|
Table of Content - Volume 21 Issue 3 - March 2022
Swetha P1, Manjula R2, Prathibha P3*
1Assistant Professor, 2Professor, 3Junior Resident, Department of Anesthesiology, Adichunchanagiri Institute of Medical Sciences, B.G.Nagara, Mandya 571448, Karnataka, INDIA.
Abstract Background: Fascia Iliaca and Femoral nerve blocks are used frequently in patients posted for hip surgery, for analgesia and adequate positioning to aid central neuraxial blockade (CNB). They are known for their feasibility, opioid sparing effects and reduction in opioid related adverse effects. Recently in 2018, Pericapsular Nerve Group (PENG) block was described for analgesia in hip fracture patients as an alternative to Fascia Iliaca and Femoral Nerve blocks. Aims And Objectives: To evaluate the effectiveness of this technique in providing analgesia for effective positioning and aiding the CNB in patients posted for hip surgeries such as, hip replacement, Neck of femur fracture, Intertrochanteric and subtrochanteric fracture and to study block related complications. Materials And Methods: Total 25 patients of ASA I and II, between the age group of 18-80 years, posted for hip surgery under CNB, were selected for this study. PENG block was administered in these patients in the procedure room before shifting on operation table, using ultrasound and inguinal ligament as landmark. 20ml of 0.5% Ropivacaine was the local anesthetic used for the study. The comfort during positioning for Spinal/ Combined spinal epidural anaesthesia was assessed by Ease of Spinal Position score (EOSP). Results: All 25 patients had successful block and could sit comfortably during CNB. Median EOSP score was 3 (2-3). No complications were observed. Conclusion: PENG block is a good alternative to Fascia Iliaca and Femoral Nerve block in patients posted for hip surgery. Inguinal ligament based, ultrasound guided PENG block provides good analgesia without complications.
INTRODUCTION Peripheral nerve blocks (PNBs) are commonly given as a component of multimodal analgesia and may be administered as a single injection or continuous infusions. They demonstrate superior pain control and reduce the opioid consumption.1,2 Fascia iliaca (FI) and femoral nerve (FN) blocks are commonly practiced to provide analgesia and aid positioning for central neuraxial blocks (CNB) in patients posted for hip surgery.2 In 2018, Giron-Arango L et al., described a new block, called the PENG block, for analgesia in patients with hip fracture.3 PENG block is primarily an ultrasound guided technique, where articular branches of femoral nerve and accessory obturator nerve (AON) are blocked.3 The block area is the pelvic rim (superior pubic ramus) near iliopectineal eminence (IPE), deep to fascia of ilio-psoas muscle.3,5 However, by increasing the local anaesthetic (LA) volume, obturator, femoral, genitofemoral and lateral femoral cutaneous nerves can also be blocked.6 Hence the indications for this block are increasing, and this block has been used for surgical anaesthesia in reduction of dislocated hip and varicose vein stripping procedures.7,8 To assess the effectiveness of inguinal ligament based approach to PENG block in providing analgesia, to aid positioning for CNBs in patients posted for hip surgery [hip replacement, neck of femur (NOF) fracture, intertrochanteric (IT) and subtrochanteric (ST) fracture], we conducted a feasibility study. AIMS AND OBJECTIVES Primary Aim: To assess the analgesic effectiveness of the ultrasound guided PENG block with inguinal ligament as landmark. Secondary Aim: To assess the procedural difficulty and block related complications.
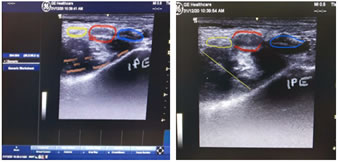
MATERIALS AND METHODS After obtaining ethical committee clearance and written informed consent, 25 ASA 1 and 2 patients between the age group of 18 – 80yrs, posted for hip surgery (hip replacement, NOF fracture, IT and ST fracture) under CNB were selected. Standard NPO protocols and adequate antibiotic prophylaxis were followed. In procedure room, after connecting NIBP, SPO2 AND ECG monitors, pain intensity was assessed in supine position. After taking adequate aseptic precautions, a low frequency curvilinear ultrasound probe was placed in plane with inguinal ligament. After appreciating the femoral artery and nerve, the probe was moved cephalad in parallel to inguinal ligament, tracing the femoral artery and nerve until the pubic ramus and IPE were appreciated. With in plane approach, 20 gauge and 100mm needle was inserted from lateral to medial and needle tip was placed in the plane between the pubic ramus posteriorly and ilio-psoas muscle anteriorly avoiding injury to the femoral nerve. After negative aspiration, 20 ml of 0.5% Ropivacaine was infiltrated in this plane. Adequate LA spread i.e., lifting of the ilio-psoas muscle from the pubic ramus was appreciated. After the block, patients were shifted on to operating table and standard monitors (NIBP, SPO2 AND ECG) were attached. Adequate IV fluids were connected and later positioning for CNB was done. EOSP scoring was performed to assess the comfort during the positioning. The time elapsed between the block and EOSP scoring was roughly between 8 – 10 minutes. Figure 1 Figure 2
RESULTS Successful needle placement and adequate spread of LA was appreciated in all patients. All patients were comfortable during positioning for CNB, as assessed with EOSP score (table 1). No block related complications were noticed in these patients.
Table 1: demographic profile, EOSP score and complications.
DISCUSSION Regional nerve blocks are often used for providing analgesia in patients with hip fractures. FI and FN blocks are used frequently in patients posted for hip surgery, for analgesia to aid positioning for CNB.2 A recent Cochrane review on peripheral nerve blocks in hip fractures has shown reduction in dynamic pain within 30 minutes of blockade, reduced risk for pneumonia, decreased time to first mobilization and cost reduction of the analgesic regimen (single shot blocks).4 In 2018, PENG block was described for analgesia in hip fracture patients as an alternative to FI and FN blocks by Giron-Arango L et al.3 With PENG block, obturator nerve (ON) and AON blocks are well achieved when compared to FI and FN blocks. In FI and FN blocks, medial spread of LA to block ON doesn’t occur9, and more importantly cephalad spread is unlikely to spread beyond the L5 level.1 Recent studies have shown that PENG block produces more effective analgesia for positioning and post operative pain than FI block9 In contrast, the main targets of PENG block are articular branches of AON and FN between anterior inferior iliac spine (AIIS) and IPE. The sub pectineal plane (SPP) between the pectineus and obturator externus muscle has been recently described by Nielsen et al.11 as a target point for ON and its articular branches. Given the proximity of the SPP, it is believed that the LA may spread to this plane. However further studies are required to confirm this. Though PENG block was described to be pericapsular nerve block, it is questionable whether it blocks only ON, AON and articular branches of FN supplying hip joint or not.6,12,13 In our study, we used inguinal crease at the inguinal ligament as the landmark for the positioning of the ultrasound probe to visualize the IPE, pubic ramus, AIIS and psoas muscle to guide the PENG block. This study shows effective block of ON and FN to reduce the dynamic pain and provide a good position for CNB. It can be further studied to identify newer indications for PENG block.7,8,14,13
CONCLUSION With our results, we conclude that inguinal ligament can be used for correct positioning of ultrasound probe for PENG block, without any complications. This new approach provides effective analgesia for CNB positioning in patients posted for hip surgery.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home