|
Table of Content - Volume 22 Issue 3 - June 2022
A study of effect of melatonin premedication on attenuation of haemodynamic responses to laryngoscopy and intubation
G K Kumar1*, G P Aravind2, R Shanthimalar3
1Professor, 2Post Graduate, 3Professor, Department of Anaesthesia, Government Chengalpattu Medical College Hospital, Chengalpattu. Email: drkumargk@gmail.com , drshanmal@gmail.com
Abstract Background: Laryngoscopy and endotracheal intubation provokes reflex hemodynamic responses leading to a marked increase in heart rate and blood pressure. Melatonin is used for sedation and anxiolysis. We studied these properties for reducing haemodynamic surge in intubation. Aim and objective: To study the effect of melatonin premedication on attenuation of haemodynamic responses to laryngoscopy and intubation Material and methods: Present study was a double-blind randomized control trial conducted on patients with ASA I and II undergoing general anaesthesia. Patients were randomly divided into 2 groups. Group A received oral melatonin tablets 6 mg (two tablets of 3 mg each), administered 120 min before surgery and Group B received 2 placebo tablets 120 min before surgery. Haemodynamic parameters like heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure were monitored pre operatively, intra operatively. Data was analysed with appropriate statistical tests. Results and Discussion: Melatonin Group patients showed statistically significant decrease in heart rate, SBP, DBP and MAP than placebo group patients to laryngoscopy and intubation(p<0.05).
INTRODUCTION Laryngoscopy and intubation is one of the commonly performed procedure in anaesthesia. During tracheal intubation, the laryngeal and tracheal sensory receptors are stimulated resulting in the release of endogenous catecholamine and causes tachycardia and hypertension in patients.1 This haemodynamic change It is usually well tolerated by normotensive patients, but even a shortest stimulation will lead to significant morbidity and mortality in Patients with recent myocardial infarction, hypertension, pre-eclampsia, gastrointestinal surgeries especially prolonged and major surgeries and cerebro-vascular pathology such as tumors, aneurysms or increased intracranial pressure.2-4 Various drugs has been utilized to prevent this haemodynamic surge like Lignocaine, opioid, vasodilator, Ca channel blocker, beta-blocker, Magnesium sulphate, Gabapentin and Pregabalin. All these agents are useful but not fully efficient to reduce haemodynamic stress response during laryngoscopy and endotracheal intubation. These drugs have some side effects and limitations.5,6 Melatonin (N‑acetyl‑5‑methoxytryptamine) is a pineal gland hormone which controls the circadian rhythm. It has been used for sleep disorders, perioperative anxiolysis and sedation, jet lag, cognitive and psychomotor functions.7-10 The blood pressure lowering effect is due to the specific binding of melatonin-to-melatonin receptors in the blood vessels, interfering with the vascular response to catecholamines. The blood pressure lowering effect could also be due to the sedative action of orally administered melatonin. The sedative effect is mainly due to binding at GABA‑A receptor and exerting its anaesthetic effect.11 Melatonin interferes with the peripheral as well as central autonomic system, causing a reduction in adrenergic outflow and resulting catecholamine levels.12 Melatonin causes relaxation of arterial wall smooth muscle by enhancing the availability of nitric oxide.13 Melatonin act via specific receptors melatonin type 1 or melatonin type 2 located peripherally in the blood vessels and centrally in blood pressure regulating area of the brain.14 It also has free radical scavenging effect leading to dilatation of blood vessels, and it may work via epigenetic mechanism at area postrema in the brain.15 Present study was conducted to study the effect of melatonin premedication on attenuation of haemodynamic responses to laryngoscopy and intubation Aim and objective: To study the effect of melatonin premedication on attenuation of haemodynamic responses to laryngoscopy and intubation
MATERIAL AND METHODS Present study was a double-blind randomized control trial conducted at a tertiary care centre. Study population was Patients of ASA I and II undergoing general anaesthesia. Inclusion criteria: 1. Patients with ASA grade I and grade II 2. Patients of either sex in age group of 20-45 years 3. Patients willing to participate in the study Exclusion criteria: 1. Patients with diabetes, hypertension, psychiatric illness, sleep disorders, obesity and drug allergy 2. Patients with intake of antipsychotics, sedatives, anxiolytics and antiepileptic drugs. 3. Patients with difficult intubation 4. Pregnant and lactating females Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. Data was collected with pre tested questionnaire. Data included sociodemographic data, clinical history and through clinical examination. Total 60 patients were studied. They were randomly divided into 2 groups. Group A received oral melatonin tablets 6 mg (two tablets of 3 mg each), administered 120 min before surgery and Group B received 2 placebo tablets 120 min before surgery. Vitamin D3 tablets were used as placebo and looked similar to melatonin tablets. Both patient and investigator were unaware of the type of drug. In the pre‑operative room, patients received study drugs. They were monitored for basic vitals. On receiving the patient in the operation theatre, routine monitoring was commenced which included heart rate, electrocardiogram, arterial SpO2, non‑invasive blood pressure (NIBP) and end‑tidal carbon dioxide (EtCO2). Two puffs of 10% lignocaine were sprayed on the larynx. All the patients were administered 100% oxygen for 3 min before induction. Glycopyrrolate 0.004 mg/kg and fentanyl 1 μg/kg were administered intravenously. Induction was attained with intravenous propofol 2 mg/kg intravenously mixed with preservative-free lignocaine hydrochloride. Succinylcholine was given intravenously 2 mg/kg to facilitate endotracheal intubation with proper sized well‑lubricated cuffed endotracheal tube by the same person each time. Maintenance of anaesthesia was attained with inhalation of isoflurane 1 minimum alveolar concentration; nitrous oxide: oxygen 40:60. Muscle relaxation was attained with vecuronium bromide administered in the dose of 0.06–0.08 mg/kg intravenously as loading dose and one‑fourth of the initial dose as maintenance doses. Mechanical ventilation was adjusted to maintain normocapnia (EtCO2 values of 35–38 mmHg). Intravenous infusion of injection diclofenac sodium 75 mg was administered slowly 15 min before completion of surgery for post‑operative analgesia. After completion of the surgery, neostigmine 50 μg/kg and injection glycopyrrolate 10 μg/kg were administered intravenously to reverse the residual neuromuscular blockade. Haemodynamic parameters like heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure were monitored pre operatively, intra operatively (immediately after induction, at laryngoscopy and intubation just after laryngoscopy and after intubation at 1,3,5 and 10 mins). Data was entered in excel sheet and analysed by SPSS version 22.0.
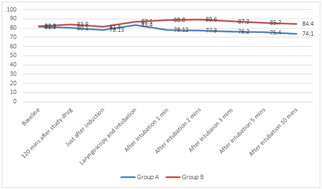
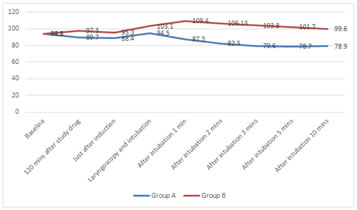
RESULTS In our study, we studied two groups with 30 patients each. Group A patients received tab. Melatonin 120 minutes prior to surgery and group B patients received placebo tablets 120 minutes prior to surgery. Table 1 shows comparison of different variables. ASA grade I patients were 13 and 14 in group A and group B respectively. Mean age of the patients in group A was 32.3±2.5 years and 31.7±2.1 years in group B. Male to female ration in group A was 17/13 while in Group B it was 18/12. Mean weight of the patients in group A was 56.5±4.8 kg and 57.3±4.3 kg in group B. Mean duration of surgery in group A was 70.12±9.6 mins and 72.13±10.1 mins in group B. Both the groups were comparable with respect to age, gender distribution, ASA grade, weight, duration of surgery (p>0.05). Figure 1 shows comparison of heart rate at different point of time in both the groups. Baseline heart rate in Group A and group B were 81.3±9.1 and 82.3±4.9 per minute respectively. Heart rate decreased in group A after 120 minutes to 80.1±9.8 per minute. On data analysis we found that statistically significant decrease in heart rate was observed in group A at laryngoscopy and intubation, and after intubation upto 10 minutes than Group B. (p<0.05) Systolic blood pressure (SBP) was 122.3±5.7 and 123.4±6.1 mm of Hg in group A and group B respectively. Melatonin group showed statistically significant decrease in SBP just after induction, at laryngoscopy and intubation, after intubation at 1,2,3,5 and 10 minutes. (p<0.05). (table 2) Table 3 shows Comparison DBP at different point of time in Melatonin and placebo group. In group A baseline DBP was 79.2±6.3 mm of Hg and it significantly decreased to 65.2±6.3 mm of Hg after 10 minutes of intubation. In group B baseline DBP was 79.4±5.7 mm of Hg and it increased to 85.7±3.8 mm of Hg after 10 minutes of intubation. Statistically significant change was observed in DBP at 120 minutes after giving the study drug, just after induction, at laryngoscopy and intubation, after intubation at 1,2 3,5 and 10 minutes. (p<0.05) Comparison of MAP in group A and group B was shown in figure 2. Baseline MAP were 93.8±5.4 mm of Hg and 94.1±6.2 mm of Hg in group A and group B respectively. Data analysis showed that statistically significant decrease was observed in Melatonin group than placebo group at different point of time like 120 minutes after study drug, just after induction, laryngoscopy and intubation, after intubation at 1,2,3,5 and 10 minutes. (p<0.05). In our study, we observed no complications like bradycardia, hypotension but nausea and vomiting was observed in one patient in each group. Two patients in placebo group observed restlessness but not in melatonin group.
Table1: Comparison of Melatonin and placebo group according to variables
Figure 1: Comparison of heart rate at different point of time in Melatonin and placebo group
Table2: Comparison of SBP at different point of time in Melatonin and placebo group
Table 3: Comparison of DBP at different point of time in Melatonin and placebo group
Figure 2: Comparison of MAP at different point of time in Melatonin and placebo group
DISCUSSION In our study, statistically significant decrease in heart rate was observed in group A at laryngoscopy and intubation, and after intubation upto 10 minutes than Group B. (p<0.05) Anxiolytic actions and analgesic effects of melatonin causes decrease in heart rate.16 Contrary to our study, no difference was observed in the changes of heart rate in the melatonin groups as compared to the placebo group in Mohamed AA et al.17 Melatonin group showed statistically significant decrease in SBP just after induction, at laryngoscopy and intubation, after intubation at 1,2,3,5 and 10 minutes. (p<0.05). Statistically significant change was observed in DBP at 120 minutes after giving the study drug, just after induction, at laryngoscopy and intubation, after intubation at 1,2 3,5 and 10 minutes. (p<0.05) In our study, Data analysis showed that statistically significant decrease was observed in Melatonin group than placebo group at different point of time like 120 minutes after study drug, just after induction, laryngoscopy and intubation, after intubation at 1,2,3,5 and 10 minutes. (p<0.05). Similar to our study, Mohammed et al. compared the role of oral melatonin 6 mg and 9 mg with placebo administered 1 h before surgery in attenuating pressor response to laryngoscopy and intubation. They observed that there was a reduction of blood pressure with regard to systolic, diastolic and mean blood pressure; and perfusion index in both melatonin groups as compared to the placebo group.17 Sewerynek et al. found a similar observation to our study that oral Melatonin in 1 mg dose reduces BP and also decreases catecholamine level after 90 min in humans.18 Russel, et al., stated that melatonin has a variety of actions; it may function to lower blood pressure. Moreover, melatonin has endothelium-relaxing effects, it is a potent scavenger of free radicals (which negatively influence blood pressure), and it may work via epigenetic mechanisms at the level of the area postrema to regulate blood pressure.19 Gupta et al. also noted the hemodynamic stability during laryngoscopy procedure and intubation when melatonin was given 120 min before the procedure. They observed that the patients were stable at all points of time as compared to the control group in terms of SBP, DBP, and MAP.20Arangino S et al. observed that melatonin may decrease the MBP in a healthy population.21 Rosenberg et al. in their study have also shown that melatonin has sympatholytic activity.22 In our study, there were no significant side effects such as bradycardia, arrhythmias, respiratory depression, restlessness, nausea and drug interactions. Various studies indicate that melatonin has an excellent safety profile. Kain et al. safely used 0.4 mg/kg oral melatonin in children.23
CONCLUSION Melatonin causes significant decrease in heart rate, SBP, DBP and MAP on laryngoscopy and intubation. It is effective and safe drug for use in intubation.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home