|
Table of Content - Volume 24 Issue 1 - 2024
Comparison of transforaminal epidural injection vs trigger point injection for low back pain
Ravi Bathia1*, Jadeja Chetna A2, Darshan N3, Devanshi Patel4
1Resident Doctor, 2(M.D, Fiapm), 3,4Resident Doctor, Department of Anesthesiology, P.D.U Medical College and Hospital. College, INDIA.
Email: ravibathia28@gmail.com, chetnagohil72@gmail.com, darshann59@gmail.com., devanshipatel0411@gmail.com.
Abstract Background: Lumbar transforaminal Epidural Steroid injection is frequently used intervention for lumbar radiculitis but associated with complications. Trigger-point therapy is useful adjunct in treatment of low-back pain. We compared efficacy and safety of transforaminal epidural injection with trigger point injections for chronic back pain. Aims: To compare the degree of pain relief, safety and to measure functional Improvement between TFESI and TPI for low back pain. Settings and Design: This is a Retrospective analytical study. Methods and Material: Records of last 5 years of patients attending the pain clinic at pdumc, Rajkot were searched Data of 90 patients who were given TFESI(GROUP E) and 90 patients who were given TPI (GROUP T)were collected. Statistical analysis used: Student t test used to compare VAS and ODI Scores between Two groups Results: VAS and ODI scores at 1st 3rd and 6th month of post procedure is less in TFESI group than in TPI group and are statistically significant Conclusions: Although TFESI is more effective than TPI, if we add TPI as a step-up procedure between conservative management and TFESI, in many patients more invasive procedures like TFESI and its complications can be avoided.
Key-words: Transforaminal Epidural steroid Injection, Trigger point Injection.
INTRODUCTION
Low back pain is a common disease which affects 15-20% population at any point of time, and common reason for young age morbidity, disability, work absenteeism. Lumbar disc herniation (LDH) results from the displacement of the nucleus pulposus inside the vertebral canal and causes nerve root pain.2 Epidural steroid injection has been used for treatment of lumbosacral radiculopathy. dorsal aspect of herniated disc.3 TPs are common sources of regional neuromusculoskeletal pain which occur as irritable spots in the skeletal muscle and may manifest as palpable nodules.2 Studies are there which shows that trigger points (TPs) are common in patients with radiculopathy. The presence of TP-related pain in radiculopathy, in addition to peripheral neuropathy, is a major factor of symptom aggravation.2 An active trigger point causes pain at rest. It also have referred pain pattern that is similar to the patient's pain complaint. This referred pain is felt not at the site of the trigger-point origin, but remote from it.4 TPs are usually managed byThe transforaminal epidural steroid injection (TFESI), when given under fluoroscopy guidance results in high concentration of corticosteroid at the target site on ventral aspect of the lumbar root sleeve and the Pharmacological agents, manual and physical therapy, dry needling, TP injection, and botulinum toxin injections.4 In vitro studies on human fibroblasts and chondrocytes show that glucose elevation to 0.5% to 0.6% (normal cell concentration is 0.1 %) results in stimulation of growth factor production by a variety of human cells, which includes fibroblasts and chondrocytes, within 2 hours.[11] we have taken 25% dextrose along with bupivacaine for stimulating regeneration and tissue healing.5 No studies are available in the literature comparing efficacy of transforaminal epidural steroid injection and trigger point injection in low back pain. So, we did this study to observe efficacy and safety of both modalities in low back pain patients with or without radiculopathy.
MATERIAL AND METHODS
This is a retrospective comparative analytical study of 180 patients who underwent intervention for low back pain.
Inclusion criteria: 1. Adult patients who underwent intervention (either TFESI or TPI) for low back pain, 2. Whose follow up for 6 months was available.
Exclusion criteria: 1. Previous back surgery. 2. History of substance abuse,
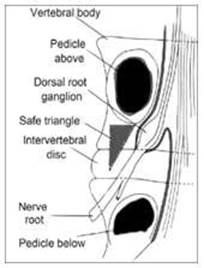
Records of last 5 years of patients attending the pain clinic at PDUMC, Rajkot were searched Data of 90 patients who were given TFESI and 90 patients who were given TPI were collected. TFESI injection was delivered through the 'safe triangle’ which comprised of a roof made by the pedicle of vertebra, a tangential base corresponding to the exiting nerve root and the lateral border of the vertebral body.
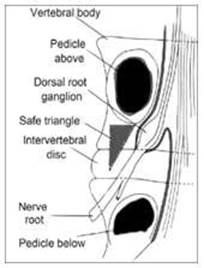
Image 1: Safe triangle.3
Roy, Chinmoy, Nilay Chatterjee, Satya Narayan Patro, Amit Chakraborty, GR Vijay Kumar, and Robin Sengupta. "The efficacy of transforaminal epidural steroid injections in lumbosacral radiculopathy." Neurology India 59, no. 5 (2011): 685.
Fluoroscopy was started to reach the foramen involving the nerve root with safe triangle approach with anterior- posterior view and then mild craniocaudal tilt was applied to view the upper end plate of the lower vertebra as a single line. Next step was to give 10–20-degree oblique tilt to place the needle under the pedicle using the tunnel view. Lateral X-ray confirmed the position of the needle at the ventral aspect of the foramen, then 1-2 ml of contrast medium Iohexol (omnipaque 300) was injected to outline the nerve root and Epidural spread. Drug was never injected if there was any doubt regarding the pattern of spread of the contrast.3 After the procedure, all patients were told to consult physiotherapist for back-strengthening exercises, starting afterday-7 of the procedure after the pain relief.3 In patients given TPI therapy, TPs were localized in prone position and compressed between the thumb and index finger and against the underlying bone and soft tissue. TP were diagnosed with local twitch response and jump sign and elicited pain at that hypersensitive spot. 2
A sterile 26-gauge needle attached to a 10-mL syringe containing 5 mL of bupivacaine (0.5%) and 5 mL of D25 was used for each patient. With the patient in the prone position, the sterile mixture was injected at the painful TP in all direction until the trigger points break using the technique suggested by Simons et al., whereby the syringe is held with the fingers of the dominant hand, the TP is held between the index and middle fingers of the non-dominant hand, and the needle is inserted into the muscle at a 90° angle. The patients were advised ice application and stretching exercises.

Image 2: Trigger Point Injection Technique.6
Image taken from Raj, P. Prithvi, and Serdar Erdine. Pain- relieving procedures: the illustrated guide. John Wiley and Sons, 2012.
Aii the patients were followed up for six months.
VAS Score, ODI Score and Complications of patients were noted pre procedure and at 1month, 3 months and 6 months For measuring VAS, a standard 100 mm scale was used where 0 corresponded to ‘no pain' and 100 to 'worst pain' patient had ever perceived.
The Oswestry Disability Index (also known as the Oswestry Low Back Pain Disability Questionnaire) is an extremely important tool that researchers and disability evaluators use to measure a patient's permanent functional disability. The test is considered the ‘gold standard’ of low back functional outcome tools
Scoring instructions
For each section the total possible score is 5: if the first statement is marked the section score = 0; if the last statement is marked, it = 5. If all 10 sections are completed the score is calculated as follows:
Example: 16 (total scored)
50 (total possible score) x 100 = 32%
If one section is missed or not applicable the score is calculated:
16 (total scored)
45 (total possible score) x 100 = 35.5%
Minimum detectable change (90% confidence): 10% points (change of less than this may be attributable to error in the measurement.
Interpretation of scores
0% to 20%: minimal disability: The patient can cope with most living activities. Usually, no treatment is indicated apart from advice on lifting sitting and exercise. 21%-40%: moderate disability: The patient experiences more pain and difficulty with sitting, lifting and standing. Travel and social life are more difficult and they may be
RESULTS
disabled from work. Personal care, sexual activity and sleeping are not
grossly affected and the patient can usually be managed by conservative means.
41%-60%: severe disability: Pain remains the main problem in this group but activities of daily living are affected. These patients require a detailed investigation.
61%-80%: crippled: Back pain impinges on all aspects of the patient's life. Positive
intervention is required.
81%-100%: These patients are either bed-bound or exaggerating their symptoms.
GROUP E: Transforaminal Epidural Steroid Injection GROUP T: Trigger point Injection.
(Respective figures and tables should be in the JPEJ format at the end of the document)
Table 1: Table of demographic characters(Age ,Sex)
|
F/M (SEX) |
0-20 (AGE) |
21-40 (AGE) |
41-60 (AGE) |
61-80(AGE) |
GROUP T |
60(66.6%)/30(33.3%) |
|
18(20%) |
50(55.5%0 |
22(24.44%) |
GROUP E |
58(64.45%)/32(35.55%) |
|
20(22.2%) |
54(60%) |
16(17.7%) |
The VAS at one month (33±13.16), three months (25±16) and six months (16.14±16) in group E was less than group T at one month (40.6±14.16), three month (33±18) and six month (26±22) respectively.
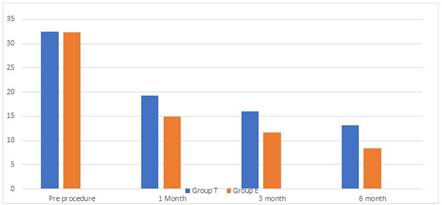
The ODI at one month (14.97±5.1), three months (11.6±5.9) and six months (8.36±7.29) in group E was less than group T at one month (19±6.4), three month (16±8.35) and six month (13.21±10.33) respectively.
The difference of VAS and ODI between group E and T was statistically significant.
There were no complications in Group T while 11.11% of patients developed minor complications in group E as shown in Table 2.
Table 2: Table of complications
Sr No Complications Group E Group T
1. Dizziness |
3(3.33%) |
0 |
2. Headache |
2(2%) |
0 |
3. Giddiness |
1(1%) |
0 |
4. Heaviness |
3(3.33%) |
0 |
5. Hypoesthesia And Paresthesia 1(2%) 0
TOTAL 10(11.11%)
DISCUSSION
Trigger points which are painful on compression located on skeletal muscle can also cause reffered pain, referred tenderness, motor dysfunction, and autonomic phenomena. The prevalence of trigger points in patients is between 30- 93%.4 Trigger points and tender points are different, but tender points do not cause referred pain. And TP cause referred pain which is not felt at the site but remote from it and radiating or spreading in nature.4 With firm presuure over TP, local twitch response and jump sign can be elicited. It is defined as transient visible or palpable contraction or dimpling of the muscle and skin as the taut band muscle fibres contract when pressure is applied. 4 Hong reported that either dry needling or injections lidocaine of trigger points provided immediate pain relief if local twitch response is elicited. Trigger points are commonly seen in painful skeletal diseases. It follows mechanical or neurologic stimulation. Timely trigger point’s injection has better prognosis and is important in the treatment of chronic lumbosacral radiculopathy. Pain scores get lower and SLR gets higher. It is also important to note that SLR may be positive due to active trigger points, which make it of diagnostic significance. Pain due to active trigger point may coexist with radiculopathy and add to the patient discomfort. Injection of trigger points is suggested as a good adjuvant therapy when these points coexist with Radiculopathy. Treatment of active trigger point is important because in cases of combined pain, standard treatment of radiculopathy may fail. Early treatment of trigger points can avoid unnecessary interventional and diagnostic procedures.7 Steroids can reduce edema and pressure on nerves and alleviate pain. E pidural steroid injection has a significant therapeutic role in mitigating the inflammatory component of radicular syndrome. TFESI is most commonly done intervention for low back pain with or without radicular pain, but These image-guided procedures have side effects like radiation exposure to patients, practitioners and operating room personnel.8 More over for TFESI, availability of fluoroscope, operation theatre and trained x-ray technician etc is essential while TPI can be done as office procedure, although sterile precautions are to be observed. However results shows that trigger point injection therapy in patients suffering from chronic lumbosacral radiculopathy with trigger points can significantly improve their recovery.7 The overall success rate of TFESI has been reported to be around 76–88%.8
VAS
Abdulla kocak et al. in their study observed that after TPI the VAS score improved from 7.55 pre procedure to 1.42 at 10 min, 0.55 at 30min and 0.41 at 60min and are statistically significant.13 Roy C et al. found in their study that, after TFESI the VAS Score improved from 9.2 pre procedure to 3.9 at one month,3.8 at 6 months,4.2 at one year.9 In our study, The VAS was low at all time intervals in TFESI group compare to TP group The difference of VAS between group E and T was statistically significant.

Figure 1: VAS Scores
ODI
Hong and Jin Et al. observed that after TPI the ODI scored improved from 31.71 pre treatment to 20.64 at one month and are statistically significant.14 In their study Roy et al., found that Ronald Morris score decreased from 18/24 to 10/24 at 6 months following TFESI.9 In our study, the ODI was less at all time intervals in TFESI group compare to TP group. The difference of ODI between group E and T was statistically significant.
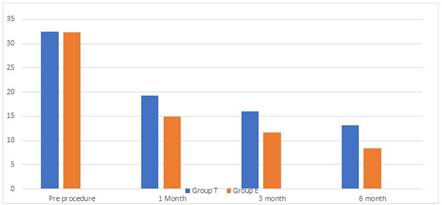
Figure 2: ODI scores
COMPLICATIONS
Common complications after TPI are pain, bleeding, infection, allergic reaction to anaesthetic agent, formation of hematoma, vascular injury, rarely pneumothorax when treating points in the cervicothoracic region using a needling technique.10 We did not encountered any complications in TPI group. The major complications after epidural injections including spinal abscess, spinal cord infarct, and epidural hematoma were documented as case reports. Some patients with spinal cord infarct had permanent neurologic deficits, while the other patients had recovery of neurological function after surgical or medical intervention.1 Chang A et al. found in their study, rate of minor complications in tfesi was between 2.4 and 9.6%.1 The most dangerous complication following TFESI is spinal cord infarction, resulting in paraplegia of which there are a few case reports.1 Viswanathan et al. in their studies found that Adverse effects related to steroids including pituitary-adrenal axis suppression, Cushing’s syndrome, osteoporosis, avascular necrosis of bone, myopathy, weight gain, fluid retention and hyperglycaemia, although rare, are theoretical possibilities following tfesi injections.9 The rate of minor complications in our study was 11.11% in group E.
REFERENCES
- Chang, Andrew, and Andrew T. Ng. "Complications associated with lumbar transforaminal epidural steroid injections." Current Pain and Headache Reports 24, no. 11 (2020): 1-6.
- Dernek, B., Adiyeke, L., Duymus, T. M., Gokcedag, A., Kesiktas, F. N., and Aksoy, C. (2018). Efficacy of Trigger Point Injections in Patients with Lumbar Disc Hernia without Indication for Surgery. Asian spine journal, 12(2), 232–237. https://doi.org/10.4184/asj.2018.12.2.232
- Roy, Chinmoy, Nilay Chatterjee, Satya Narayan Patro, Amit Chakraborty, GR Vijay Kumar, and Robin Sengupta. "The efficacy of transforaminal epidural steroid injections in lumbosacral radiculopathy." Neurology India 59, no. 5 (2011): 685.
- Alvarez, David J., and Pamela G. Rockwell. "Trigger points: diagnosis and management." American family physician 65, no. 4 (2002): 653.
- Pain Management Steven D. Waldman, MD, JD SAUNDERS ELSEVIER 1600 John F. Kennedy Blvd Edition 1,pg 1106.
- Raj, P. Prithvi, and Serdar Erdine. Pain-relieving procedures: the illustrated guide. John Wiley and Sons, 2012.
- Saeidian, Seyed Reza, Mohammad Reza Pipelzadeh, Saleh Rasras, and Masud Zeinali. "Effect of trigger point injection on lumbosacral radiculopathy source." Anesthesiology and pain medicine 4, no. 4 (2014).
- Garvey, Timothy A., Michael R. Marks, and Sam W. Wiesel. "A prospective, randomized, double-blind evaluation of trigger-point injection therapy for low-back pain." Spine 14, no. 9 (1989): 962-964.
- Viswanathan, Vibhu Krishnan, Rishi Mugesh Kanna, and
H. Francis Farhadi. "Role of transforaminal epidural injections or selective nerve root blocks in the management of lumbar radicular syndrome-A narrative, evidence-based review." Journal of Clinical Orthopaedics and Trauma 11, no. 5 (2020): 802-809.
- Hammi C, Schroeder JD, Yeung B. Trigger Point Injection. [Updated 2021 Sep 13]. In: StatPearls [Internet].
- Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK542196/
- He, Yubao, Lei Chen, Zhiyang Xu, Jieying Wang, and Bo Liu. "Lumbar transforaminal epidural block for treatment of low back pain with radicular pain." Nan Fang yi ke da xue xue bao= Journal of Southern Medical University 40, no. 12 (2020): 1804-1809.
- Jasper, Joseph F. "Lumbar retrodiscal transforaminal injection." Pain Physician 10, no. 3 (2007): 501.
- Kocak, Abdullah Osman, Ali Ahiskalioglu, Emre Sengun, Sultan Tuna Akgol Gur, and Ilker Akbas. "Comparison of intravenous NSAIDs and trigger point injection for low back pain in ED: a prospective randomized study." The American journal of emergency medicine 37, no. 10 (2019): 1927-1931.
- Hong, Jin Oh, Joon Sang Park, Dae Geun Jeon, Wang Hyeon Yoon, and Jung Hyun Park. "Extracorporeal shock wave therapy versus trigger point injection in the treatment of myofascial pain syndrome in the quadratus lumborum." Annals of rehabilitation medicine 41, no. 4 (2017): 582.
|
|
 Home
Home