|
Table of Content - Volume 21 Issue 3 - March 2022
Comparative study of ketamine-propofol in two proportions for short gynecological procedures as sedation and analgesia
P Naveena1, Latha Puroshothama2, Shiladitya Bose3, Senthil Marappan4*
1Assistant Professor, 2,3Post Graduate, 4Associate Professor, Department of Anaesthesiology, Vinayaka Mission's Kirupananda Variyar Medical College & Hospital, VMRF (Deemed To Be), Salem, Tamil Nadu, INDIA. Email: naveenasen@gmail.com, lathapurushotham@gmail.com, shiladityabs@gmail.com, marappansenthil@gmail.com
Abstract Background: Ketofol is most recently practicing procedural and sedation analgesia for the short duration surgical procedures. To assess and compare the two different ratios of intravenous propofol-ketamine combination in minor gynecological procedures with respect to adequate analgesia and sedation, hemodynamic stability, airway intervention, need for supplementation, duration of recovery, emergence phenomena and vomiting. Method: Ninety patients of ASA grade I and II posted for elective minor gynecological procedures were randomly allocated to two groups with 45 patients in each arm. Group A received propofol 2.0mg/kg and ketamine 1.0mg/kg and Group B received propofol 1.0mg/kg and ketamine 1.0mg/kg. Adequacy of sedation was analyzed using Ramsay sedation scale and hemodynamic parameters were recorded. Results: Higher Sedation score, more recovery time, less need for supplemental dose and less emergence phenomena were noted to be statistically significant in group A as compared to group B. A significant 10% higher hemodynamic parameters were noted in patients of group B as compared to patients of group A. Conclusion: Adequate analgesia and better hemodynamic parameters were seen in patients receiving ketofol(1:2) as compared to ketofol(1:1) for short gynecological procedures. Keywords: ketamine, Propofol, Gynecological procedures
INTRODUCTION Patients attending the hospital for any surgical procedure would feel extremely anxious and so it is important to choose the most appropriate form of anesthesia for induction, analgesia, and sedation.1 In anesthesia currently the usage of TIVA (total intravenous anesthesia) has been on a rise by using different type of drugs, making the patient more comfortable, and facilitates the surgeon in completing the surgical procedure without any anesthetic related complications as well as a rapid recovery at the end of the surgery.2 The most recent procedural and sedation analgesia (PSA) combination to be described in the literature is that of low dose ketamine and propofol (Ketofol).3,4 It is postulated that combining these two agents for PSA may preserve sedation efficacy while minimizing their respective adverse effects.5,6 Most studies do attempt to evaluate safety as measured by respiratory and cardiovascular status , very few look at the frequency of other adverse events such as emergence reactions which , if present, may cause practitioners to veer away from ketofol and use an alternate regimen that is more familiar.
METHODS Ninety patients posted for short gynecological procedures such as Dilatation and Curettage, polyp excision, fractional curettage and Bartholin’s cyst excision were included in the study after getting the written consent of the patients and approval by the ethical committee of the institution. The study population includes women aged between 18 and 60 years of ASA I and II posted for short gynecological procedures. The entire study subjects were divided into 2 groups, each consisting of 45 patients. Group A - Propofol 2.0mg/kg + Ketamine 1.0mg/kg Group B - Propofol 1.0mg/kg + ketamine 1.0mg/kg All the study participants received 10mcg/kg of glycopyrrolate and 20mcg/kg of midazolam as premedication drugs, and later they were given the calculated dose of the drug combination after a period of 1 minute as per their group allocation. Once the patient was under deep sedation, the vital parameters were measured every 5 minutes from the time of starting propofol and ketamine intravenous administration and the readings were recorded. Adequacy of sedation was analysed using Ramsay sedation scale. Score of 5 and above was considered as satisfactory and the surgeon was allowed to do the procedure. Time was noted from propofol and ketamine administration to attain a score of 4 or below on the Ramsay Sedation Scale - this was considered as inadequate level of anesthesia and incremental doses of propofol was administered as iv bolus. The effective duration of anesthesia and the amount of supplemental propofol required were recorded. The need for positive pressure ventilation and untoward events like vomiting and emergence phenomena were recorded carefully. Statistical Method: Mean ± standard deviation(SD) was calculated for all the parametric variables and percentage was calculated for all the frequency variables. Statistical inference was derived by applying student T test (unpaired T test) for two continuous variables and chi-square test or Fisher’s exact test for categorical variables. P value <0.05 is considered as as statistically significant. The data were analyzed using Statistical Package for the social Sciences (SPSS version 21)
RESULTS Age wise distribution were similar in both groups and duration of all procedures were less than 30 minutes Table 1: Age wise distribution
The most common gynecological procedures that was done in both groups were dilatation and curettage and fractional curettage. Table 2: Surgical procedures done among the study participants
Table 3: Comparison of study variables in two study group
Sedation score was similar in both groups after 1 minute after the induction of anesthesia. The sedation score was significantly higher in group A after 5 minutes of induction of anesthesia (P value<0.001). Postoperative recovery time was 5.51±0.77 in group A as compared to 4.73±0.74 in group B (P value<0.001). The additional dose requirement of propofol was 22.2% in group A and 48.8% in group B (P value<0.001). Delirium was seen in 16 patients in group B as compared to 3 in group A (P value<0.01). Positive Pressure Ventilation was needed for 3 patients in group A and vomiting was seen in 2 patients in group B, that was not statistically significant.
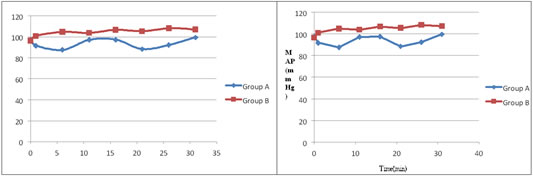
Figure 1: Changes in Heart rate Figure 2: Changes in mean arterial pressure
|
Value |
T0 |
T1 |
T6 |
T11 |
T16 |
T21 |
T26 |
T31 |
SBP |
|
|
|
|
|
|
|
|
Group A |
120.4±18.4 |
118±16.2 |
119.7±16.2 |
119.7±16.2 |
119.2±16.1 |
121.5±15.5 |
119.6±14.8 |
121.3±14.8 |
Group B |
124.6±16.8 |
135.7±16.6 |
138.4±15.5 |
139.4±15.5 |
139.4±15.8 |
140.3±14.8 |
140.3±14.8 |
140.5±14.8 |
p |
0.194 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
DBP |
||||||||
Group A |
83.6±14.4 |
81.4±13.8 |
82.1±14.4 |
83.7±14.4 |
82.7±14.4 |
82.8±13.8 |
82.6±12.9 |
86.5±12.9 |
Group B |
82.9±15.2 |
93.7±14.2 |
98.5±13.8 |
94.4±13.8 |
95.8±13.8 |
93.7±12.8 |
95.1±12.8 |
99.2±12.8 |
P |
0.218 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
HR |
||||||||
Group A |
88.9±12.1 |
88.1±14.2 |
85.6±13.4 |
85.6±13.4 |
89.4±13.8 |
87.8±13.4 |
89.9±14.2 |
90.9±14.2 |
Group B |
91.4±13.5 |
99.2±15.1 |
101.6±14.2 |
101.8±14.2 |
102.3±14.6 |
102.5±13.6 |
102.9±13.6 |
102.6±13.6 |
P |
0.328 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
T0-baseline, T1-1min after induction, T6-6 min after induction, T11- 11min after induction, T16- 16 min after induction, T1616 min after induction, T21-21 min after induction, T26-26 min after induction, T31-31 min after induction, SBP-systolic blood pressure, DBP diastolic pressure, HR-heart rate, Significant P.
DISCUSSION
Our study included 90 patients posted for short gynecological procedures, who were equally allocated to two groups,
Group A- Propofol 2.0mg/kg + Ketamine 1.0mg/kg and
Group B- propofol 1.0mg/kg + ketamine 1.0mg/kg.
Both groups were comparable to baseline characteristics and the duration of procedures. The most common gynecological procedure carried out were missed abortions and dysfunctional uterine bleeding. In the present study considering the hemodynamic parameters we found a rise of around 10% increase in both heart rate and MAP during first minute in group B which was statistically significant (P value<0.001). Similar observation of 10% higher hemodynamic parameters in patients of group B were seen during the period 20 to 30 minutes post injection.7 The increase in HR and MAP were not associated with any adverse cardiovascular effects. These results were similar to the data from the previous studies done by Jouguelet-Lacoste et al., Da Silva PS et al., Aouad MT et al. and Akin A et al.7-9 where they had shown the increase of heart rate and the mean arterial pressure was quite obvious among the group which received lesser doses of propofol because of the cardio-respiratory depression role of the propofol and the sympatho-adrenal activation of the ketamine. Our study did not show any difference in the respiratory rate and SpO2 levels between these two groups. In the current study we found that the sedation score was higher and well maintained (Ramsay sedation score more than 5) throughout the procedure among the patients who received higher dose of propofol (group A) compared to the group which received a lower dose of propofol and this difference was found to be statistically significant (p<.05). Saeed et al. and Sharieff et al. had shown that ketofol in the ratio of 1:2 (ketamine 1mg/kg: propofol 2mg/kg) provided effective sedation with a higher sedation score and also with a rapid recovery profile.10,11 In our study it was shown that among the patients who received the ketofol in the ratio of 1:2 only 3 patients required a positive pressure ventilation during the procedure and the difference was not found to be statistically significant. Hui and co-workers and Mortero and co-workers had also shown a similar type of findings in their study.[12,13] The addition of low dose ketamine to propofol improves ventilation and reduces the risk of respiratory depression and also reduces the additional anesthetic drug requirement, which might be due to ketamine-induced sympathoadrenal activation.14-16 Emergence reaction (delirium) during recovery in the form of confusion, shouting, hyperirritability, irrelevant talks and repeated tongue movements were noted in 6.6% in group A compared to 35.5% in group B and the difference was found to be statistically significant between the two groups. So a high dose combination of propofol with ketamine had shown a reduced incidence and intensity of emergency delirium which was on par with the studies by Mortero and co-workers and Sicignano and co-workers.13,17 In the present study only 2 patients in group B developed vomiting and so it was found that nausea and vomiting did not show any statistical significant association between the groups. The additional dose requirement of propofol was 22.2% in group A and 48.8% in group B; This is because of the lesser dose of propofol given as loading dose in group B and the difference between the group was found to be statistically significant. In our study the post-operative recovery time in group A was higher (5.51 mins) compared to group B (4.73 mins) and the difference was found to be statistically significant (p value<0.001). This increase in the recovery time in group A is because of the higher dose of propofol given in group A.
CONCLUSION
Adequate analgesia and better hemodynamic parameters were seen in patients receiving a combination of propofol 2mg/kg +ketamine 1mg/kg as compared to patients who received Propofol 1mg/kg+ ketamine 1mg/kg for short gynecological procedures.
REFERENCES
- Soleimanpour H, Mahmoodpoor A, Eftekhari Milani F, Shahsavari Nia K, Mehdizadeh Esfanjani R, Safari S. Effectiveness of oral ketamine, midazolam, and atropine cocktail versus oral diphenhydramine for pediatric sedation in the emergency department. Iran Red Crescent Med J. 2014;16(9):e21366
- Aaa Bellolio MF, Gilani WI, Barrionuevo P, Murad MH, Erwin PJ, Anderson JR. et al. Incidence of Adverse Events in Adults Undergoing Procedural Sedation in the Emergency Department: A Systematic Review and Meta-analysis. Acad Emerg Med. 2016;23(2):119–34
- Rai K, Hegde AM, Goel K. Sedation in uncooperative children undergoing dental procedures: A comparative evaluation of midazolam, propofol and ketamine. J Clin Pediatr Dent 2007;32:1-4
- G Kip, D Atabek, M Bani. Comparison of three different ketofol proportions in children undergoing dental treatment. Nigerian Journal of Clinical practice. 2018;vol 21 (11), 1501-07
- Akin A, Guler G, Esmaoglu A, Bedirli N, Boyaci A. A comparison of fentanyl-propofol with a ketamine-propofol combination for sedation during endometrial biopsy. J Clin Anesth 2005;17:187-90
- Daabiss M, Elsherbiny M, AlOtibi R. Assessment of different concentrations of Ketofol in procedural operation. Br J Med Pract 2009;2:27-3
- Da Silva PS, de Aguiar VE, Waisberg DR, Passos RM, Park MV. Use of ketofol for procedural sedation and analgesia in children with hematological diseases. Pediatr Int 2011;53:62-7
- Aouad MT, Moussa AR, Dagher CM, Muwakkit SA, Jabbour-Khoury SI, Zbeidy RA, et al. Addition of ketamine to propofol for initiation of procedural anesthesia in children reduces propofol consumption and preserves hemodynamic stability. Acta Anaesthesiol Scand 2008;52:561-5
- Jouguelet-Lacoste J, La Colla L, Schilling D, Chelly JE. The use of intravenous infusion or single dose of low-dose ketamine for postoperative analgesia: A review of the current literature. Pain Med 2015;16:383-403
- Saeed E. Ketofol infusion as a procedural sedation and analgesia modality for minor orthopedic surgeries: Evaluation of dose-outcome relation. Ain Shams J Anaesthesiol 2011;4:63-74
- Sharieff GQ, Trocinski DR, Kanegaye JT, Fisher B, Harley JR. Ketamine-propofol combination sedation for fracture reduction inthe pediatric emergency department. Pediatr Emerg Care 2007;23:881-4
- Hui TW, Short TG, Hong W, Suen T, Gin T, Plummer J. Additive interactions between propofol and ketamine when used for anaesthesia induction in female patients. Anaesthesiology 1995; 82:641-8
- Mortero RK, Clark LD, Tolan MM et al. The effects of small dose ketamine on propofol sedation, respiration, postoperative mood, perception, cognition and pain. Anesth Analg 2001; 92:1465-69
- Hashemi A, Ayatolahi V, Ghilian R, Ghadami Yazdi A, Fadavi N, Yadegari Y, et al.
- Ketofol for bone marrow aspiration and lumbar puncture in children with all. Iran J Pediatr Hematol Oncol 2011;1:126-32
- Goh PK, Chiu CL, Wang CY, Chan YK, Loo PL. Randomized double-blind comparison of ketamine-propofol, fentanyl-propofol and propofol-saline on haemodynamics and laryngeal mask airway insertion conditions. Anaesth Intensive Care 2005;33:223-8
- Khutia SK, Mandal MC, Das S, Basu SR. Intravenous infusion of ketamine-propofol can be an alternative to intravenous infusion of fentanyl-propofol for deep sedation and analgesia in paediatric patients undergoing emergency short surgical procedures. Indian J Anaesth 2012;56:145-50
- Sicignano A, Bellato V, Cancelleri F, Foroni C, giubelli D, Moro D, Vesconi S. Propofolketamine vs propofol-fentanyl in short gynaecologic surgery. Minerva Anestesiol 1990 Mar; 56:61-6.
Policy for Articles with Open Access
Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms:
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
 Home
Home