|
Table of Content - Volume 21 Issue 3 - March 2022
Comparison of Dexamethasone and Dexmedetomidine as adjuvants for TAP block for postoperative analgesia after abdominal hysterectomy under spinal anaesthesia
Mehul T Suratwala1*, Sonali A Joshi2
1IIIrd Year Resident, 2Assistant Professor, Department of Anaesthesiology, SMIMER Medical College, Umarwada, Surat, Gujarat-395010, INDIA. Email: mihirsuratwala1992@gmail.com
Abstract Background: Abdominal hysterectomy is usually associated with considerable pain during the postoperative period , which may affect multiple systems and induce physiological, immunological, and psychological changes. Adequate postoperative analgesia causes reduction in the postoperative stress response and postoperative morbidity. TAP block as a regional analgesic technique reduces pain intensity, decreases in the incidence of side effects from analgesics and improved patient comfort. Adjuvants are used to intensify the quality and increase the duration of local anesthetics in TAP block. Aims And Objectives: Compare the efficacy of Dexamethasone and Dexmedetomidine as adjuvants for TAP block for postoperative analgesia after abdominal hysterectomy under spinal anaesthesia. Materials And Methods: 52 patients of ASA grading I and II, aged between 18-60 years undergoing elective abdominal hysterectomy under spinal anaesthesia were randomly divided in two groups A and B of 26 each. Group A patients received Inj. Bupivacaine 0.25% 20 ml + Inj. Dexamethasone 4 mg + 1 ml normal saline in TAP block on each side at the end of surgery. Group B patients received Inj. Bupivacaine 0.25% 20 ml + Inj. Dexmedetomidine 25 μg + 1 ml normal saline in TAP block on each side at the end of surgery. Assessment parameters included hemodynamic, postoperative VAS score, duration of postoperative analgesia, total dose of postoperative rescue analgesia and side effects. Results: In the first 24 hrs postoperative VAS score was lower in group A compared to group B. Duration of postoperative analgesia was longer in group A compared group B. Total dose of postoperative rescue analgesia consumption in 24 hrs was lower in group A than in group B. Conclusion: Dexamethasone as an adjuvant to Bupivacaine in TAP block has prolonged postoperative analgesia and has reduced requirement of rescue analgesia than Dexmedetomidine following abdominal hysterectomy under spinal anaesthesia. Keywords: Dexamethasone, Dexmedetomidine, Postoperative analgesia, Transverse abdominis plane block.
INTRODUCTION Hysterectomy is a frequent surgery performed in women. Due to substantial incision and soft tissue undermining associated with this operation, it could result in moderate to severe postoperative pain which affects multiple system and induces physiological, immunological and psychological changes.13 Successful management of postoperative pain can have an impact on patient’s quality of life. Neuraxial block has many advantages over general anaesthesia like easier to perform, rapid onset of acion and good muscle relaxation. One of the main disadvantage is its limited duration of action and hence lack of postoperative analgesia.14 Traditionally NSAIDs or opiods used for postoperaive analgesia, however the use of systemic analgesics is confined for short period of time and associated with frequent side effects, including gastrointestinal problems, kidney dysfunction, nausea and vomiting and reduced bowel motility.3 There are different modalities to reduce the postoperative pain of lower abdominal surgery including systemic analgesia with NSAIDs, opioids, intravenous patient controlled analgesia and regional analgesic techniques like port site local anaesthestic infiltration , patient controlled epidural analgesia and transverse abdominis plane block. Transeverse abdominis plane (TAP) block as a regional analgesic technique for postoperative analgesia is very useful in major abdominal surgeries. Transverse abdominis plane containing the thoraco-lumbar nerves originating from T6 to L1 lies between the internal oblique and transverse abdominis.4 Adjuvants are used to intensify the quality and increase the duration of local anaesthetics in different regional block techniques.Dexamethasone,tramadol,buprenorphine,clonidine,dexmedetomidine have been used as adjuvants for transverse abdominis plane block for postoperative analgesia for lower abdominal surgeries.6 Dexmedeomidine,alpha-2 adrenergic receptor agonist is very useful due to sedative, analgesic and hemodynamic stabilizing properties and prolonged postoperative analgesia with minimal side effects. Site of action of Dexmedetomidine are prejunctional and postjuctional alpha-2 receptors present in dorsal horn of spinal cord. Activation of presynaptic receptors reduces neurotransmitter release, whereas postjunctional receptor activation results in hyperpolarization and reduction of pulse transmission. It has a relatively high ratio of alpha-2 / alpha-1 activity (1620:1) and lack respiratory depression making it a safe adjuvant.7 Dexamethasone is also used as an adjuvant. Steroid potentiate the action of local anaesthetic through modulation of K+ channels in excitable cells and also by vasoconstriction, which decreases the absorption of local anaestheic solution. Alternatively, Dexamethasone blocks nociceptive impulse transmission along unmyelinated C- fibers through its antiinflammatory and immunosuppressive effect. After intracellular uptake, glucocorticoid activate cytoplasmic receptors that bind to their response elements in DNA. Hence decreasing the production of inflammatory proteins and increasing production of anti-inflammatory proteins.9 This study is designed to compare Dexamethasone and Dexmedeomidine as an adjuvant for trasnverse abdominis plane block after abdominal hysterectomy under spinal anaesthesia.
MATERIALS AND METHOD After obtaining written and informed consent, we conducted a randomised study in 52 patients and compared the efficacy of Dexamethasone and Dexmedetomidine as adjuvants for TAP block for postoperative analgesia after abdominal hysterectomy under spinal anaesthesia. Patients were divided randomly in two groups with 26 patients in each group. Patient’s inclusion and exclusion criteria: Inclusion criteria: Patients belonging to ASA Classes I or II. Patients aged between 18-60 years. Patients who give a valid informed consent. Patients posted for elective abdominal hysterectomy under spinal anaesthesia. Exclusion criteria: Patients who did not give a valid informed consent. Patients not belonging to the above mentioned age or ASA grade. Allergy to study drug. Contraindication to spinal anaesthesia. Chronic analgesic users Patients with cardiovascular disease. Patients using adrenergic receptor blockers, calcium channel blockers. Preanaesthetic evaluation: Preanaesthetic evaluation of all patients consisted of detailed history, physical examination and routine investigation. A written informed consent was taken after proper counselling. Anaesthetic protocol: Preoperative preparation: Patients were explained about procedure and informed consent was taken. I.V. line was secured. Preloading was done with Inj. Ringer Lactate 10-15 ml/kg I.V. Preoperative vitals were recorded. Pre-operative vitals: Temperature: Pulse: Blood pressure: MAP: SpO2: Premedication: Inj. Glycopyrolate 0.01 mg/kg Inj. Ondensatron 0.1 mg/kg Anaesthetic technique: Monitors attached – pulse oximeter, NIBP, ECG Vital parameters noted and monitoring was done throughout the procedure. Subarachnoid block was instituted: under strict aseptic and antiseptic precaution. in sitting position. in L3-L4 intervertebral space. with 25G quincke’s spinal needle. 4 ml of 0.5% hyperbaric Bupivacaine was used in all cases, to achieve a desirable level of sensory block in accordance with the surgical procedure. Onset of sensory block was assessed by pinprick method. Motor block was assessd according to modified bromage scale. Surgery was allowed once desired sensory block level and motor block of modified bromage grade 3 was achieved. At the end of surgery, TAP block was administered in both the groups with doses as described below: Group A: Patient received Inj. Bupivacaine plain 0.25% 20 ml + Inj. Dexamethasone 4 mg + 1 ml normal saline in TAP block on each side. Group B: Patient received Inj. Bupivacaine plain 0.25% 20 ml + Inj. Dexmedetomidine 25 μg + 1 ml normal saline in TAP block on each side. Postoperative observation: Pain was assessed postoperatively at 0,2,4,8,12 and 24 hours using a VAS Score. At any time during postoperative period if the VAS score is equal to or more than 4, rescue analgesia of tramadol 1 mg/kg was administered iv and time of administration noted and that time was calculated as total duration of postoperative analgesia. The total dose of consumption of rescue analgesia in first 24 hours was recorded. Any side effects like nausea or vomiting were recorded. Figure 1: VAS Score
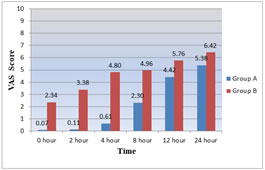
OBSERVATION AND RESULTS After studying 52 cases, observation and results were summarized in chart form and described below. Both groups comprised of 26 patients. Statistical Method: t test for quantitative data and chi square test for qualitative data A P value of <0.05: significant, >0.05 : non significant We observed that both the groups were comparable with respect to demographic data. The mean age in Group A was 46.8 ± 4.3 and in Group B was 47.1 ± 4.5.The mean body weight in Group A was 57.8 ± 5.4 and in Group B was 58.3 ± 6.1. TABLE 1: VAS SCORE
Graph 1: VAS SCORE Patients in Group A had lower mean VAS scores than those in Group B at all time intervals and statistically significant difference were observed at 0,2, 4, 8, 12, and 24 hours. (p < 0.05) Table 2: Duration of Postoperative Analgesia
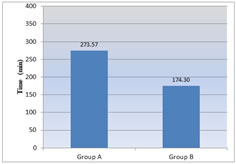
Graph 2: Duration of Postoperative Analgesia The duration of postoperative analgesia was longer in Group A (273.57 ± 13.25) than in Group B (174.30 ± 24.24), which was statistically significant (p < 0.05). Table 3: Total dose of Analgesia in 24 hours
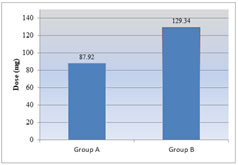
Graph 3: Total dose of Analgesia in 24 hours The total dose of consumption of rescue analgesia was lower in Group A (87.92 ± 5.59) than in Group B (129.34 ± 11.81), which was statistically significant (p <0.05).
DISCUSSION Abdominal hysterectomy is usually associated with considerable pain during the postoperative period, which may affect multiple systems and induce physiological, immunological, and psychological changes. Adequate postoperative analgesia causes reduction in the postoperative stress response and postoperative morbidity and in certain types of surgeries postoperative analgesia does yield an improved surgical outcome. Other benefits of effective regional analgesic techniques include reduced pain intensity, decrease in the incidence of side effects from analgesics and improved patient comfort. TAP block as a regional analgesic technique for postoperative analgesia is very useful in major abdominal surgeries. Adjuvants are used to intensify the quality and increase the duration of local anesthetics in different regional block techniques. In my study, postoperative analgesia with the addition of Dexamethasone (Group A) or Dexmedetomidine (Group B) to Bupivacaine in TAP block was compared. The average VAS score in patients who received TAP block with Dexamethasone(Group A) was significantly lower than those who received TAP block with Dexmedetomidine (Group B) (p < 0.05). Further, the duration of analgesia was longer in Group A compared to Group B, which was statistically significant (p < 0.05). The total dose of rescue analgesic requirement was lower in Group A compared to Group B, which was statistically significant (p < 0.05)0. There were no significant side effects in both the groups. Deshpande JP et al.1 studied the analgesic efficacy of Dexamethasone (4 mg) added to Ropivacaine in transversus abdominis plane block for transabdominal hysterectomy under subarachnoid block. Addition of dexamethasone to Ropivacaine in TAP block prolonged the postoperative analgesia and reduced postoperative analgesic requirement following abdominal hysterectomy under spinal anesthesia. A study conducted by Rai P et al.2 studied the effect of addition of Dexmedetomidine (0.5mcg/ kg) to Ropivacaine (0.25% 20ml) in transversus abdominis plane block on postoperative pain in lower segment caesarean section under spinal anaesthesia. The time for first analgesic dose was longer in Dexmetomidine group. VAS score was found to be lower in all postoperative patients for the first 6 hours in Dexmedetomidine group. Hence the authors concluded the addition of Dexmedetomidine to Ropivacaine in TAP block helps to achieve better analgesia and decreases the total dose of analgesics required postoperatively without any major side-effects. Another study conducted by Ramya Parameswari A et al.5 to compare the efficacy of 20ml of Bupivacaine (0.25%) with 0.5μg/kg of Dexmedetomidine and 20ml Bupivacaine (0.25%) alone for TAP block for Post-operative Analgesia in Patients Undergoing Elective Caesarean Section under spinal anaesthesia. The addition of Dexmedetomidine to Bupivacaine in TAP block prolonged the duration of postoperative analgesia.
CONCLUSION Addition of Dexamethasone to Bupivacaine in TAP block prolonged the duration of postoperative analgesia and reduced the analgesic requirements compared to addition of Dexmedetomidine following open abdominal hysterectomy under spinal anaesthesia without any major side effects.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home