|
Table of Content - Volume 22 Issue 3 - June 2022
Anaesthetic management of a man with five chambered heart - A case of a rare large left ventricular pseudoaneurysm
Pratika Bhokare1*, Antony George2, Grace Maria George3, Job Wilson4, Jacob Abraham5
1Fellow In Cardiac Anaesthesia, 2,3,4,5Consultant, Consultant & HOD, Department of Cardiac Anaesthesiology, Lisie Heart Institute, Lisie Hospital, Kochi – 682018, INDIA. Email: pratika16691@yahoo.com
Abstract Background: Left ventricular (LV) aneurysm is a serious complication of acute myocardial infarction. The aneurysm is mostly asymptomatic, but large LV aneurysm may cause heart failure, tachyarrhythmias or even sudden death.[1] The term Ventricular aneurysm is usually used to describe dyskinesia or local expansile paradoxical wall motions.[2] Favaloro and colleagues described LVA as a full thickness scar tissue replacement of the left ventricular wall, usually containing thrombus and attached to pericardial sac by adhesions.[3] Surgical intervention is required for LV aneurysm, if it is associated with heart failure, in view of low survival rate.[4] Here, we present a 49 year-old male patient with a recent history of Congestive cardiac failure, with LV pseudoaneurysm with clots and a triple vessel coronary artery disease. He was evaluated and posted for LV aneurysm repair and coronary artery bypass grafting (CABG). The aim of this case report is to highlight the role of the cardiac anesthesiologist in the perioperative management of this rare and complex condition, including the perioperative transesophageal echocardiogram assessment and postoperative recovery. Keywords: Left ventricular aneurysm, pseudoaneurysm, myocardial infarction, anesthetic management, transesophageal echocardiography, ventricular dysfunction.
INTRODUCTION LV aneurysm is a life-threatening complication, occurring as a sequela of myocardial infarction. True LV aneurysm consists of a region of thinned myocardium which is dyskinetic and comprises of full thickness of ventricular wall.5 Left ventricular pseudoaneurysm is LV wall rupture, contained by the pericardium, without any myocardial tissue in the wall. They are found more commonly in the postero-inferior wall followed by postero-lateral wall and anterior wall.7 LV aneurysms are linked to very high mortality rates of 35-40%. It is crucial to distinguish false aneurysm from true aneurysm, as large pseudoaneurysms almost always indicate surgical management due to high risk of rupture.8
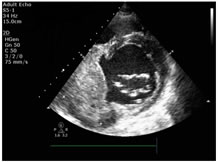
CASE HISTORY- The patient, a 49 year old man with history of breathlessness and paroxysmal nocturnal dyspnoea for one week. He was hemodynamically stable with q waves in leads III and aVf and t inversions in V5 and V6 with positive Troponin I. 2D Echo showed Global Hypokinesia with an LV ejection fraction of 30% with left ventricular pseudoaneurysm of size 9.8 x 8.8 cm at the basal inferior wall with a suspicious large layered clot. The coronary angiography revealed Triple Vessel Disease. The patient was received at our hospital, where 2D Echo revealed Aneurysmal Left Ventricular Basal Inferior Wall with large layered clot 8.2 x 6.4 cm, Ejection fraction of 33% and Moderate Mitral Regurgitation. Pre-anaesthesia evaluation was done. After confirmation of NBM, patient was taken in OT and monitors were attached. Under sedation and local anaesthesia, Arterial line was taken in the right brachial artery, a right femoral arterial catheter was inserted to facilitate IABP insertion if required; and a central venous line was taken in the Right IJV, 8.5 FR, 4 lumen. Infusions of Noradrenaline, Adrenaline, Vasopressin, Dobutamine, NTG, Dexmedetomidine and Tranexamic acid were started. Magnesium 1g was added in the IV fluid. Anaesthesia induction was done. Cis atracurium was used; with Sevoflurane for maintenance of anaesthesia. The Trans Esophageal Echocardiography revealed unruptured Left ventricular false aneurysm at the inferior wall of size 9.8 X 8.2 cm with a clot measuring 8 X 7.3 cm (Fig1). The patient had moderate to severe LV dysfunction and Moderate mitral regurgitation. Sternotomy was done (fig2) Heparin was given followed by cannulation of aorta and vena cava, hemodynamics were maintained with a MAP of 70-80 and patient was put on Cardio Pulmonary Bypass (CPB) with subsequent cardioplegia and systemic hypothermia. The aneurysm was found on the inferior surface of the LV and filled with about 250g of degenerated thrombus. Aneurysmectomy was done and defect was closed with PTFE patch. The aneurysmal wall was wrapped over repair and then CABG was done with 3 grafts. After an aortic clamp time of 102 minutes, aorta was de clamped. Inotropes and vasodilators were restarted on rewarming (Noradrenaline 0.02 mcg/kg/min, Dobutamine 2 mcg/kg/min and NTG 0.6 mcg/kg/min) While coming off of CPB, there was severe RV Dysfunction – inhaled Nitric Oxide was started. The Blood pressure continued to hover around MAP of 48 - 50 mmHg with decreased heart contractility. Intra-aortic Balloon Pump (IABP) was inserted at the time and augmentation was initiated at 1:1 ratio. The inotropic supports were increased at the time as follows: - NA 0.05 mcg/kg/hr, Vasopressin 0.04 units/min, NTG 3 mcg/kg/min, Dobutamine 3.5 mcg/kg/min and Adrenaline 0.05 mcg/kg/min. The Hb immediately after weaning off CPB was 6.8 g/dL and 2 units of whole blood were transfused to augment the oxygen carrying capacity. Continuous TEE assessment was done to assess the RV dysfunction. The RV dysfunction slowly improved and his hemodynamics improved. The inotropic supports were reduced and chest kept open for 24 hours to monitor bleeding. Post operatively the heart rate stayed at 100 - 110/min. Digoxin 0.25 mg and MgSO4 1g were administered. The urine output remained adequate throughout the post-operative period. Inotropes and ventilatory support were continued. Chest cavity was closed the next morning. The inotropic supports were reduced to a minimum with NA at 0.01 mcg/kg/min, Vasopressin 0.01 units/min and Dobutamine at 2.5 mcg/kg/min. All other supports were stopped. Patient was extubated on Post-Op Day 2. RV showed acceptable contractility. IABP was weaned on POD 3 and was removed on day 4; dobutamine was also weaned by day 4.
DISCUSSION LV Aneurysm is the most common complication following Myocardial infarction. These aneurysms are associated with complications like heart failure, ventricular arrhythmias, thrombo-embolization, ventricular ruptures, cardiac tamponade and eventually mortality. CT scan, MRI, Echo cardiography and Angiography are the various modes used to diagnose ventricular aneurysms.6 Pseudoaneurysms present with a high risk of rupture. However, true ventricular aneurysms can be operated electively. LV pseudoaneurysm is mostly located in the postero-inferior wall, whereas the true aneurysm is mainly located at apical and anterior walls.6,7 This patient was planned for surgery as he was symptomatic with large ventricular pseudoaneurysm and history of heart failure. Hypertension and tachycardia were avoided throughout the surgery. Continuous TEE monitoring helped to check to contractility status of the heart. The Mean BP was maintained at an optimum level (above 60 mmHg) for adequate perfusion of coronaries. Post CPB, in view of significant RV dysfunction, inhaled NO was initiated. RV dysfunction is an important predictor of ICU stay duration and morbidity. Ventricular interdependency needs to be in perfect balance for recovery of the patient. Mean arterial pressure, post CPB was maintained between 60-70mmHg in order to avoid any bleeding along the suture line. LV contractility was maintained using inotropes and IABP. Sufficient blood and blood products were administered. Concurrently, precautions must be taken to avoid volume overloading; by checking for LV contractility via TEE. Prolonged surgery coupled with prolonged CPB time and aortic cross clamp time can lead to severe myocardial dysfunction and thus, optimal management of such cases is important.
CONCLUSION A detailed pre-operative check-up with relation to diagnosis between true and pseudo aneurysm is crucial. The surgery included ventriculotomy with severe manipulation of the ventricle and an increase in the myocardial dysfunction. These patients are prone to rapid hemodynamic changes in the peri-operative period and thus, hemodynamic monitoring should be accurate as these patients have a narrow safety range for hemodynamic parameters. Balanced delivery of inotropes, vasopressors, vasodilators and inodilators is the key. Post-operative management plays an important role in the outcome of left ventricular pseudoaneurysm. Declaration of Patient Consent- The authors certify that they have obtained the appropriate consents for recording the data. The patient and relatives understand that their names will not appear in any of the documents and complete anonymity will be maintained. Figure 1: Size of the LV pseudoaneurysm clot as measured on Trans Thoracic Echocardiography pre operatively Figure 2: LV pseudoaneurysm as seen after sternotomy.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home