|
Table of Content - Volume 22 Issue 2 - May 2022
Comparison of epidural catheter fixation via subcutaneous tunneling versus device fixation
Neha Sharma1*, Vidushi Sharma2, Ankur Kumar3
1Lecturer, Department of Anaesthesia Superspecility Hospital Government Medical College, Jammu, INDIA. {2Assistant Professor Department of Anaesthesia} {3Statistician Cum Lecturer Department of PSM} Kanti Devi Medical College Hospital and Research Centre Mathura, Uttar Pradesh, INDIA. Email: drneha116@gmail.com
Abstract Background: The efficiency of epidural analgesia greatly depends on the technique of securing the epidural catheter. Specific device for fixation of epidural catheter for example lock it epidural catheter clamp is available for securing the epidural catheter in place and it successfully prevents catheter migration. Tunneling of catheters has been associated with the possibility of catheter snapping and surgical retrieval has to be done for the same. Comparison between these two techniques for securing safe and efficient fixation of epidural catheters in the post-operative period has not been done. Materials and methods: A total of 100 patients requiring post-operative epidural analgesia for lower limb orthopedic surgery were randomized into 2 groups for the study. In Group I (n=50) epidural catheters were tunneled vertically in the paravertebral subcutaneous tissue and in Group II (n=50) a Lock-it device was used for catheter fixation. During the procedure, quantification of patient’s comfort was done using Likert score. We compared the two techniques on the basis of catheter migration, local trauma, snapping of catheter, dislodgement of catheter and catheter obstruction. Results: In group I, 12% of tunneled catheters had migrated outward significantly. Erythema was found in 22% of patients, 18% patients reported inadequate analgesia and 12% had bleeding from the site of tunneling and 70% of patients experienced significant procedural discomfort whereas in group II, 5% catheters were found kinked and 14% of patients had erythema from device adhesive (p=0.08), 14% reported inadequate analgesia (p=0.10) and catheter obstruction was found in 4% (p=0.10) of patients. Conclusion: On the basis of our study we conclude that fixation of epidural catheter using Lock-it device is safe, comfortable and efficient as compared to subcutaneous tunneling of the catheters. Keywords: epidural analgesia, tunneling, catheter, subcutaneous tissue, lock-it device.
INTRODUCTION Appropriate epidural catheter fixation forms the mainstay in providing post-operative analgesia in orthopedic patients requiring combined spinal epidural anesthesia. An inward migration of epidural catheter has been associated with subdural, sub arachnoid or intravascular injection of repeat doses while outward migration results in loss of analgesia. Migration has been correlated with numerous factors but the most practical approach to prevent the same remains proper fixation of the epidural catheter.1 The techniques that have been evaluated for their efficacy and safety for fixation of epidural catheter are fixation of adhesive foam with help of a suture.2 tegaderm dressing alone or along with shoulder fixation of the filter,3 Niko Epifix device3, Lock-it device4 and subcutaneous tunneling of the epidural catheter.5 Subcutaneous tunneling of the epidural catheter provides good fixation along with transparent dressing. Drag on the catheter can be decreased by interposed loop thereby protecting the catheter entering the epidural space. Catheter entry points are secured by sterile adhesive dressing which also prevents the chances of infection. We compared the safety and efficacy of lumbar epidural catheter fixation via Lock-it epidural catheter clamp (LECC) and subcutaneous tunneling of epidural catheter (SETC) in orthopedic surgical patients in a prospective, randomized study.
MATERIALS AND METHODS A prospective, randomized, double blind study was designed on 100 patients of ASA grade I and grade II between 18-58 years of age of either sex, admitted in K D Medical College, Hospital and Research Centre, Mathura (U.P.) and scheduled for elective orthopedic surgical procedure under combined spinal epidural anesthesia. The study protocol was approved by Institutional Ethics Committee and written informed consent was obtained from all patients. The pre anesthetic check-up included a detailed medical and surgical history and previous anesthetic exposure with its outcome. General examination included general condition, built, weight, heart rate, blood pressure, respiratory rate and presence of cyanosis, anemia, clubbing, jaundice or edema. A careful thorough systemic examination was done to rule out any cardiovascular, respiratory, gastrointestinal and neurological or any other systemic illness. Careful examination of spine was done to rule out any spinal deformity like kyphoscoliosis and any infection at the site of performing the combined spinal epidural procedure. Routine biochemistry investigation included hemoglobin level, total leucocyte count, differential leucocyte count, platelet count, coagulation profile, blood sugar level, blood urea and serum creatinine. ECG and X- ray chest were done in patients where indicated and those above 40 years of age along with other relevant investigations. Patients posted for elective lower limb orthopedic procedures, with no contraindication to receive a neuraxial block were included in the study. After taking detailed history and clinical examination, the patients were excluded from the study on the basis of below mentioned criteria: Patients with systemic hypertension, hepatic, renal, endocrine and cardiac dysfunctions, morbid obesity (body weight >20% of the ideal body weight), patients with infection at the site of entry for spinal and epidural block, spinal deformities, deranged coagulation profile, patients with known hypersensitivity, those on antihypertensive medications, patients with pre-existing neurological disabilities and who were unstable to understand, express and communicate visual analog scores and those who refused to give consent. A total of 100 patients of either gender aged 18-58 years were divided randomly into two groups using simple sealed envelope method. All patients in group I and group II (n=50 each) received combined spinal epidural anesthesia in the lumbar region (L3-L4 OR L4-L5) through midline approach. Local anesthetic was infiltrated at the site of skin puncture for all patients to ensure patients comfort during the procedure. Loss of resistance technique was used to identify the epidural space. 3 ml of 0.5% hyperbaric bupivacaine was administered via 25 G spinal needle in subarachnoid space. 4 cm length of the epidural catheter was placed in the epidural space and fixed by either subcutaneous tunneling or using Lockit epidural device clamp. All catheters were flushed with 3 ml of lignocaine with adrenaline to rule out catheter kink and to ensure the desired placement of the catheter post fixation. Epidural catheter was fixed using subcutaneous tunneling of the catheter in group I or STEC (n=50) using a Tuohy 18 G epidural needle for making a vertical tunnel. A 3-4cm long tunnel was created in the subcutaneous plane 1.5 cm away from the catheter puncture site. A small loop of catheter was left between the epidural puncture site and the tunnel entry and was maintained using a sterile gauze placed under it. Then it was covered using tegaderm dressing and the rest of the catheter was fixed over the right shoulder along its length on the back of the patient using dynaplast. In group II or LTEC (n=50) the epidural catheter was fixed using the Lock-it epidural catheter clamp after tunneling of catheter through the central eyelet of the fixator device after its exit from the skin. Once the adhesive from the device sticked on the skin and the clamp was closed over the catheter. 3 ml of 2% lignocaine was administered one and a half hour after block placement. The entire fixation assembly was checked and redone in case of any obstruction to drug injection. About 0.5% bupivacaine was given as 5-7 ml bolus through epidural catheter every hour. The parameters recorded were length of the catheter inserted, any unusual bleeding, incidence of needle stick injury and catheter snapping during fixation. Likert score of -2 to +2 was used to evaluate patients comfort during the procedure. An independent observer evaluated all the parameters and the technique used to secure the epidural catheter was not revealed to the co-observer. Continuous post-operative infusion using an infusion pump was administered to all the patients using 0.125% bupivacaine. Any inward and outward migration, erythema and induration were reported at the time of catheter removal at 72 hours after the surgery. Migration more than 1 cm was considered significant enough to be reported. Visual analog score (VAS) more than or equal to 5 was treated with rescue analgesic (tramadol 50mg intravenous). During the first 72 hours when epidural analgesia was delivered, pain scores were noted every 4 hours. Data were expressed as mean with standard deviation for continuous variables. Categorical variables were expressed as numbers and percentages. The statistical analysis was performed using statistical package for social sciences (SPSS, VERSION 25.0). Independent samples t-test was applied to continuous variables. The categorical variables such as gender, Likert score, bleeding, kink, VAS score and outward migration were analyzed by chi square test. P<0.05 was considered as statistically significant.
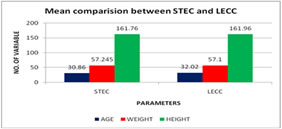
RESULTS 100 patients undergoing lower limb orthopedic surgical procedures requiring combined spinal epidural anesthesia were included in the study. In 70% of the patients the neuraxial block was successfully placed in first attempt. In rest of the patients repeated attempts i.e. more than or equal to 2 attempts were required due to obesity (50%), less distance between the two spinous processes (40%) and faulty technique (10%). The two groups were comparable with respect to the age, height and body mass index as shown in Table 1 and bar diagram 1. The orthopedic procedures performed were ilizarov procedure (40%), joint replacement (40%), acetabular fractures (10%) and fracture both bone lower limb (10%). Pre-operative deep vein thrombosis prophylaxis was given in around 40% of the patients and block was given according to the ASRA guidelines. Table 1
STEC- subcutaneous tunneling of epidural catheter, LECC- Lock-it epidural catheter clamp, S.D- standard deviation In STEC group tunneling was totally unacceptable in 27 patients, unacceptable in 11 patients whereas 3 patients were either indecisive or neutral. It was acceptable only in 9 patients. Figure 1: Bar diagram 1
In LECC group the fixation technique was acceptable in 10 patients and completely acceptable in 40 patients. The comparative statistics of Likert score is presented in Table 2 (P=0.005). Table 2: Patients comfort during epidural fixation-Likert score
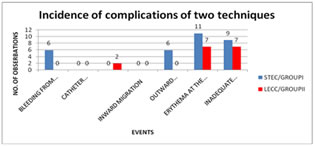
STEC- subcutaneous tunneling of epidural catheter, LECC- Lock-it epidural catheter clamp 6 of the patients with bleeding from the tunneling site were on DVT prophylaxis. The complications are enumerated in Table 3 and bar diagram 2. Table 3: Incidence of complications with the two techniques
STEC- subcutaneous tunneling of epidural catheter, LECC- Lock-it epidural catheter clamp
Figure 2: Bar diagram 2
DISCUSSION Inadequate analgesia is mostly caused by migration of epidural catheter and thus can only be prevented by securely fixing the epidural catheter to prevent its dislodgement. Fixation technique should be comfortable for the patient and non-cumbersome for the operator. Our study shows that tunneling procedure is less acceptable and uncomfortable for the patient. Similar results were deducted by Kumar and Chambers6 and they also expressed safety concerns about tunneling and suggested catheter hygiene and daily catheter examination to decrease morbidity during tunneling. Using needle sheath as a stabilizer to guide the hub of the needle7 during tunneling can help decrease morbidity. Tunneling decreases the incidence of catheter migration but does not guarantee the same according to Burstal et al.8 Outward and inward catheter migration can be successfully prevented by LECC by about 88% as shown by Clark et al.4 In our study, the patients in STEC group showed increased incidence (22%) of poor pain scores and required rescue analgesics for the same. Thus apart from catheter migration, other factors like pain threshold level and the complexity of procedure being done contribute towards inadequate analgesia. 30% incidence of failed epidural analgesia due to incorrect primary catheter placement, migration of the catheter after correct initial placement and inadequate drug dosing have been reported by Hermanides et al.9 Tripathi and Pandey left a loop of catheter on the skin while tunneling to prevent catheter dislodgement.10 The outward traction on the catheter is decreased as a result of the interposed loop. There was local inflammation at the site of tunneling in 29% of patients according to their study and using the epidural needle twice also increases the chances of infectious complication. Retraction of the catheter inside the skin can lead to snapping of the catheter. Recommendations on the length of catheter to be left in epidural space and indication of surgical retrieval of the catheter fragment has been outlined by Hobaika.11 Exploratory laminectomy has to be done in case of neurological changes in the patient, if catheter is in the subarachnoid space or if the tip emerges out of the skin. In one case report where the catheter had snapped a little away from its point of exit from skin and this was managed as a routine epidural with the filter assembly attached to the severed end.12 In our study 2 patients in LECC group experienced catheter obstruction due to obesity and significant lumbar lordosis leading to improper contact between skin and device. Lock-it epidural catheter clamp ensures no movement of catheter after clamping. Thus small portion of the catheter can kink between the skin and device. People’s attitudes, opinions or perceptions were measured by Likert scale using a set of questions. Baroudi et al.13 validated this five point scale with -2 to +2 as available scores to quantify the patient’s satisfaction after anesthetic exposure. Sharma A et al.14 compared lock-it epidural catheter clamp with subcutaneous tunneling of catheter and found that there was less erythema at the site of fixation than the site of tunneling, less incidences of catheter obstruction and inadequate analgesia. Odor, P et al.15 found in their study that lock-it epidural catheter clamp provides best securement of catheter as compared to tegaderm or Epi-fix device. Tunneling was disliked and unacceptable in our study by maximum number of patients.
CONCLUSION Lock-it epidural catheter clamp is a more efficacious, safe, comfortable and acceptable method to prevent epidural catheter migration as compared to subcutaneous tunneling of the catheter.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home