|
Table of Content - Volume 22 Issue 2 - May 2022
A comparative study of epidural 0.5% bupivacaine with buprenorphine and 0.5% ropivacaine with buprenorphine for elective lower limb surgeries
Ashwini A1, Nabeela Basri2*
1Associate Professor, 2Senior Resident, Department of Anesthesiology, Kempegowda Institute of Medical Sciences, Bangalore, INDIA. Email: nabeelabasrir@gmail.com
Abstract Background: The present study was conducted to evaluate the efficacy of 0.5% Bupivacaine and 0.5% Ropivacaine, with Buprenorphine with regard to the sensory blockade, motor blockade, duration of analgesia and hemodynamic response. Methods: 60 patients undergoing elective lower limb surgeries were randomly selected and divided into two groups of 30 each. Group B patients received 14.5 ml of 0.5 % Bupivacaine with 150 micrograms (0.5 ml) of Buprenorphine through the Epidural route. Group R patients received 14.5 ml of 0.5% Ropivacaine with 150 micrograms (0.5 ml) of Buprenorphine through the Epidural route. The onset of sensory blockade, motor blockade, duration of motor blockade, duration of sensory analgesia and hemodynamic changes were assessed. Results: The mean time for onset of sensory block in Bupivacaine with Buprenorphine (Group B) was 10.63±1.59 min and 10.23±1.63 in Ropivacaine with Buprenorphine (Group R). The mean time for onset of Motor block in Bupivacaine with Buprenorphine (Group B) was 28.87±3.35 and 29.17±2.23 in ropivacaine with buprenorphine (Group R). The mean duration of the motor blockade in Bupivacaine with Buprenorphine (Group B) was 282.87 min±21.03 min and 241.7min±22.5min in Ropivacaine with Buprenorphine (Group R). The mean duration of sensory analgesia in Bupivacaine with Buprenorphine (Group B) was 390.07min±15.44min and 389.7min±16.51min in Ropivacaine with Buprenorphine (Group R). There was no significant difference in heart rate and blood pressure between the two groups. There was no episode of bradycardia in either of the group. 10% of the patients in Group B and 7% in Group R had hypotension. Conclusions: Epidural 0.5% Ropivacaine with Buprenorphine and Epidural 0.5% Bupivacaine with Buprenorphine were found to be clinically similar in terms of onset of sensory and motor blockade. However, the duration of motor blockade was shorter in the Ropivacaine group when compared to the Bupivacaine group. Because of the shorter duration of action of 0.5% Ropivacaine, it can be used, in lower limb surgeries effectively as early mobilisation can be done in the postoperative period. Keywords: Bupivacaine, Ropivacaine, Buprenorphine, Epidural anaesthesia, Lower limb surgery.
INTRODUCTION The word pain is derived from the Greek word poine (penalty).1 The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”. Other than psychological trauma, pain is shown to affect the physiology of almost all the systems including respiratory, cardiovascular and metabolic profiles thereby increasing morbidity.2 Epidural anaesthesia is the most commonly used technique for providing not only perioperative surgical anaesthesia but also postoperative analgesia in lower abdominal and lower limb surgeries.3 It provides dynamic analgesia. Allowing patients to resume normal activities unlimited by pain.4 It is possible to perform all surgical procedures while the patient is under GA, but GA has its disadvantages and limitations. Therefore regional anaesthesia is preferred for lower extremity surgeries. The advantages of regional anaesthesia are5
Epidural anaesthesia has a high success rate and patient satisfaction. There is evidence for reduced blood loss and low risk of other complications in orthopaedic surgeries; hence in recent years, the epidural technique has gained widespread popularity and has been well accepted by both the patient and surgeon.3 Epidural anaesthesia is more versatile in providing anaesthesia, analgesia and treatment of chronic disease syndromes. It provides better postoperative pain control and a more rapid recovery from surgery. It also reduces the incidences of hemodynamic changes and PDPH as the dura is not pierced.2 Epidural anaesthesia is nowadays considered the gold standard anaesthetic technique for lower limb orthopaedic surgeries. A local anaesthetic–opioid combination provides superior analgesia during the perioperative period. This combination limits rapid regression of sensory blockade and possibly decreases the dose of local anaesthetic administered.6 Analgesia provided by epidural opioids is superior to that with systemic opioids. Bupivacaine, a local anaesthetic is a widely used drug in epidural anaesthesia as it is a long-acting amide local anaesthetic.6 Its introduction in 1957 was a very important step in the evolution of regional anaesthesia. It is commercially available as a racemic mixture containing equal proportions of S (-) and R (+) isomers. Despite its popularity, it is associated with several side effects like an unwanted motor blockade, CNS and cardiotoxicity. There have been many reports of even death attributed to bupivacaine-induced cardiotoxicity after accidental intravenous injection. These cases resulted in continued search for new and a safer anaesthetic agents.5 Ropivacaine is a new long-acting amide local anaesthetic that is unique among local anaesthetics as it is prepared as a single enantiomer rather than a racemic mixture. Studies have shown that there is a more profound motor blockade with ropivacaine and sensory anaesthesia comparable in length to bupivacaine and has thus been introduced as an answer to bupivacaine-induced cardiotoxicity although it is available for a long time internationally. Ropivacaine, registered for use in 1996, has only been launched recently in Indian markets since 2009.6 Opioids are routinely added to local anaesthetics in blockade to prolong the duration of postoperative analgesic effects.7 Due to easy availability, cost-effectiveness, lack of significant side-effects like respiratory depression and sedation, longer duration of action, lipophilic nature, high affinity for μ receptor, buprenorphine has been selected for study as an adjuvant to local anaesthetics in epidural anaesthesia.8 Buprenorphine is thebaine derivative, mu-receptor partial agonist and antagonist. It is effective in relieving moderate to severe pain. Buprenorphine is a long-acting, highly lipophilic opioid, which has proved to be a promising analgesic, by the epidural and intrathecal route.9 It is found to be about 25 times more potent than morphine and has a low level of physical dependence. When compared to local anaesthetics, it offers good analgesia while allowing early ambulation of the patient by sparing sympathetic and motor nerves.10 Objectives: The present study was conducted to evaluate the efficacy of 0.5% Bupivacaine with Buprenorphine and 0.5% Ropivacaine with Buprenorphine, in terms of onset, duration of sensory and motor block, duration of analgesia, hemodynamic parameters and side effects in patients undergoing lower limb orthopaedic surgeries under epidural anaesthesia. Though Ropivacaine and Bupivacaine have been used with many opioids there are only few studies available to compare the effects of the addition of epidural Buprenorphine to Bupivacaine and ropivacaine for lower limb surgeries.
METHODS This is a prospective comparative study conducted from December 2018 to September 2020 in the Department of Anaesthesia, Kempegowda Institute of Medical Sciences, a tertiary care centre. Study Subjects: The study was conducted among the subjects who were undergoing elective lower limb surgeries under epidural anaesthesia at our tertiary care centre. Inclusion Criteria: Sixty patients of ASA I and II aged between 18 and 60 years, posted for elective lower limb surgeries under epidural anaesthesia were included in our study. Exclusion Criteria: The study subjects who had contraindications for epidural anaesthesia, pregnant women, patients with a history of convulsions and neurological problems, cardio-respiratory diseases, those with known spinal deformities, with history of hepatic and renal diseases and those with a known psychiatric disorder were excluded from the study. Study Procedure: 60 patients undergoing elective lower limb surgeries were randomly selected using a random number table and were divided into two groups of 30 each consecutively. The first group (Group B) received 14.5 ml of 0.5 % Bupivacaine with 150 micrograms (0.5 ml) of Buprenorphine through the Epidural route and the second group (Group R) received 14.5 ml of 0.5 % Ropivacaine with 150 micrograms (0.5 ml) of Buprenorphine through Epidural route. Outcomes: Outcomes were assessed and compared in terms of time taken for the onset of sensory blockade, motor blockade, duration of motor blockade, duration of sensory analgesia and hemodynamic changes. Side effects were also recorded and compared. Statistical Analysis: Data were entered into a Microsoft Excel data sheet and analyzed using SPSS 22 version software. Categorical data was represented in the form of frequencies and proportions. Chi-square and Fisher’s exact test were used as tests of significance for qualitative data. Continuous data were represented as mean and standard deviation. An independent t test was used as a test of significance to identify the mean difference between two continuous quantitative variables. MS Excel and MS word were used to obtain various types of graphs such as bar diagrams and line diagrams. A P-value of < 0.05 was considered statistically significant.
RESULTS The mean age in the Bupivacaine with Buprenorphine (group B) was 44.87 years and for Ropivacaine with Buprenorphine (group R), mean age was 42.87 yrs. In group B, there were 13 females (43%) and 17 males (57%) and in group R there were 10 females (33%) and 20 males (67%). There was no significant difference among the groups in respect to age and gender distribution and both the groups were comparable (P > 0.05) [Table-1] Table 1: Demographic Distribution
ONSET OF SENSORY BLOCKADE The mean time for onset of sensory block in bupivacaine with buprenorphine (Group B) was 10.63±1.59 min and 10.23±1.63 in ropivacaine with buprenorphine (Group R). The onset of sensory block in group B was delayed for a few seconds compared to group R, but it was not statistically significant as p-value was 0.340. [Table-2] ONSET OF MOTOR BLOCKADE The mean time for onset of motor block in Bupivacaine with Buprenorphine (Group B) was 28.87±3.35 and 29.17±2.23 in ropivacaine with buprenorphine (Group R). Statistically there was no significant p value between the two groups (p value 0.685). [Table-2] Table 2: Duration of motor block and sensory analgesia in mins comparison between two groups
DURATION OF MOTOR BLOCKADE: The mean duration of the motor blockade in Bupivacaine with Buprenorphine (Group B) was 282.87±21.03 and 241.7±22.5 in Ropivacaine with Buprenorphine (Group R). Statistically, there was a highly significant p-value between the two groups (p value < 0.001*). The significant p-value concluded that the duration of motor blockade in group Ropivacaine with Buprenorphine (Group R) was significantly lower than the Bupivacaine with Buprenorphine (Group B). [Table-2] DURATION OF SENSORY ANALGESIA: The mean duration of sensory analgesia in Bupivacaine with Buprenorphine (Group B) was 390.07 min±15.44 min and 389.7 min±16.51 min in Ropivacaine with Buprenorphine (Group R). Statistically there was no significant p-value between the two groups. [Table-2]
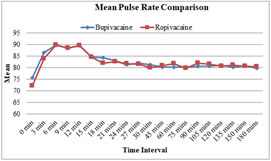
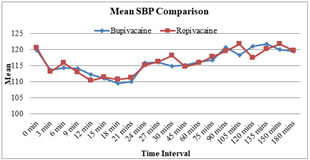
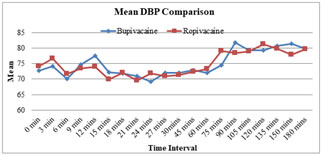
Graph 1 Graph 2 Graph 1: Line Diagram Showing Mean Pulse Rate Comparison between two groups at different intervals of time; Graph 2: Line Diagram Showing Mean SBP Comparison between two groups at different intervals of time There was no significant difference between the two groups with respect to pulse rate when recorded at different intervals. The mean systolic blood pressure was compared between the two groups over time intervals. It was found that there was no significant difference between the two groups. The mean diastolic blood pressure was compared between the two groups over time intervals. It was found that there was no significant difference between the two groups. [Graphs 1-3]
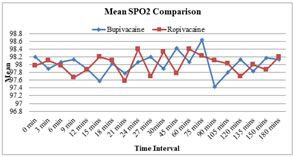
Graph 3 Graph 4 Graph 3: Line Diagram Showing Mean DBP Comparison between two groups at different intervals of time; Graph 4: Line Diagram Showing Mean SPO2 Comparison between two groups at different intervals of time The mean saturation was compared between the two groups over the time intervals. It was found that there was no significant difference between the two groups. [Graph 4] ECG was normal throughout the procedure between the two groups. No significant difference was seen. Table 3: Distribution of Side Effects among the two groups
In Bupivacaine with Buprenorphine (Group B), 10 % had hypotension, 7% had nausea and vomiting 0 % and in Ropivacaine with Buprenorphine (Group R), 7% had hypotension, 3% had nausea and 3% had vomiting. There was no significant difference between the two groups in the occurrence of side effects (P > 0.05). [Table-3]
DISCUSSION Epidural anaesthesia is the most commonly used technique for providing perioperative surgical anaesthesia and postoperative analgesia in lower limb surgeries. It provides dynamic analgesia allowing the patient to resume normal activities unlimited by pain. When compared to spinal anaesthesia epidural anaesthesia provides less frequency of hypotension and there is no limitation on the duration of surgery. Ropivacaine is a long-acting local anaesthetic containing pure s (-) - enantiomer. It differs from bupivacaine in substitution of a propyl group for butyl group on piperidine rings tertiary nitrogen atom and it consists of a single (s) - enantiomer. Neuronal and cardiac Na+ channels action of the (s) - isomer of the piperidine containing local anaesthetic are less potent than the (R) isomer which makes Ropivacaine less potent than Bupivacaine. Buprenorphine is the most widely used epidural opioid analgesic for orthopaedic surgeries, it is 30 times more potent than morphine and has been associated with a lower incidence of delayed respiratory depression. Because there is no rostral spread, the addition of opioids along with local anaesthetic decreases the dose of local anaesthetic. So with less volume of local anaesthetic adequate, a longer duration of analgesia is achieved and less systemic toxicity. The aim of our study was to compare the efficacy 0.5 % Bupivacaine with Buprenorphine and 0.5 % Ropivacaine with Buprenorphine for epidural anaesthesia in lower limb surgeries. Our study design consisted of 60 patients aged between 18-60 years. Belonging to ASA I and II, 60 patients were randomly divided into two groups’ of 30 patients each. Group B (Bupivacaine with Buprenorphine) patients received 14.5 ml of 0.5 % Bupivacaine with 150 micrograms (0.5 ml) of Buprenorphine and Group R (Ropivacaine with Buprenorphine) patients received 14.5 ml of Ropivacaine with 150 micrograms of Buprenorphine. The following parameters were measured
Demographic Data: Demographic data comparing age and sex showed no statistically significant difference between the two groups. The onset of Sensory Blockade Block: The mean time for onset of sensory block in Bupivacaine with Buprenorphine (Group B) was 10.63±1.59 min and 10.23±1.63 in ropivacaine with Buprenorphine (Group R). The onset of sensory block in group B was delayed for a few seconds compared to Group R but it was not statistically significant as p-value was 0.340 Brockway MS et al. conducted a study comparing 0.5 %, 0.75 % and 1 % Ropivacaine with 0.5 % and 0.75 % Bupivacaine. Their study also concluded that there was no significant statistical difference between the two groups in the onset of sensory block or motor block Wolff A.P et al. conducted a study comparing 0.5 % 0.75 % and 1 % Ropivacaine with 0.5 % Bupivacaine administered epidurally in patients undergoing elective hip surgeries. In their study, they concluded there was no statistical difference between the two groups in respect to the onset of sensory and motor blockade. Brown D et al. compared 0.5 % Ropivacaine and 0.5 % Bupivacaine for epidural anaesthesia in patients undergoing elective lower limb surgeries. They observed no difference between the two groups in the onset of sensory and motor blockade. Finucane B T et al. conducted a study comparing 0.5 %, 0.75 % and 1 % Ropivacaine and 0.5 % Bupivacaine for epidural anaesthesia in patients undergoing abdominal hysterectomy. They found no difference in the onset of sensory and motor blockade between the two groups. Mc Glade DP et al. compared 0.5 % Ropivacaine and 0.5 % bupivacaine in lumbar epidural anaesthesia for lower limb orthopaedic surgery. They also concluded they were no statistical difference between the two groups in the onset of sensory and motor blockade. The above study results were similar to our study in respect to the onset of sensory block. So, it can be concluded that there is no difference in onset of sensory blockade between 0.5 % Bupivacaine with Buprenorphine and 0.5 % Ropivacaine with Buprenorphine in Epidural anaesthesia. The onset of Motor Block: The mean time for onset of motor block in Bupivacaine with Buprenorphine (Group B) was 28.87±3.35 and 29.17±2.23 in group R, statistically there was no significant p-value between the two groups (p-value 0.685) Brockway MS et al. conducted a study comparing 0.5 %, 0.75 % and 1 % Ropivacaine with 0.5 % and 0.75 % Bupivacaine. Their study also concluded that there was no significant statistical difference between the two groups in the onset of motor block. Wolff A.P et al. conducted a study comparing 0.5 % 0.75 % and 1 % Ropivacaine with 0.5 % Bupivacaine administered epidurally in patients undergoing elective hip surgeries. In their study, they concluded there was no statistical difference between the two groups in respect to the onset of motor blockade. Brown D et al. compared 0.5 % Ropivacaine and 0.5 % Bupivacaine for epidural anaesthesia in patients undergoing elective lower limb surgeries. They observed no difference between the two groups in the onset of motor blockade. Finucane B T et al. conducted a study comparing 0.5 %, 0.75 % and 1 % Ropivacaine and 0.5 % Bupivacaine for epidural anaesthesia in patients undergoing abdominal hysterectomy. They found no difference in the onset of motor blockade between the two groups. Mc Glade DP et al. compared 0.5 % Ropivacaine and 0.5 % bupivacaine in lumbar epidural anaesthesia for lower limb orthopaedic surgery. They also concluded they were no statistical difference between the two groups in the onset of motor blockade. The above results were similar to our study in respect to the onset of motor blockade. So it can be concluded that there is no difference in the onset of motor blockade between 0.5 % Bupivacaine with Buprenorphine and 0.5 % Ropivacaine with Buprenorphine in Epidural anaesthesia. Duration of Motor Blockade: In our study, the mean duration of the motor blockade in Bupivacaine with Buprenorphine (Group B) was 282.87 min±21.03 min and 241.7min±22.5 min in Ropivacaine with Buprenorphine (Group R). Statistically there was a highly significant p-value between the two groups (p value< 0.001*). The significant p value concludes that the duration of the motor blockade in group Ropivacaine with Buprenorphine (Group R) was significantly lower than the Bupivacaine with Buprenorphine (Group B). Wolff A.P et al. conducted a study comparing 0.5 % 0.75 % and 1 % Ropivacaine with 0.5 % Bupivacaine administered epidurally in patients undergoing elective hip surgeries. In their study, they concluded that Ropivacaine produced less intense motor blockade compared to Bupivacaine. Brockway MS et al. conducted a study comparing 0.5 %, 0.75 % and 1 % Ropivacaine with 0.5 % and 0.75 % Bupivacaine. In the study, they concluded that there was an earlier return of motor function in the Ropivacaine group compared to the Bupivacaine group. David L Brown et al. conducted a study comparing 0.5 % Ropivacaine with 0.5 % Bupivacaine for epidural anaesthesia in a patient undergoing lower limb surgery. In their study, it was concluded that bupivacaine produced a longer duration of motor block compared to Ropivacaine. McClure et al. conducted a study comparing Bupivacaine and Ropivacaine. In their study, they concluded that Ropivacaine produced less intense and shorter duration of motor blockade compared to Bupivacaine. Cekmen N et al. conducted a study comparing a single dose of Epidural Ropivacaine and Bupivacaine in arthroscopic surgery. They observed that Bupivacaine produced a more intense and longer duration of motor blockade compared to ropivacaine. The above studies observation was similar to our study in respect to the duration of motor blockade. Hence we can conclude that duration of motor block is less intense and shorter duration with Ropivacaine than Bupivacaine. Duration of Sensory Analgesia: In our study, the mean duration of sensory analgesia in Bupivacaine with Buprenorphine (Group B) was 390.07 min±15.44 min and 389.7 min±16.51 min in Ropivacaine with Buprenorphine (Group R). Statistically there was no significant p-value between the two groups. David L Brown et al. conducted a study comparing 0.5 % Ropivacaine with 0.5 %Bupivacaine for epidural anaesthesia in a patient undergoing lower limb surgery. In their study concluded that there was no significant difference in the duration of sensory analgesia between the two groups Brockway MS et al. conducted a study comparing 0.5 %, 0.75 % and 1 % Ropivacaine with 0.5 % and 0.75 % Bupivacaine. In their study also they concluded that no difference was seen between the two groups in the duration of analgesia. Wolff A.P et al. conducted a study comparing 0.5 % 0.75 % and 1 % Ropivacaine with 0.5% Bupivacaine administered epidurally in patients undergoing elective hip surgery. They observed that there was no difference in the duration of analgesia between the two groups. Hemodynamic Changes: In our study, there was no significant difference in heart rate and blood pressure between the two groups. There was no episode of bradycardia in either of the group. 10 % of the patients in Group B and 7 % in Group R had hypotension which was treated with graded doses (3 mg) of inj Mephenteramine In a study conducted by Wolff AP et al. comparing epidural ropivacaine with bupivacaine in hip surgeries, blood pressure decreased in both the groups and no statistical difference was seen between the groups. Brockway MS et al. conducted a study comparing 0.5 %, 0.75 % and 1% Ropivacaine with 0.5 % and 0.75 % Bupivacaine, blood pressure decreased by 20 % in both the groups over the first 20 minutes and heart rate increased over the first 15 min and tend to decrease slightly lower than the baseline after that, but there was no significant difference between the two groups. Finucane BT et al. concluded in their study that epidural administration of Bupivacaine produced similar changes in hemodynamic parameters as epidural Ropivacaine. The above studies results are the same as our study in respect to hemodynamic parameters
CONCLUSIONS Based on the present clinical study, we conclude that 0.5 % Ropivacaine with Buprenorphine given epidurally in lower limb surgeries provide adequate anaesthesia as 0.5 % Bupivacaine with Buprenorphine and 0.5 % Ropivacaine with Buprenorphine has a shorter duration of motor block compared to 0.5 % Bupivacaine with Buprenorphine. The onset of sensory and motor blockade and duration of analgesia was similar between the two groups i.e., 0.5 % bupivacaine with Buprenorphine and 0.5 % Ropivacaine with Buprenorphine. The hemodynamic changes were also not significant between 0.5 % bupivacaine with Buprenorphine and 0.5 % Ropivacaine with Buprenorphine. Hence we found 0.5 % Ropivacaine with Buprenorphine and 0.5 % Bupivacaine with Buprenorphine to be clinically similar in onset sensory and motor blockade characteristics except that Ropivacaine produces a shorter duration of motor blockade. Because of the shorter duration of motor blockade of Ropivacaine, it can be used in lower limb surgeries effectively as early mobilisation in the post-operative period can be done.
REFERENCES
Policy for Articles with Open Access
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home