|
Table of Content - Volume 22 Issue 1 - April 2022
A comparative study of supreme laryngeal mask airway versus laryngeal tube undergoing general anesthesia in short surgical procedures
P S Kamat1*, K R Kulkarni2, I J Namazi3
1,2,3Department of Anaesthesiology, D. Y. Patil Medical College, Kolhapur, Maharashtra, INDIA. Email: kamatpooja102@gmail.com
Abstract Background: Aim is to compare the ease of insertion and associated pressor response of Supreme LMA and Laryngeal tube in patients undergoing general anesthesia in short surgical procedures. This prospective randomized study was conducted among ASA grade I and II patients aged between 18-60 years of either sex, 30 in each. In group L, Laryngeal tube and in group S, Supreme LMA was inserted. The ease of insertion and associated haemodynamic response among patients of two groups were noted. Statistically, the ease of insertion was better in SLMA than LT. The associated pressor responses of heart rate, systolic and diastolic blood pressure were lesser with SLMA than with LT. Supreme LMA was a better alternative device when compared to Laryngeal tube in maintaining an intact airway. However, both can be safely used in general anesthesia for elective surgical procedures. Keywords: Laryngeal tube (LT), Supreme LMA (SLMA).
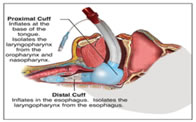
INTRODUCTION Laryngoscopy and endotracheal intubation is the commonest method of securing a definitive airway for administering anesthesia. However it is associated with tachycardia and hypertension and an increase in intraocular pressure.1 Most supraglottic airway devices are designed for use during routine anesthesia, for securing the airway and providing adequate ventilation.2 The LMA Supreme is the leading single-use, gastric access device which forms an effective first seal with the oropharynx and an innovative verifiable second seal with the upper esophageal sphincter.3The Laryngeal tube is an alternative to other airway management techniques. This device can be inserted through the oropharynx into hypopharynx to create an airway during anesthesia and cardiopulmonary resuscitation lungs.4 Hence, this study was carried out in an attempt to compare both these airway devices viz. Supreme LMA and Laryngeal tube with respect to the insertion conditions and pressor responses in patients undergoing general anesthesia in short surgical procedures.
METHODOLOGY After Ethical committee’s approval and written informed consent, we studied 60 patients (ASA I or II, aged 18-60 year, height 148±180 cm, weight 45±80 kg) undergoing general anesthesia in short elective surgical procedures. Patients with anticipated difficult airway, obesity (body mass index > 35 kg/m2), oropharyngeal pathology, cardiopulmonary disease, cervical spine fracture or instability, or at increased risk of aspiration were excluded from the study. In the anaesthetic room, Patients were premedicated with Tab. alprazolam 0.25 mg on the night before surgery. On the day of surgery, IV line was secured, followed by Inj. ranitidine 0.25 mg/kg IV and Inj. metoclopramide 0.15 mg/kg IV and Inj. ondensetron 0.1 mg/kg IV were administered 30 minutes before surgery. In the operation theatre, standard monitors were attached and baseline parameters were recorded. Inj. midazolam 0.05 mg/kg IV, Inj. glycopyrrolate 0.004 mg/kg IV, and Inj. fentanyl 1mcg/kg IV were administered 1-2 minutes before induction. After preoxygenation with 100 % O2 for 3-5 minutes, general anesthesia was induced with Inj. propofol 2-2.5 mg/kg IV. Lubricated SLMA /LT was inserted and secured. Figure 1: Insertion of LMA Supreme. SLMA was inserted according to the manufacturer’s instructions including weight-based recommendations for the size (SLMA: size 3 for patients 30 to 50 kg, size 4 for patients 50 to 70 kg, size 5 for >70 kg). After insertion, the SLMA device was then inflated to a pressure of 60 cm of H2O using a handheld pressure gauge device. Figure 2: Insertion of Laryngeal tube. Laryngeal tube was inserted according to manufacturer’s instructions including hight-based recommendations for the size. A size 3 was used for patients less than 155 cm, a size 4 for those between 155-180 cm, and a size 5 for those > 180 cm in height. After insertion, the cuffs were inflated using cuff inflator until the intracuff pressure reached to 80-90 cm of H2O.Insertions of all the devices were done by the same anesthesiologist. SPO2 was maintained >95 % by adjusting respiratory rate, FiO2 and tidal volume (7 ml/kg). If SLMA/LT insertion was unsuccessful after two attempts, the patient was withdrawn from the study. Correct placement of the devices was confirmed. Anesthesia was continued with 50 % N2O + 50 % O2 with sevofluorane. At the end of the surgery, anesthetic agents were discontinued and cuff was partially deflated for removal of SLMA and Laryngeal tube was removed after deflating both the cuffs after the patient regained consciousness spontaneously and responded to verbal command to open the mouth. The outcomes measured were as follows: Ease of insertion (Graded subjectively on a scale from 1 to 45 Grade 1: Excellent -No resistance to insertion, Grade 2: Good -Slight resistance to insertion, Grade 3: Poor -Moderate resistance to insertion, Grade 4: Impossible) and associated pressor responses of heart rate, systolic BP and diastolic BP just before insertion of SLMA / Laryngeal tube and Heart rate, systolic BP and diastolic BP at 1, 2, 3 and 5 minutes of SLMA / Laryngeal tube. Data was collected, tabulated, coded and analyzed using MS Excel 2007 and Statcal software. Numerical variables were presented as mean and standard deviation (SD) while categorical variables in percentage. For comparison between-groups, Unpaired t test and Chi-square test were applied. P value<0.05 was considered significant while <0.001 was considered highly significant.
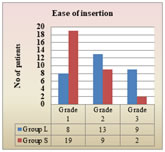
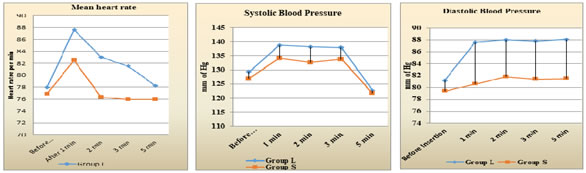
RESULTS The surgical procedures, patient characteristics and demographic data were comparable in both groups. In our comparative study we found the insertion was done easily in 19 (63.33 %) of the 30 patients in Group S patients. The difference between Group L and Group S was statistically significant p=0.007 (< 0.05). Graph 1: Grades of insertion conditions among two groups. Pressor response of Supreme LMA and Laryngeal tube showed the mean heart rate of Group S was significantly lesser at 1, 2, 3 and 5 minutes compared to Group L, which was statistically significant (p<0.05) also the mean systolic blood pressure of Group S was significantly lesser at 1, 2 ,3 and 5 minutes than that of Group L, which was statistically significant (p<0.05) and the mean diastolic blood pressure of Group S was significantly lesser at 1, 2, 3 and 5 minutes than that of Group L which was statistically significant (p<0.05).
Graph 2 Graph 3 Graph 4 Graph 2: Mean heart rate at different time among two groups; Graph 3: Mean systolic blood pressure at different time among two groups; Graph 4: Distribution according to the mean diastolic blood pressure at different time among two groups.
DISCUSSION The study was conducted for comparing the ease of insertion and pressor response of Supreme LMA and Laryngeal tube in patients undergoing general anesthesia in short surgical procedures. The insertion was easier in 19 (63.33 %) among 30 patients of Group S. The difference between Group L and Group S was statistically significant p=0.007 (<0.05). In the study done by Russo SG et al.,6 it was found that the insertion was easier with SLMA device than that of LT. The mean heart rate of Group S was significantly lesser at 1, 2, 3 and 5 minutes compared to Group L (P<0.05). Similar findings were seen in the study done by Wilson et al.7 where there was 0-20% rise in heart rate among children as well adults. The mean systolic blood pressure of Group S was statistical significantly lesser at 1, 2, 3 and 5 minutes than that of Group L (p<0.05). Similarly, the mean diastolic blood pressure of Group S was significantly lesser at 1, 2, 3 and 5 minutes than that of Group L (p<0.05). Similar findings were seen in study conducted by Dahaba AA et al.8 the LTS produced a greater and more sustained haemodynamic and catecholamine stress response than the PLMA. Systolic and diastolic blood pressure levels over time were significantly lower in the PLMA group than in the LTS group.
CONCLUSION Thus in conclusion, we could say that Supreme LMA was a better alternative device when compared to Laryngeal tube in maintaining an intact airway. However, both can be safely used to conduct general anesthesia for elective surgical procedures.
ACKNOWLEDGEMENT We thank all our colleagues in the department for assisting us in conducting this study.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home