|
Table of Content - Volume 21 Issue 3 - March 2022
Original Research Article
Hiren R Chauhan1*, Pratik Doshi2, Deesha Patel3, Vandana Parmar4, Jinal Gohil5
1Class I officer, 2Associate Professor, 3Tutor, 4Professor & HOD, 5IIIrd Year Resident, Department of Anaesthesiology, P.D.U. Government Medical College and Hospital, Rajkot-360001, INDIA. Email: drhiren44@gmail.com
Abstract Objective: To compare effect of 3 doses of chloroprocaine 1% 20,30 and 40mg for spinal anesthesia in high risk patients undergoing short duration surgery of lower limb with regards to hemodynamic parameters and Characteristics of sensory and motor block Material and Methods: 90 ASA physical status III and IV patients both male and female posted for various short duration lower limb surgeries under spinal anaesthesia were randomized into three group to receive one of the single doses of chloroprocaine 1% either 20mg,30mg or 40mg via intrathecal injection Results: The onset time of sensory and motor block, duration of sensory and motor block, maximum height of block, hemodynamic parameters was noted. Their hemodynamic parameters were stable and dermatomal level reached was T8-T10 in majority in the dose of 3ml and 4ml of chloroprocaine while in 2ml level is T12-L1. Serious side effect or neurological deficit associated with the drug did not occur in any patient in this study. Conclusion: 1% choloprocaine in the dose of 3ml and 4 ml to be effective and 20 mg dose may not be suitable for lower limb procedure for lasting 60 min. Keywords: chloroprocaine, spinal anesthesia, high risk patients, hemodynamic stability, short duration surgery,
INTRODUCTION Spinal anesthesia is a safe and reliable technique for surgery of the lower abdomen and lower limbs.1 2-Chloroprocaine is an amino-ester local anesthetic with a very short half-life. Spinal anesthesia performed with preservative-free 2-Chloroprocaine produces blocks with rapid onset, increased potency in comparison with Procaine, and no evidence of toxicity. In comparison with Bupivacaine, Lidocaine and Procaine 2-Chloroprocaine showed quicker onset of action, higher level of sensory blockade and early voiding and ambulation. Chloroprocaine constricts blood vessels resulting in reduced blood loss; this is in contrast to other local anesthetics e.g. lidocaine, which do not do such. Chloroprocaine was developed to meet the need for a short acting spinal anaesthetic that is reliable and has a favourable safety profile to support the growing need for day care surgery. When compared with lidocaine, the time to ambulation and time to discharge were significantly shorter with 2-Chloroprocaine.2 Chloroprocaine significantly less toxic than other compounds. Chloroprocaine used for spinal anaesthesia now a days is without preservative. Large number of research papers published particularly from 2004 onwards have shown the safety and efficacy of 2-Chloroprocaine preservative free preparation for use in spinal anaesthesia. None of the studies available to us till now showed any incidence of TNS or any other neurological deficit following use of 2-CP in spinal anaesthesia. This makes Chloroprocaine different from Lidocaine.3 When compared with lidocaine, the time to ambulation and time to discharge were significantly shorter with 2-Chloroprocaine.4 The duration of anaesthesia with different doses of Chloroprocaine used in spinal anaesthesia has been reported to be quite variable. Hence, we decided to carry out this study using three different doses of preservative free Chloropropane 1% i.e, 20mg,30mg and 40 mg in spinal anaesthesia for short duration surgeries. Aims and objectives of study: Primary: Effect on hemodynamic parameters. Requirement of total dose of vasopressors. Time to recovery of sensory block and motor block. Secondary: Assessment of sensory and motor block (onset time and readiness for surgery), Time of analgesia. Adverse events.
MATERIAL AND METHOD We obtained approval from our institution’s ethics committee and written informed consent was obtained from patients. It was a prospective randomized single blind clinical study. Inclusion criteria: Patients aged between 18- 65 years. Physical status ASA grade III and IV. Scheduled for lower limb surgeries. Exclusion criteria: Pediatric patients up to 18 years. ASA grade I, II and V. Known allergy to chloroprocaine and local anaesthetic agents. Local infection at the back region. Coagulation abnormality. Peripheral neuropathy. H/o CV stroke (Paraplegia and paraparesis). Spine surgery. Thyroid disease. Pregnant and lactating mother. Each group will be randomly allocated to three groups of 30 patients each. Group A: Receives 2 ml(20mg) chloroprocaine(1%) Group B: Receives 3 ml (30mg) chloroprocaine(1%) Group C: Receives 4 ml(40mg) chloroprocaine(1%) Statistical analysis of data: The parameters recorded were entered on a computer and compared between the three groups using ANOVA test and P≤0.05 is deemed significant. And statistical software from below mentioned site was used https://statpages.info/anova1sm.html Microsoft excel The significance was judged as follows- P > 0.05 not significant; P < 0.05 significant; P < 0.001 highly significant.
OBSERVATION AND RESULT Following the data collection, statistical analysis was done as described above. The results were as follows; The study participants of two study groups were comparable in terms of age, height and weight, gender and ASA classication in three groups. Table 1: Assessment of sensory block
Sensory block: Onset of sensory block: In our study we found the mean time for onset of sensory block 2.40±0.03 minutes in Group A, 2.30±0.032 minutes in Group B and 2.16±0.31 minutes in Group C. The difference was statistically highly significant (p<0.001). Time to achieve maximum sensory level: Time to achieve maximum sensory level was 4.12±0.04 minutes in Group A 4.00±0.04 minutes in Group B and 4.00±0.003 minutes in Group C which was statistically highly significant (p<0.001). Time for sensory regression: In our study the mean time taken for sensory regression was 51.83±11.02 minutes in Group A, 88.5±10.84 minutes in Group B, 137.5±18.50 minutes in Group C. The difference was highly significant statistically (p<0.001). Table 2: Assessment of motor block
Motor block: Onset time of motor block: Group A was 3.42±0.03 minutes, 3.36±0.036 minutes in Group B and was 3.16±0.022 minutes in Group C. The difference was statistically highly significant (p<0.001). Time to attain Maximum Motor level: Time to attain maximum motor level was 5.22±0.04 minutes in Group A while it was 5.12±0.042 minutes in Group B and 4.57±0.031 minutes in Group C. The difference was statistically highly significant (p<0.001). Duration of motor block: The mean duration of motor block was 40.5±9.86 minutes in Group A, 77.67±10.96 minutes in Group B and 113.67±16.29 minutes in Group C. The difference was statistically highly significant (p<0.001).
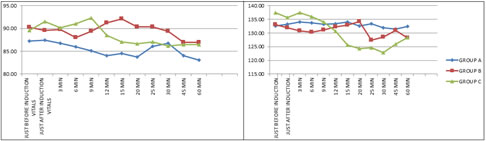
Figure 1 Figure 2 Figure 3 Figure 4 Figure 1: Intraoperative pulse rate: Mean pulse rate in three groups at different time intervals, there is no significant difference in mean pulse rate between three groups; Figure 2:Intraoperative systolic blood pressure after giving spinal anaesthesia. p value >0.05 which was not significant; Figure 3: Intraoperative diastolic blood pressure after giving spinal anaesthesia. It shows P value >0.05 at different time interval intraoperatively which was not significant; Figure 4: Intraoperative mean arterial pressure: Mean blood pressure in three groups at different time intervals, there is no significant difference in mean pulse rate between three groups.
Table 3: Duration of effective analgesia(minutes)
Table 3 shows the duration of effective analgesia in three Groups which was 60.5±9.94 minutes for Group A, 135.67±23.52 minutes for Group B and 155.67±17.30minutes for Group C. The difference was highly significant statistically (p<0.001) which indicate longer post-operative effective analgesia in Group C as compared to Group A and Group
Table 4: Intra and post operative complications
In Group C, bradycardia was observed in 2 (6.6%) patients which treated with Inj. Atropine 0.6 mg IV. In our study inclusion criteria of ASA grade III and IV which include septicemia, Ischemic heart disease, Myocardial infarction and other comorbid diseases. Chloroprocaine has very less effect on heamodynamics. So, only 5(16.66%) cases in Group C have response of spinal anesthesia as hypotension. And it was vigorously treated with IV fluids, oxygen and Inj. Ephedrine 0.1–0.5 mg/kg IV with very good recovery. Among them 1 patient required Inj. Noradrenaline infusion through microinfusion pump for 2-hour duration and it may be due to ASA grade IV patient having septicemia and IHD. 1 patient in Group A, 1 patient in Group B and 2 patient in Group C developed shivering and rigors which is treated with Inj. Tramadol 0.5 mg/kg i.v. No other complications like nausea and vomiting, urinary retention or respiratory depression transient neurological deficits were noted in three the groups. Post-operative period was uneventful in all cases. DISCUSSION In our study we found the mean time for onset of sensory block 2.40±0.03 minutes in Group A, 2.30±0.032 minutes in Group B and 2.16±0.31 minutes in Group C. The difference was statistically highly significant (p<0.001). Thus, it appears that the onset is dose related and comes fast by increasing the dose. Casati A et al.5 2006 observed that the median time required to achieve readiness to surgery was 8(3-25) min with 30 mg, 7 (3-26) min with 40 mg and 6(3-20) min with 50 mg dose of 2 CP (p =0.74). In our study we noticed that in Group A, peak sensory level achieved was T10 in 1(3.33%) patient, T12 in 15(50%) patients and L1 in 14 (46.62%) patients. IN Group B, T8 5 (16.65%) patients, T10 level in 18 (59.94%) and T12 level in 7(23.31%) patients. IN Group C, T6 level in 5(16.65%) patients, T8 level in 15(50%) patients and T10 level in 10(33.33%) patients. Smith K N et al.6 2004 observed that peak sensory level achieved was higher in higher drug dose. It was maximum atT2level (T6-C5) with 60mg, T5 (T10-T1) with 45 mg and minimum with 30mg at T7(L3-T2) level, p value 0.03. Kopacz DJ et al.7 2005 observed peak sensory level of L1 (T8-L4) with10 mg dose andT9 (T4-L1) with 20 mg dose. Thus 20 mg dose able to produce cephalad level of sensory anaesthesia of atleast L1 in all patients. Time to achieve maximum sensory level was 4.12±0.04 minutes in Group A 4.00±0.04 minutes in Group B and 4.00±0.003 minutes in Group C which was statistically highly significant (p<0.001). Camponovo C et al.8 2014 on the other hand found faster onset of peak sensory level with 50mg of 1% plain CP compared to 0.5% plain bupivacaine (8.5 vs14 min). Yoos J R et al.9 2005 did not find any difference in time to achieve peak sensory level (p 0.45) when 2CP was compared with 0.5% bupivacaine. In our study the mean time taken for sensory regression was 51.83±11.02 minutes in Group A, 88.5±10.84 minutes in Group B, 137.5±18.50 minutes in Group C. The difference was highly significant statistically (p<0.001). Sell A et al.10 2008 had the same observation as shown in all above studies. Time to complete sensory block regression was faster in the 35 mg group (111 min) and in the 40 mg group (108 min) than in the 50 mg group (134 min, P=0.005). In our study the mean onset of motor block in Group A was 3.42±0.03 minutes, 3.36±0.036 minutes in Group B and was 3.16±0.022 minutes in Group C. The difference was statistically highly significant (p<0.001).Camponovo C et al.8 2014 who compared 50 mg 2CP with 10 mg Bupivacaine intrathecally, found early onset of motor block (5 vs 6 min.) in 2CP group. In Group A, 10 (33.33%) patients had Modified Bromage score II and 20(66.66%) patients had Modified Bromage score III. In Group B, 11 (36.63%) patients had Modified Bromage score I, 16 (53.28%) patients had Modified Bromage score II and 3(9.99%) patients had Modified Bromage score III. In Group C, 19(63.27%) patients had Modified Bromage score I, 11 (36.63%) patients had Modified Bromage score II. Time to attain maximum motor level was 5.22±0.04 minutes in Group A while it was 5.12±0.042 minutes in Group B and 4.57±0.031 minutes in Group C. The difference was statistically highly significant (p<0.001). Sell et al.10 2008, observed that time for maximum motor block achieved was early in Group with higher dose than lower. The mean duration of motor block was 40.5±9.86 minutes in Group A, 77.67±10.96 minutes in Group B and 113.67±16.29 minutes in Group C. The difference was statistically highly significant (p<0.001). Smith K N et al.11 2004 Duration of motor block in the study as judged by Bromage scale was dose dependent 72±12 minutes with 30 mg, 88±15 minutes with 45 mg and 100± 13 minutes with 60 mg of 2CP, p being <0.001. Duration of motor block as judged by EMG at abdomen (Time to 90%) was also dose dependent, longer with high dose, p being < 0.01. Kouri M E et al.12 2004 Duration of motor block as per Bromage grading was 79±15 in 2CP 40 mg compared to 90±14 in 2% 40 mg Lidocaine group, p being 0.16. Caponovo C et al.8 2014 Resolution of motor block was much less in 2CP 50 mg compared to Bupivacaine 10 mg (100 vs 210 minutes). The mean duration of surgery was 62±5.19 minutes in Group A, 63±9.09 minutes in Group B and 65±9.09 minutes in Group C. P value >0.05 which was not significant There was need for supplementation of GA in 15 patients in Group A and 1 patient of Group B which conducted by Inj. ketamine (30mg to 50 mg) IV and Inj.propofol (50mg to 90 mg) IV due to inadequate dose effect and insufficient duration of sensory and motor block. Casati et al.5 2006 the mean duration of surgery was 45±15 with 30 mg, 50±13 in 40 mg and 48±15 min in 50 mg group of 2CP (p=0.68). the duration of surgery was between 30-60 minutes. They reported the use of intraoperative supplementation of analgesic in 7 (50%) patients with 30 mg, in 5 (33%) patients with 40 mg and in 2(13%) patients with 50 mg dose of 2CP. In 7 of these 14 patients (5 of 30 mg group and 2 of 40 mg group) analgesic supplementation was required on completion of procedure because of insufficient duration of block (at 40 minutes) for designed surgical procedure. Accordingly, the very small dose of 30 mg may be adequate for surgeries lasting <30 minutes. 40 and 50mg of plain Chloroprocaine provided adequate spinal anaesthesia for lower limb outpatient procedures lasting 45 to 60 min.
CONCLUSION After going through the study results and comparing the intrathecal effect of 20mg, 30mg and 40mg of preservative free 1% Chloroprocaine in spinal anesthesia, following conclusions can be drawn – Intrathecal 1% is a safe short acting local anesthetic for short or ultra-short surgical procedures. Onset and duration of sensory and motor block and time of recovery of ambulation were dose related. There is no signicant difference of systolic blood pressure, diastolic blood pressure and heart rate between these groups. The intraoperative haemodynamic parameter remained stable in all the three groups. 30 and 40 mg of plain chloroprocaine 1% provided adequate spinal anesthesia for lower limb outpatient procedures lasting 45 to 60 min. Reducing the dose of 2-chloroprocaine to 20 mg resulted in a spinal block of insufficient duration and had no advantages in terms of home discharge.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home