|
Table of Content - Volume 21 Issue 3 - March 2022
Comparative study of ropivacaine and nalbuphine and ropivacaine alone in PNS guided supraclavicular brachial plexus block
Shraddha Kangad1*, Pratik M Doshi2, Khatija Dalvani3, Vandana Parmar4
1Assistant Professor, 2Associate Professor, 3Tutor, 4Professor & HOD, PDU Department of Anaesthesiology, Government Medical College and Hospital, Rajkot, Gujarat, INDIA. Email: shraddhakangad8@gmail.com, pratikdoshi880@yahoo.com, dalvanikhatija@gmail.com, vandanapithadia@gmail.com
Abstract Background: Adjuvants has been used with local anaesthetics to improve the quality and duration of analgesia. Nalbuphine being a mixed k agonist and µ antagonist opioid have been studied several times as adjuvant to local anesthetics in spinal, epidural, local infiltration and on brachial plexus block. The present study was aimed to evaluate the efficacy of nalbuphine with ropivacaine on nerve blockade during brachial plexus block using peripheral nerve stimulator. Material and Methods: One hundred and ten patients undergoing upper limb surgery were randomly divided into two groups, Group R and N. Group R received 30 ml of 0.5% of ropivacaine with 1 ml normal saline while Group N received same amount of ropivacaine with 1 ml (equivalent to 10 mg) of nalbuphine for supraclavicular brachial plexus block. The groups were observed for onset time and duration of both sensory and motor blockade, duration of post-operative analgesia and intra and post-operative complications Results: There was a significant decrease in onset time and increase in duration of motor and sensory block and analgesia in Group N as compared to Group R patients (P < 0.0001). No complications of technique and hemodynamic variations or any adverse effects due to nalbuphine had occurred. Conclusion: Use of 10 mg of nalbuphine as adjuvant to ropivacaine for brachial plexus block prolongs motor and sensory block and analgesia without significant side effects. Keywords: Brachial Plexus Block, Nalbuphine, Ropivacaine.
INTRODUCTION Regional anaesthesia benefits the patient with extended post-operative pain relief and the doctor with satisfactory surgical conditions with complete sensory and motor blockade. The supraclavicular approach for brachial plexus block has been long in practice for upper limb surgeries.1 Ropivacaine is an amide local anesthetic having differential blocking effect on motor and sensory nerve fibers. When compared to bupivacaine, it has reduced potential for cardiotoxicity and central nervous system toxicity, appears to be an important option for regional anesthesia and management of postoperative pain.2 Nalbuphine is mixed k agonist and µ antagonist has the potential to maintain or even enhance µ-opioid based analgesic effect while simultaneously mitigating the µ-opioid side effects. It was studied several times as an adjuvant to local anesthetics and the result of all studies concludes that Nalbuphine is effective when used as an adjuvant to local anesthetics in spinal, epidural, and local intravenous block, as it significantly prolongs the block duration.3Hence, we aimed to compare the efficacy of Nalbuphine 10 mg as an adjuvant to local anaesthetic agent 0.5% Ropivacaine 30 ml in PNS guided supraclavicular brachial plexus block for upper limb surgeries.
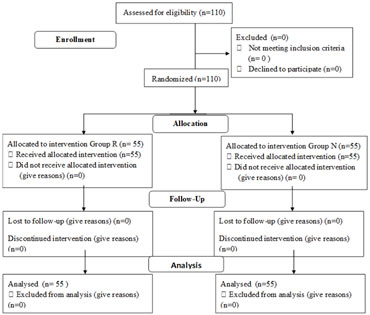
MATERIAL AND METHODS After approval from Institutional Ethics Committee-Human between October 2017 to October 2019, one hundred ten patients of ASA I and II of both genders, aged 18–60 years, scheduled for elective upper limb surgeries were enrolled for this prospective, randomized, double blind control study in PDU Government Medical College and Hospital, Rajkot. Written informed consent was taken from all the patients for anaesthesia as well as enrolment in the study. One hundred ten patients were divided into two groups of fifty-five patients each (consort flow diagram) [Figure 1]. Group R patients received Inj. Ropivacaine 0.5% (30 ml) with normal saline 1ml making total 31ml whereas Group N received Inj. Ropivacaine 0.5% (30 ml) with Nalbuphine 10 mg (1 ml) making total 31ml.Benefits and likely complications of the technique used were explained to the patients and their caretakers in understandable language. All patients underwent a thorough pre-anaesthetic check-up which included history taking, general examination, systemic examination and local neurological examination. Routine investigations were carried out for all patients. All patients were taught about pain scale regarding numerical rating scale during pre-operative visit. Patients with known case of allergy to local anaesthetics and opioids, local infection at site of block, brachial plexus injury, neuromuscular diseases, bleeding disorders or patient on anticoagulant therapy were excluded. The day before the surgery, procedure was explained and kept Nil by Mouth after 10 pm. On the day of surgery, IV line was secured and Inj. Dextrose Normal Saline (DNS) was started. Standard monitors like Electro Cardio Gram (ECG) leads, Non-Invasive Blood Pressure (NIBP) cuff, and pulse oximeter were applied and baseline parameters like Pulse Rate (PR), Systolic, Diastolic and Mean Blood Pressure (SBP, DBP, MBP respectively), SpO2, and pain score were recorded. Premedication given: Inj. Ondansetron (0.08 mg/kg) iv, Inj. Ranitidine (1 mg/kg) iv, Inj. Midazolam (0.04 mg/kg) iv. Identical looking syringes filled with local anaesthetic mixture were prepared by a resident doctor not directly or indirectly involved in the study. Patients were randomly allocated into two groups using a computer-generated random number and concealed by sealed opaque envelopes. The anaesthesiologist giving block and accessing parameters were blinded to the drugs given in supraclavicular block. Classical technique was used for performing brachial plexus blockade through supraclavicular approach. Local infiltration with plain 2% 2cc lignocaine was given to minimize needle pain. A 22G 5cm insulated needle with the nerve stimulator was directed just above and posterior to the subclavian arterial pulse and directed caudally at a very flat angle against the skin, until the flexion of finger was noted. After negative aspiration for blood, 31ml of respective drug will be injected depending on whether patient is allotted to either group R and N. Pulse rate, blood pressure, oxygen saturation was recorded before the procedure and there after every 5 min after the administration of block till half an hour, and then every 15 min till the end of procedure and postoperatively. Simultaneously patient was monitored intraoperatively and postoperatively for numerical rating scale (Pain) score and any complications like nausea, vomiting, chest pain, coughing, convulsion, hypotension and bradycardia. Sensory block was assessed every 3 min and motor block was assessed at every 5 min intervals for the initial 30 min and after 12-hour post block, and every 60 min until complete recovery. Onset of Sensory block was assessed by pin prick test in areas innervated by radial, ulnar and median nerves and compared with the same stimulation on contra lateral hand. Sensory block will be graded as Grade 0- Sharp pain Grade 1- Touch sensation only Grade 2- No sensation. Onset time will be defined as- dull sensation on any of the nerve distribution. Sensory peak effect time is defined as- complete loss of sensation along all the nerve distribution. Total duration of sensory blockade is defined as- Time interval between injection of drug and complete recovery of sensation. Similarly, onset of motor block was evaluated by asking the patient to move the forearm against resistance and to flex the forearm. Motor block assessed by the Bromage scale: Normal motor function. - Decreased motor strength with ability to move the finger only. - Complete motor block with inability to move the fingers. Onset time will be considered when patient felt heaviness on abduction of arm at shoulder. Motor peak effect time is absence of any voluntary movement at the level of arm and forearm. Total duration of motor blockade is defined as Time interval between injection of drug and complete recovery of motor power. Tourniquet inflation and deflation time and duration of surgery will be noted. Intensity of post-operative pain was evaluated using numerical rating scale with grade 0 (no pain) to 10 (worst pain). Pain score was noted every 5 to 10 minutes initially then hourly till the patient regain numerical rating scale score of 4. Analgesia was considered satisfactory if the score was 3 or less. If score was more than 4, analgesia was judged unsatisfactory and rescue analgesia was administered in the form of inj. Diclofenac sodium and time for need of first analgesia was noted. Both groups will be compared for total duration of analgesia (time interval between injections of drug in supraclavicular brachial plexus to rescue analgesic given), total duration of sensory blockade (Time interval between injection of drug and complete recovery of sensation) and total duration of motor blockade (Time interval between injection of drug and complete recovery of motor power).In our study primary outcome measures were duration of analgesia while secondary measures were onset and duration of sensory and motor blockade, pain scores, and evidence of any adverse drug reactions. The data was analysed by Graphpad Prism software. The data were expressed as mean ± standard deviation (SD). For demographic data, haemodynamic parameters, onset and duration of sensory and motor blockade and duration of analgesia unpaired t-test was applied. P-value was considered highly significant if <0.001.
OBSERVATIONS AND RESULTS The demographic profiles in both the groups were comparable [Table 1]. Onset time of sensory and motor block in Group N was significantly faster than Group R [Table 2]. The mean duration of sensory and motor block in Group N was significantly prolonged than Group R [Table 2]. No side effect was seen in either group. None of the patients in the two groups had incomplete or failed block. Rescue analgesia was given in the form of Inj. Diclofenac sodium 1.5mg/kg im when Numeric rating scale was ≥4. In Group N, 39(70.9%) patients required only 1 dose of rescue analgesia in first 24 hours, 16 (29.09%) patient required 2 doses of rescue analgesia. In Group R, 36(65.45%) patients required 2 doses of rescue analgesia in first 24 hours, 19 (34.54%) patient required 3 doses of rescue analgesia. In our study, patients of Group N required significantly less number of Diclofenac sodium Injection in first 24 h of the postoperative period than patients of Group R. In our study, we have also monitored the incidence for headache, nausea, vomiting, hypotension, bradycardia, chest pain, pruritis, convulsion and respiratory depression. Complication of supraclavicular block includes pneumothorax, phrenic nerve block (ipsilateral), horner’s syndrome, neuropathy and haematoma formation at site of injection. However, we have not come across any of these complications. The demographic profiles (age, gender) were comparable for both the groups. [Table 1]
Table 1
Onset time and duration of sensory and motor block and duration of analgesia in both groups. [Table 2] Table 2
Figure 1: Consort flow diagram explaining Randomised trail of two groups. DISCUSSION Nalbuphine used in addition to ropivacaine 0.5% for peripheral nerve stimulator (PNS) guided supraclavicular brachial plexus blockade decreases the onset time for sensory and motor blockade, increased the duration of both sensory and motor blockade, and the need for rescue analgesic in post-operative period was also reduced significantly. As duration of action of local anaesthetics is short, increasing the dose of local anaesthetics may prolong the duration of action but may also increase the risk of systemic toxicity.4 To improve the quality and increase the duration of anesthesia and post-operative analgesia, since many year, different types of adjuvants have been added to local anesthetics in peripheral nerve block. Nalbuphine being a mixed k-agonist-μ-antagonist opioid have affinity to k-opioid receptors results in analgesia, sedation, and cardiovascular stability with minimal respiratory depression and also have the same mode of action on opioid receptors, and inhibition of neuronal serotonin uptake which leads to augmentation of the spinal inhibitory pain pathways. Due to stimulation of opiate receptors on neurons of the central nervous system lead to hyperpolarization of the cell membrane potential and inhibition of action potential transmission of ascending pain pathways.3 The use of peripheral nerve stimulator has shown the considerable increase in the success rate of block and despite ultrasound-guided peripheral nerve blockade, nerve stimulation remains a popular technique used alone.5 It allows a precise localization of nerve plexus improving the accuracy and decreasing the chances of nerve injury.6Due to unavailability of USG in our institution, we have chosen to use peripheral nerve stimulator in our study. In our study, the onset time for sensory and motor block was earlier with Group Nalbuphine.4,8-12 The result in our study is in agreement with other studies, showed that addition of Nalbuphine with local anaesthetic in supraclavicular brachial plexus block prolongs sensory and motor block along with duration of analgesia.3,4-12The addition of ropivacaine with nalbuphine showed a significant difference in the pain scores. The number of patients who required rescue analgesia in the form of Diclofenac sodium in Ropivacaine with Nalbuphine group were 70.9%, 29.09% respectively, who needed 1,2 doses of rescue analgesics in 24 h, respectively, whereas in Ropivacaine alone group 65.45%, 34.54% needed 2, 3 doses respectively.Less requirement of number of diclofenac sodium injection as rescue analgesia in first 24 h of the postoperative period in Group N.9,10In our study use of nalbuphine were not associated with any hemodynamic variability or any adverse event in intra operative or post-operative period .3,7,8-12
CONCLUSION Addition of Nalbuphine as an adjuvant to local anaesthetic agent Ropivacaine(0.5%) for PNS guided supraclavicular brachial plexus block hastens the onset time and prolongs the duration of sensory-motor blocks and also significantly improves the quality and duration of postoperative analgesia and decreases requirement of rescue analgesics. Hence, Nalbuphine as an adjuvant prolongs the time to first analgesic request, provides significantly lower postoperative VAS pain scores.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home