|
Table of Content - Volume 21 Issue 3 - March 2022
Comparison of perineural and intravenous dexamethasone on duration of analgesia in supraclavicular brachial plexus block
J Keerthana1, M S Prasanth Kumar2*, S Shaik Mushahida3
1,2,3Department of Anaesthesiology, PSGIMSR, Peelamedu, Coimbatore -641004 Tamil Nadu, INDIA. Email: nimi_5@yahoo.co.in
Abstract Background: Pain in the postoperative period is a major concern for anaesthesiologists, which is usually managed by administration of opioids or analgesics. Single shot nerve blocks with additives such as alpha 2 agonists, opioids and glucocorticoids provide adequate analgesia for a longer duration postoperatively when compared to intravenous opioids or analgesics thereby reducing polypharmacy. The addition of glucocorticoids such as Dexamethasone perinerually increases the duration of analgesia but there are concerns regarding potential neural toxicity. Hence, we compared the analgesic duration, onset of sensory block and motor block in patients receiving Dexamethasone 8 milligram perineurally vs intravenously in supraclavicular brachial plexus block to avoid the potential neural toxicity due to perineural injection of the same. Methodology: 60 patients assessed under ASA 1 and 2 belonging to both genders aged between 20- 70years posted for upper limb surgeries under Supraclavicular brachial plexus block were randomly allocated into two groups: Group 1 – patients received 8mg Dexamethasone perinerually, Group 2 – patients received intravenous 8mg dexamethasone The onset of sensory blockade, onset of motor blockade, duration of analgesia, requirement of rescue analgesia postoperatively and severity of pain at the time of administration of analgesia was noted. Results: The onset of sensory blockade, motor blockade, duration of analgesia in both the groups were comparable with no statistical significance. Conclusion: Both IV and perineural Dexamethasone similarly prolonged the duration of analgesia in Supraclavicular Brachial Plexus block. Due to the existence of some controversies over perineural use of Dexamethasone, IV Dexamethasone can be used as a safer alternative to prolong duration of analgesia in patients undergoing upper limb surgeries under Supraclavicular Brachial plexus block. Key Word: perineural, intravenous, dexamethasone, analgesia, brachial plexus
INTRODUCTION Pain is the most common complaint of patients in the post-operative period and its management forms an important component of peri-operative care1.Supplementation of excessive opioids and other analgesics such as Non steroidal anti-inflammatory drugs (NSAID’S) for pain management often becomes necessary in most of the cases. Opioids have their own side effects such as nausea, vomiting, respiratory depression and dependence when used in large doses while NSAID’s are contraindicated in patients with renal and liver dysfunction2. Brachial plexus nerve blocks with additives for upper limb surgeries provide superior analgesia, avoid side effects of general anaesthesia and also minimise use of analgesics in the post-operative period3,4. Single shot Brachial Plexus blocks provide analgesia in the immediate post-operative period whereas continuous peripheral nerve blocks with the use of catheters provide extended analgesia as post-operative pain can exist for several days1.Catheter migration, leakage of the local anaesthetic, infection5,6,7, lack of expertise to perform continuous peripheral nerve blockade and lack of continuous monitoring are some of the major problems with continuous nerve block catheters. Hence, various additives have been studied in an attempt to enhance the effect of single shot nerve blockade. These additives prolong the duration of blockade either by producing local vasoconstriction or delaying diffusion of local anaesthetic from the site of injection. Commonly used additives include alpha 2 agonists, NSAID’s, opioids, and glucocorticoids8. Addition of Dexamethasone with local anaesthetics in peripheral nerve blocks to prolong duration of analgesia is being extensively studied. Although many studies have shown that the addition of Dexamethasone perineurally increases the duration of analgesia, there are concerns regarding potential neural toxicity but the evidences remain inconclusive 9,10. The use of intravenous Dexamethasone as a safe alternative to perineural Dexamethasone in prolonging the analgesia duration is being studied and investigated recently. In our study we have compared the analgesic duration between patients receiving Dexamethasone 8 milligram perineurally and by the intravenous (IV) route in supraclavicular brachial plexus block. We have also compared the difference, if any between the onset of sensory and motor blockade in both the groups.
AIM OF THE STUDY Primary Aim: The aim of the study is to compare the effects of perineural and IV Dexamethasone in the duration of analgesia in adult patients undergoing elective upper limb surgeries under Supraclavicular Brachial Plexus block. Secondary Aim: To find out the difference if any, between the onset of sensory and motor blockade in patients receiving perineural and IV Dexamethasone.
METHODOLOGY The study was done in PSG Institute of Medical sciences and Research, Coimbatore after obtaining clearance from the Institutional Human Ethics Committee and informed written consent from the patients. Sample size of 30 patients per group was calculated using duration of analgesia as the primary outcome based on previous studies. Inclusion Criteria: Patient acceptance. ASA 1 and 2 patients. Patients aged between 20-70 years. All patients posted for elective upper limb surgeries under Supraclavicular Brachial Plexus block. Exclusion Criteria: Patients with history of allergy to local anaesthetics. Patients on steroid therapy. Patient with Diabetes and Coagulopathies. Infection at the site of proposed puncture for block. Neuropathies. Routine pre-operative assessment of the patients was done prior to the surgery and tablet Ranitidine 150 mg was prescribed the night before surgery and on the day of surgery. Starvation guidelines were followed. The patients were randomly allocated into two groups (group 1 and group 2) using the random table method. After shifting the patient to the operating room, monitors were connected and baseline parameters recorded. The consultant in the operating room who was not involved in the study prepared the study drug according to the group in which the patient belonged to. All vital parameters were recorded every 5 minutes. Under aseptic precautions Supraclavicular Brachial plexus block was performed using a nerve stimulator. Group 1: Patients received 3mg/kg of Bupivacaine and 8 mg (2ml) of Dexamethasone perineurally and 2ml normal saline intravenously. Group 2: Patients received 3mg/kg of Bupivacaine and 2 ml of normal saline perineurally and 8mg (2ml) of Dexamethasone intravenously. The time of injection of the local anaesthetic, onset of complete sensory and motor blockade was noted and recorded. Patients were followed up post-operatively and the time of administration of first analgesic was recorded. The severity of pain at the time of administration of analgesic was graded with the verbal analogue scale. Definitions: Onset of sensory blockade was defined as the time interval between the end of local anaesthetic administration to loss of sensation to needle prick. In our study this was tested using needle prick method. Onset of motor blockade was defined as the time interval between the end of administration of the local anaesthetic to inability to move the fingers. In our study it was tested using the modified Bromage score. Duration of sensory blockade was defined as the time interval between the completion of injection of local anaesthetic to the administration of first analgesic to the patient. Modified Bromage Scale:
Verbal Analogue Scale:
Statistical Analysis: The data was entered in Microsoft excel 2010 and statistical analysis was performed using the software SPSS version 23.0. Data was expressed as percentages and mean values with standard deviations. Differences between both the groups were analysed using the independent sample ‘t’ test and the Pearson’s chi square test. Results were defined as statistically significant if the ‘p’ value was less than 0.05. RESULTS AND OBSERVATION Table 1: Demographic Distribution Of The Two Groups
Table 2:
Comparison Of Onset Of Sensory Blockade: For statistical purpose, the onset of sensory blockade was segmented into two categories according to the mean and median values. According to the statistical analysis mean sensory onset in both groups was 14.47 with a median value of 15. Hence the grouping was done as sensory onset less than 14 minutes and more than 15 minutes. In group 1, 33% of patients had a sensory onset below 14 minutes and 66% of patients had sensory onset more than 15 minutes. The mean sensory onset in group 1 was found to be 15.23 In group 2, 36.6 % of patients had sensory onset less than 14 minutes and 63.3%of patients had a sensory onset of more than 15 minutes. The mean sensory onset in group 2 was found to be 14.45. When the sensory onset in both the groups were compared, there was no significant statistical difference according to the ‘p’ value of 0.861. Figure 1: Comparision Of Sensory Onset In Both Groups
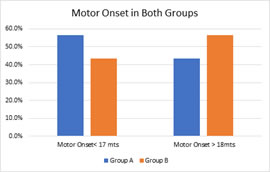
Comparision Of Onset Of Motor Blockade: For statistical purpose, the onset of motor blockade was segmented into two categories according to the mean and median values. According to the statistical analysis mean sensory onset in both groups was 17.14 with a median value of 17. Hence the grouping was done as motor onset less than 17 minutes and more than 18 minutes. In group 1, 58.62% of patients had a motor onset of less than 17 minutes and 43.33% had a motor onset of more than 18 minutes. In group 2, 48.3% of patients had a motor onset of less than 17 minutes and 56.6% of patients had a motor onset of more than 18 minutes. The mean motor onset was 17.21 in group 1 and 17.34 in group 2. According to the ‘p’ value of 0.240 there was no significant statistical difference in onset of motor blockade between both the groups.
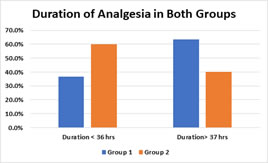
Figure2 : Comparision Of Motor Onset In Both Groups Comparision Of Duration Of Analgesia: Duration of analgesia was segmented into two, based on the mean and median values. According to statistical analysis the mean duration of analgesia was 35 hrs and the median was 36 hrs. In group 1, 36.6 % of patients had analgesia for less than 36hours and 63.3 % of patients had analgesia for more than 37 hours. The mean analgesic duration in group 1 being 38.89 hours. In group 2, 60% of patients had analgesia duration of less than 36 hours and 40% of patients had analgesia more than 37 hours. The mean analgesia duration in group 2 was 34.39 hours. When duration of analgesia was compared between the two groups, there was no significant statistical difference according to the ‘p’ value of 0.240. Figure 3: Comparision Of Duration Of Analgesia DISCUSSION Post- operative pain is the commonest complaint in patients undergoing upper limb surgeries. Administration of multiple analgesics in the post-operative period often may result in a number of adverse effects. Single shot brachial plexus nerve blocks often fail to provide extended analgesia in the post-operative period, hence the use of additives with local anaesthetics to prolong the duration of sensory blockade is practiced11. Many additives have been used with local anaesthetics to prolong analgesic duration and improve the quality of the regional block5,10. The addition of glucocorticoids with local anaesthetics in brachial plexus supraclavicular blocks significantly prolongs analgesia without much side effects12,13. The analgesic effect of Dexamethasone added to local anaesthetics in the perineural route has been studied. The mechanism of action of locally administered Dexamethasone is probably by increasing the activity of inhibitory potassium channels on nociceptive ‘C’ fibres. It also causes some amount of vasoconstrictor effect14,15. The route of administration of Dexamethasone for prolonged analgesia in Brachial plexus Supraclavicular block remains a controversy. It is shown that perineural Dexamethasone may cause potential neurotoxicity but is not proved and evidences are also inconclusive 10. The use of IV Dexamethasone for prolonged post-operative analgesia is being studied recently. Analgesic effect of systemically administered Dexamethasone could be due to decreased production of inflammatory mediators and increased production of anti-inflammatory mediators as a result of binding of cytoplasmic glucocorticoid receptors to glucocorticoid response elements in the DNA10,17. Very few studies have been done comparing the analgesic effect of Dexamethasone administered IV vs perineurally in Brachial Plexus block. In our study we have compared the duration of analgesia with 8 milligram of Dexamethasone administered IV and perineurally in 60 patients undergoing elective upper limb surgeries under supraclavicular Brachial plexus block. In our study the demographic variables like, age, gender and weight were comparable between both the groups and no significant difference occurred between them in both the groups. The onset of sensory blockade was comparable between both the groups. The mean sensory onset in group 1 was found to be 15.23 minutes and that in group 2 was 14.45 minutes. Our results matched with the results of the study done by Parveen et al2 in 2015 who also inferred that no significant statistical difference occurred between the onset of sensory blockade in the IV and the perineural group. The studies conducted by Desmet et al1 and Rosenfeld et al10 also did not show any significant difference in the onset of sensory blockade between the two groups. The onset of motor block was compared in both the groups. The mean motor onset in group 1 was found to be 17.21 minutes and the mean motor onset in group 2 was 17.34 minutes with no statistical significance similar to the findings of Abdallah et al16. Alarasan et al17 compared the effects of perineural Dexamethasone in supraclavicular block and showed that the Dexamethasone group had a shorter onset of motor blockade than the control group. The mean duration of analgesia in group 1 was found to be 38.89 hours and that in group 2 was found to be 34.39 hours. Though the mean analgesia duration in group 2 was lower than the mean analgesia duration in group 1 there was no significant statistical difference in the analgesia duration between the two groups. Our study results matched with the results of the study conducted by Abdallah et al16 who also inferred that both IV and perineural Dexamethasone had the same duration of analgesia when added in Supraclavicular brachial plexus block. Kawanishi et al18 compared the effects of Dexamethasone 4mg with interscalene brachial plexus block using Ropivacaine and concluded that only perineural Dexamethasone prolonged analgesia duration when compared to the control group.
SUMMARY A study titled “Comparison of IV and perineural Dexamethasone in prolonging duration of analgesia in Supraclavicular Brachial plexus block” was carried out in PSG Institute of Medical Sciences and Research. The study included 60 patients randomly divided into two groups of 30 patients in each group. One group received Dexamethasone 8 mg perineurally with supraclavicular block and the other group received Dexamethasone 8mg IV along with supraclavicular block. Parameters such as onset of sensory and motor blockade and duration of analgesia was noted. All data were entered in Microsoft excel 2010 and were analysed in SPSS software version 23.0. Demographic variables such as age, gender and weight were comparable between both the groups and no significant difference existed between both the groups. The onset of sensory and motor blockade was similar in both the groups and showed no significant statistical difference. Theprimary outcome of the study was duration of analgesia. The mean duration of analgesia was less in the IV group as compared with the perineural group but the results were not statistically significant. CONCLUSION Both IV and perineural Dexamethasone similarly prolonged the duration of analgesia in Supraclavicular Brachial Plexus block. The onset of sensory and motor blockade showed no difference between the two groups. The mean duration of analgesia in the perineural group was slightly higher as compared to the IV group but the results were not statistically significant. Due to the existence of some controversies over perineural use of Dexamethasone, IV Dexamethasone can be used as a safer alternative to prolong duration of analgesia in patients undergoing upper limb surgeries under Supraclavicular Brachial plexus block.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home