|
Table of Content - Volume 21 Issue 3 - March 2022
Jigisha P Badheka1, Nitin Manat2*, Vrinda P Oza3, Yash Bhorania4
1Associate Professor, 2Senior Resident, 3Assistant Professor, 4Junior Resident, Department of Anaesthesiology, P.D.U. Medical College, Rajkot -360001, INDIA. Email: jagu_jigi@yahoo.com, drnitinmanat1199@gmail.com, vrinda.agravat@yahoo.com, ycbhorania@gmail.com
Abstract Background: Femoro-sciatic nerve block (FSNB) are used for providing anaesthesia and postoperative analgesia for lower limb surgeries. Sciatic nerve can be blocked by various approaches. Our aim of the study was to compare ease, time of performance and success rate of sciatic nerve block by posterior sub-gluteus approach with the classic posterior approach along with a femoral block for lower limb surgeries using peripheral nerve stimulator (PNS). Methods: Sixty patients belonging to ASA grade I, II, III, aged 18-65 years, either sex scheduled for lower limb surgery were randomly allocated in two groups Group L: Labat’s posterior approach and Group S: Sub-gluteus approach for sciatic nerve block. Femoral nerve block was given in both the groups. Result: The time from needle insertion to sciatic stimulation was 60 sec in Group L and 32 sec in Group S (P < 0.0001). Depth in cm was 67±12 and 45±13 in Group L and Group S respectively (P < 0.0001). The number of attempts to perform block in Group L was 1.97±1.12 and 1.3±0.59 in Group-S (P<0.005). The onset time of sensory and motor block were not statistically significant. The discomfort during the procedure was less in Group S compared to Group L. In Group L 5 patients [16.6%] and 2 patients [6.6 %] in Group S required intraoperative analgesia. Conclusion: PNS guided posterior sub-gluteus approach for SNB can be considered as a safe, reliable and useful alternative, requires lesser time to perform the block, lesser attempts and less discomfort compared to the Labat’s classic approach of sciatic nerve block. Key words: Femoro-sciatic nerve block, Labat’s classic approach, sub-gluteus approach, peripheral neve stimulator, lower limb surgeries
INTRODUCTION Peripheral nerve blocks (PNB) are a useful technique for providing anesthesia for lower limb surgeries that avoid haemodynamic instability and pulmonary complications; facilitate postoperative pain management and early discharge. For lower limb surgeries, femoro-sciatic nerve block (FSNB) is widely used and sciatic nerve can be blocked at different levels along its pathway. Several approaches have been described that depend on the position of the patient- Posterior, lateral, anterior approaches.1-5 The classic approach of Labat’s1 is the most frequently used requires the identification of multiple landmarks; the stimulating needle has to pass through different layers of muscles, often causing discomfort to the patient during the block. Sub-gluteus approach2 is a new posterior approach that requires fewer identification landmarks the stimulating needle has to pass through fewer layers of muscle. Various studies have compared any of the five approaches. In literature review very few studies3,9 compared Labat’s posterior approach with sub-gluteus approach. There are various techniques for PNB like landmark guided, use of peripheral nerve stimulator (PNS), and use of ultrasonography. Despite the extensive use and acceptability of ultrasonography (USG) in regional anesthesia in recent times, PNS is also widely accepted, allows for exact nerve location without eliciting paraesthesia and has potential benefits like it is technically simple with minimal expertise, higher success rate and better localisation of nerve trunks in difficult situations. Use of PNS is a boon in tertiary care centers as well as small scale private centers where there is non-availability of USG machine because of cost, legal issues and strict law of PCPNDT.6 Our aim of the study was to compare the ease and time of performance and effectiveness of sciatic nerve block by posterior sub-gluteus approach with the classic posterior approach along with a femoral block for lower limb surgeries using peripheral nerve stimulator (PNS). The objective of the study was to compare the depth of needle and number of redirection and characteristics of block
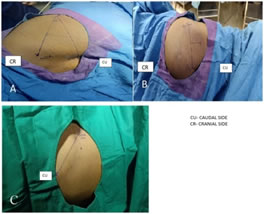
MATERIALS AND METHODS After approval from institutional ethical committee (PDUMCR/IEC/17669/2018), we conducted a prospective randomised comparative study in anaesthesiology, orthopedic and general surgery department at Government medical college, during the period between September 2018 to February 2020. We followed CONSORT guidelines. The study was carried out on sixty adult patients American Society of Anaesthesiologist (ASA) class I – III, aged 18-65 years, scheduled for lower limb surgeries under sciatic nerve block with classic posterior approach and posterior sub-gluteus approach along with femoral nerve block. We took informed consent from all the patients undergoing the study. Those patients having a history of drug allergy, diabetic patients with peripheral neuropathies, neuromuscular diseases, bleeding disorder, and infection at the local site were excluded from the study base. The sample size was calculated based on previous study3which 94% patients had a better acceptance in group sub-gluteus approach and accordingly sample size was calculated to be 26 in each group and considering the dropouts we have taken 30 patients in each group. Pre-anesthetic check-ups and routine investigations were carried out for all patients. Standard monitoring was done with non-invasive blood pressure (NIBP), heart rate, and pulse oximeter. After securing the intravenous cannula all the patients were premedicated inj. dexmedetomidine 1 mcg/kg given, and a crystalloid infusion was given at 5 ml/kg/hr. All the blocks were performed by an expert anesthesiologist by using a peripheral nerve stimulator (Plexygon, Vygon, Ecouen, France nerve stimulator). We took 10 cm and 5 cm long 20-gauge short beveled teflon coated insulated stimulating needle for sciatic nerve and femoral nerve block respectively. Patients were randomly selected as per randomization number. Randomization done with computer generated randomized numbers randomly allocated into two groups of 30 each. The group allocation number were concealed in sealed opaque envelopes. Group L: Classic posterior Labat’s approach for sciatic nerve block with a femoral nerve block. Group S: Posterior sub-gluteus approach for sciatic nerve block with femoral nerve block. Local anesthetic agents consisting of Inj. lignocaine + adrenaline (L+A) 2% 20 ml, Inj. Bupivacaine (0.5%) 20 ml and Inj. normal saline 10 ml making a total 50 ml, out of the mixture 25 ml used correspondingly at each site for blocking the femoral and sciatic nerve. Patients were placed in the lateral position with the side to be blocked uppermost. While the lower leg was kept straight, the upper leg flexed at the knee so that the ankle was brought over the knee of the lower leg in both groups. In Group L, the important landmarks the greater trochanter (GT), posterior superior iliac spine (PSIS), sacral hiatus were marked. A line was drawn between GT and PSIS. From the midpoint of this line, at the right angle to it, a second line is drawn passing down over the buttock. The point of injection was 3-5 cm along this perpendicular line. It can be more precisely identified by drawing third line intersecting with the second line between GT and sacral hiatus, the point of injection is where the third line intersects with the second line.1 [Fig.1A] In Group S, the approach line was drawn from GT to the ischial tuberosity (IT). From the midpoint of this line, a second line was drawn perpendicularly and extended caudally for 4 cm. A skin depression (groove between the biceps femoris and semitendinosus muscles) represents the site for needle entry. The stimulating needle was inserted with a 90-degree angle to the skin.3 [Fig 1B]. After locating the injection point, a standard 10 cm insulated needle was inserted at the right angle to the skin to elicit a response to the sciatic nerve stimulation. Needle advanced till appropriate muscle twitch common peroneal nerve (dorsiflexion and eversion of the foot) and tibialis nerve (plantar flexion and inversion of the foot) at a stimulating current ≤0.5 mA after that local anesthetic drug given slowly after aspiration every 5 ml. Total 25 ml local anaesthetic mixture used for sciatic nerve block. In both the groups, Femoral block also was given with 5 cm insulated PNS needle. After keeping the patient in supine position, the puncture site was marked [ Fig 1C] at 1-2 cm below the inguinal ligament and 0.5-1 cm lateral to the femoral artery pulsation. The needle is introduced immediately at the lateral border of the artery and advanced in the sagittal and slightly cephalad plane. The nerve stimulator is initially set to deliver 1.0 to 1.5 mA with proper needle position the advancement of the needle should not result in any local twitches; the first response is usually that of the femoral nerve, dancing patella sign. After an aspiration that is negative for blood, 25 ml of local anesthetic is slowly injected. Standard monitoring was done with non-invasive blood pressure (NIBP), heart rate, and pulse oximetry. We have recorded the time from needle insertion into the skin to successful elicitation of the appropriate motor response (performance time), the number of needle redirections required, the depth at which the sciatic nerve stimulation was elicited, the time from the end of injection to readiness to surgery (onset time), Sensory and motor blocks were evaluated every 5 min after block to check for the adequacy of surgical anesthesia. The patient was ready for surgery after complete loss of pinprick sensation in both the tibial and common peroneal nerve distributions. Assessment of sensory block was done by pin-prick in an area innervated by Femoral nerve (L2,3,4), Sciatic nerve (L4,5, S1,2,3) for every 2 minutes for initial 10 minutes and then every minute till completion of sensory block. 3-point scale for sensory block: Normal sensation = 0, Blunt sensation = 1, No perception=2. Onset time for sensory block: Time from an injection of LA to point 1 scale. Duration of sensory block: time from onset to first analgesic demand by the patient. Motor block was evaluated by examining the following responses. Inability to plantar flex the foot against resistance indicates sciatic nerve blockade. Inability to extend the knee against resistance indicates a successful femoral nerve block. The nerve block was considered as adequate/ inadequate depending on analgesic/sedation required during surgery. We have used 50mcg IV boluses of fentanyl for inadequate analgesia. Duration of analgesia, perioperative complication, supplementary IV analgesics, and sedation were recorded. After the block, patients were asked to grade the discomfort experienced during the procedure, by using a three-point scale (1- mild painful; 2 -moderately painful; 3 -extremely painful). Data were collected and entered in MS Excel 2010.Statistical analysis was performed using SPSS version 21 for Windows. Continuous and categorical variables were presented as the mean ± standard deviation and frequencies (percentage of patients) respectively. A student unpaired t-test for independent variable or a repeated measure, and chi-square test for categorical data used for analysis. The P-value <0.05 was considered statistically significant.
RESULTS Table 1: Comparison of demographic data
Table 2: Characteristic of Block
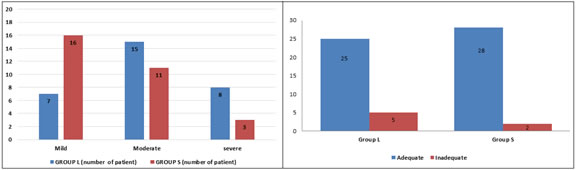
Data are presented as mean ± SD, p < 0.05 was considered statistically significant. Total of 60 patients were enrolled and randomly allocated and analysed into two groups: Group L (n=30) and Group S (n=30) [Figure 2]. Both the groups were comparable demographically [Table 1]. The time from needle insertion to proper sciatic stimulation (performance time) in Group L was 64.70±14.20 sec and 34.13±12.25 sec in Group S [p˂0.05].The depth of the needle for sciatic stimulation in Group L was 5.38±0.71 cm and 4.72±0.76 cm in Group S [p=0.0001].Number of redirections to perform block 1.97±1.12 in Group L and 1.3±0.59 in Group S [p=0.0053].The onset time for sensory and motor blocks was similar in those patients receiving the Group L 9.80±2.11 min and 16.07±2.75 min respectively and in group S the 8.57±2.94 min and15±2.94 min respectively [p=0.0677 and p=0.1508]. Also, the duration of analgesia was comparable in both the groups. [Table 2] The discomfort during the procedure was markedly less in Group S compared to Group L. [Figure 3]. Out of 30 patients in Group L and group S, 25 and 28 patients respectively had adequate block. While 5 patients in group L and 2 patients in group S required intraoperative analgesia [Figure 4] There was no immediate or delayed complication related to FSNB in the study group.
Figure 1 Figure 1: Landmark of (A) The Classic Posterior Labat Approach: First line drawn from the posterior superior iliac spine (PSIS) to the midpoint of the greater trochanter (GT). Second line drawn from the sacral hiatus (SH) to the midpoint of the first line bisecting the second line. The intersection of these two lines indicated the point of needle entry. (B) The Posterior Subgluteus Approach: The greater trochanter of the femur, the ischial tuberosity, and a line between the midpoint marked. From the midpoint, another line is drawn perpendicularly and extended 4 cm in the caudal direction to identify the needle insertion point. (C) The Femoral Nerve Block: The needle entry point is located 1-2 cm below the inguinal ligament and 0.5 -1 cm lateral to the femoral artery pulsation
Figure 2: Consort flow diagram
Figure 3 Figure 4 Figure 3: Comparison of discomfort at time of needle insertion between the groups; Figure 4: Comparison of quality of blocks between the groups
DISCUSSION The peripheral nerve block (PNB) can be confined to the regional area without affecting the sympathetic nervous system of the patients and provides better haemodynamic stability. It provides stress-free anesthesia because many perioperative complications are the consequences of stress responses to surgery, especially in patients with chronic diseases. Different approaches to the sciatic nerve have been described in the literature.1-5 Labat’s classical1 is most often used it may be quite painful because of the thick layer of muscles through which the stimulating needle passes. The stimulating needle passes through less layer of muscle in sub-gluteus approach, hence there is less pain, discomfort and also less time to perform than the classical approach.3 Davies7 have shown that without nerve stimulator sciatic nerve blocks are frequently unsuccessful. Therefore, the vast majority of sciatic nerve blocks are performed using nerve stimulators. A Study using USG guided FSNB with or without nerve locator and concluded that adding nerve locator to the USG guided block has minimal impact on the efficacy of the technique.8 In our study, we have used PNS for each case. The femoral nerve block is easy to perform and fewer chances of complications and has significant clinical applicability for surgical anesthesia anterior thigh and postoperative pain management after knee surgery. When combined with the sciatic nerve block, anaesthesia of almost the entire lower limb from mid-thigh level can be achieved. We have used combined FSNB for each case in our study. Performance time from needle insertion to proper sciatic stimulation in Group L was 64.70±14.20 sec and 34.13±12.25 sec in Group S [Table 2] Longer time for performing classic posterior approach to sciatic nerve block was due to identification of multiple landmarks, and the stimulating needle has to pass through different layers of muscles and in sub-gluteus approach, only two landmarks are required instead of three and the stimulating needle has to pass through fewer layers of muscles. Our results were similar to Di Benedetto.3 Junichiota8 and Radha Sukhani9 found the time taken to perform i.e. total procedure time was 6 ±3 minutes in posterior and infra-gluteal parabiceps approach. In our study, depth of needle insertion was less 4.72±0.76 cm in sub-gluteus approach and was 5.83±0.71 cm in classic approach (P value is<0.0001). Similar results were found by Di Benedetto,3 where the depth of needle insertion in the posterior sub-gluteus approach was 4.5±1.3 cm and 6.7±1.2 cm in Labat’s approach. In study by Radha Sukhani,7 they used infragluteal-parabiceps approach where a depth of needle insertion was 5.5±1.5 cm. The reduced depth and less discomfort in sub-gluteus approach depend on adipose tissue and less overlying muscle in gluteus region. The needle entry site was the lower limit of the gluteus maximus muscle probably due to the shallower depth at which the sciatic nerve was identified. The reason may be the same as for a reduced number of attempts. The number of attempts required for SNB in present study was also less in Group S 1.3±0.59 compared to Group L 1.97±1.12 [p=0.0053]. Similar to our study Di Benedetto3 identified sciatic nerve at 4.5 cm in sub-gluteus approach and 6.7 cm in Labat’s approach and also required fewer attempts for sub-gluteus approach was 2 (1-7) and 4 (1-10) for Labat’s approach. The onset time of sensory, motor block and duration of analgesia were statistically comparable between our study groups. Earlier studies3,11,12 have also found similar onset times for sensory and motor block. The onset of blockade was less predictable in sciatic nerve than other peripheral nerves because of its large size. Various factors markedly affect the onset time of peripheral nerve blocks. These include the concentration and volume of the injected anesthetic solution, the use of additives, the type of evoked motor response obtained, and the intensity of the current at which peripheral nerve stimulation is achieved. Because of all these factors were kept constant in our study two groups. As per Figure 3, discomfort at the time of needle insertion was higher in Labat’s approach compared with sub-gluteus approach and comparable with results of Di Benedetto.3 Effect of FSNB in 25 patients in Group L and 28 patients in Group S was adequate. Analgesia was given with inj. Fentanyl in 5 patients [16.67%] in the Labat’s approach and 2 patients [6.67%] in sub-gluteus approach. In sub-gluteus approach small intermuscular space between the greater trochanter and ischial tuberosity, within which the sciatic nerve is at the sub-gluteal level14 and the minimal amount of connective tissue surrounding it, could have improved nerve impregnation with local anesthetic solution as compared to Labat’s approach and hence reduced analgesic supplementation was observed in sub-gluteus approach. A limitation of our study, blinding was not possible during the performance of the procedure, to check the sensory, motor characteristics as well as intraoperative efficacy as this leads to bias result towards sub-gluteal approach. Another limitation of the study is difficulty in lateral position in polytrauma patients. Patients belonging to the high-risk category (old age, morbidly obese, haemodynamically unstable, ASA grade IV, V) can be studied further by randomised trials using the posterior sub-gluteus approach.
CONCLUSION We conclude that PNS guided posterior sub-gluteus approach is a reliable and useful alternative for sciatic nerve block (SNB) and requires lesser time to perform, less no of redirections of needle and less discomfort during procedure as compared to Labat’s classical approach of SNB.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home