumental delivery and 2 parturients for caesarean section. No significant difference in mode of delivery in between groups. APGAR score observed at 1 minute and 5 minutes showed neonatal depression not significant.13 In bupivacaine group 4 parturients and in levobupivacaine group 5 parturients developed hypotension, which was managed by intravenous fluids and vasopressor. Complications were minor and easily manageable. The side effects including pruritus, vomiting, hypotension were comparable between groups, with no significant difference in both groups. Several studies comparing levobupivacaine and bupivacaine using 0.125% epidural infusion and 0.25% topups failed to show any differences in motor blockade or analgesia between groups.14 In our study, we achieved in lower concentration (0.1%) the same efficacy, which is similar in both groups. The benefits of levobupivacaine over bupivacaine is the wider therapeutic index for cardiovascular and cns toxicity. The high success rate of spontaneous vaginal delivery was achieved in lower concentrations (0.1%) of bupivacaine and levobupivacaine and produce lesser degree of motor block leading to more active participation in labor.15
CONCLUSION We conclude that at equianalgesic concentrations of Bupivacaine and Levobupivacaine in epidural labour analgesia are equal with regards to the onset of analgesia, quality of analgesia, the incidence of motor block, sensory level achieved, the requirement of a local anesthetic drug, the incidence of instrumental delivery, duration of labor and incidence of side effects. Duration of analgesia, hemodynamic parameters of parturients, mode of delivery and maternal satisfaction was assessed and both drugs were equally effective clinically. Maternal demographic characteristics were comparable. There were no significant differences in visual analogue pain score, sensory block level, maternal satisfaction, mode of delivery, requirement of total dose of LAs during labor and motor blockade between the groups.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home