Official Journals By StatPerson Publication
|
Table of Content - Volume 4 Issue 3 -December 2017
Comparative study of effect of intra-operative administration of ringer’s lactate, sterofundin, plasmalyte-A and kabilyte on ionic and acid base status
Anne Kiran Kumar1, A Chaitanya Pratyusha2*, J Kavitha3, Gopinath Ramachandran4
1,3Associate Professor, 2Sr. Resident, 4Professor and HOD, Department of Anaesthesiology and Intensive care, Nizams Institute of Medical Sciences, Hyderabad - 500082, Telangana, INDIA. Email: kirankumaranne@yahoo.com, chaitanyapa9@gmail.com, drkarunya@gmail.com, gopi59@hotmail.com
Abstract Aim: The aim of the study was to compare the effect of intra-operative administration of RL, sterofundin, plasmalyte-A and kabilyte on ionic and acid base status. Materials and Methods: This study was a prospective Monocentric Double blinded Randomised controlled trial conducted for 1 year during the period of February 2015 to February 2016. 80 patients undergoing surgery for less than 3 hours (surface surgeries of limited duration and minimal blood loss ) under general anaesthesia were divided into 4 groups of 20 each randomly. 20 were assigned to each of the four groups to receive lactated ringer’s solution (Group C), sterofundin (Group S), plasmalyte (Group P) and kabilyte (Group K) respectively. Results: No biologically significant inter-group differences were observed in the patient demographics. Intergroup comparison of baseline serum urea, serum creatinine and haemodynamic parameters revealed no statistically significant difference. Intergroup comparison of ABG parameters- pH, partial pressure of oxygen, partial pressure of carbon-di-oxide, lactate, glucose, potassium, calcium, chloride, sodium, bicarbonate, base deficit, anion gap and osmolality were studied at baseline, 1 hour, end of surgery and post-op (1 hour after extubation) and Haemodynamic parameters-heart rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, SPV, dPP were studied at baseline and15,30,45,60,75,90,105, 120 mins post induction. Though our main aim was only to study the effect of administering these four different intra venous crystalloids on ionic and acid base status haemodynamic parameters were studied with our assumption to show that they are comparable across the groups and do not contribute to the changes in acid base and ionic status. Intergroup comparison of ABG parameters revealed no statistically significant difference except for PaO2 measured one hour postoperatively (p=0.016), calcium measured at the end of surgery ( p=0.022) and calcium measured one hour postoperatively (p=0.002). Intergroup comparision of all the other ABG parameters revealed no statistically significant difference between the groups at different time points (baseline, 1hour, end of surgery, 1hour post-op). However significant within group difference was observed for some parameters at some time points compared with baseline. Intergroup comparison of haemodynamic parameters revealed a statistically comparable trend at all times( p> 0.05) except the heart rates 15 and 30 minutes post induction ( p= 0.028 and 0.041 respectively),MAP recordings at 15 minutes post induction(p=0.022) and SPV recordings at 45 (p=0.012), 60(p=0.007), 75(p=0.034) and 120(p=0.044) minutes post induction. All these statistically significant inter group changes in haemodynamic parameters were observed in the sterofundin group (S) compared with Ringer’s lactatae/control group (C). No statistically significant inter group difference was found in SBP, DBP and dPP measurements at any time of study. Conclusion: The use of balanced salt solutions in surface surgeries of limited duration and minimal blood loss is associated with stable ionic and acid- base profile and is not associated with significant advantage over Lactated Ringer’s solution. All the three balanced salt solutions used in our study i.e., plasmalyte-A, sterofundin and kabilyte gave similar outcomes with respect to electrolyte and acid-base status when compared with one another. Key Words: ringer’s lactate, sterofundin, plasmalyte-A and kabilyte.
Intra-operative fluid therapy is an integral part of anaesthesia management. In an attempt to prevent organ damage it is important to ensure adequate fluid and volume therapy. The composition and appropriate use of intravenous fluids should solely be dictated by the targeted fluid space, while there appears to be no merit in differentiating between intra-operative, peri-operative, postoperative and ICU settings1. There are good theoretical grounds for using colloids or plasma volume expansion as they cause less salt and water overload and oedema than crystalloids. The potential disadvantages of colloids are well known like renal toxicity, coagulation disturbance and at present have very few indications. Crystalloid solutions differ from each other due to their osmolarity and their amount of electrolytes. Lactated Ringer’s (RL) solution is being used in the peri-operative period to treat the pathological interstitial fluid deficiency caused by dehydration or haemorrhage. Consensus guidelines recommend the use of RL in preference to Normal Saline (NS) when crystalloid fluid therapy is indicated 2. Disma.N et al proposed that NS is associated with a very high risk of hyperchloremia compared to sterofundin 3. The use of RL on the other hand, is associated with increase in lactate levels which interferes with estimation of serum lactate levels in conditions of severe hypoxia. A balanced plasma adapted solution is a solution qualitatively and quantitatively similar to plasma. It’s use avoids development of hyperchloremic acidosis, while assuring the same volume effect as unbalanced solutions potentially reducing morbidity and mortality4. It is well known that peri-operative hyperchloremic acidosis is associated with morbidity but recently it has been proposed that hyperchloremia (chloride>110meq/l) per se causes adverse outcomes one of which is renal dysfunction. Plasma adapted solutions reduce the effects on acid base balance. Specifically they avoid dilutional acidosis caused by older generation solutions by replacing bicarbonate with metabolizable anions. Plasma adapted solutions cause fewer side effects than colloid or crystalloids, thus shortening the hospital stay. The new generation of electrolyte solutions applies metabolism of anions in the form of acetate and / or malate in preference to lactate. Several studies quote the beneficial effects of various molecules like acetate, malate, gluconate and calcium added to the newer generation of balanced salt solutions 5,6. Although all the balanced salt solutions have been prepared with composition similar to plasma there exists variation with respect to electrolyte composition, osmolarity, pH, buffers etc. It was believed that serum bilirubin and glucose increase with the use of plasmalyte-A due to presence of gluconate, but certain studies contradict this by quoting Plasmalyte-A as a better choice in living donors undergoing right hepatectomy7 and Diabetic ketoacidosis8. Increase in chloride and bicarbonate (released from malate) with the use of sterofundin has also been suggested though the hyperchloremia is less compared to NS. Multiple studies comparing different plasma adapted solutions with individual crystalloids and colloids are present. But to our knowledge there are no studies comparing three different balanced solutions and Lactated Ringer’s solution in the intra-operative period with respect to variations in electrolytes and acid base status. Hence the present study intended to compare various balanced salt solutions with respect to their effects on serum electrolytes, lactates, pH and other variables using ABG analysis. MATERIALS AND METHODS The study protocol was submitted to Institutional Research Ethics Committee, Nizam’s Institute of Medical Sciences and ethics approval was obtained. Written informed consent for participation in the study was taken from all the patients. This study was conducted for 1 year during the period of February 2015 to February 2016. This study was a prospective Monocentric Double blinded Randomised controlled trial. Blinding was achieved by avoiding the presence of the primary investigator at the time of study. The randomisation procedure was a simple computer generated. Eighty patients were included in this study. Sample size analysis was done using G-power analysis. There were no previous studies comparing four fluids for calculation of effect size. Hence using a Priori approximate effect size of 0.4,power of study 80% and alpha error of 0.5 the sample size was calculated to be 19 in each group. 80 patients undergoing surgery for less than 3 hours under general anaesthesia were divided into 4 groups of 20 each randomly. 20 were assigned to each of the four groups to receive lactated ringer’s solution (Group C), sterofundin (Group S), plasmalyte (Group P) and kabilyte (Group K) respectively. Inclusion Criteria: Patients with ASA I and ASA II, patients within age group of 18 to 65 years, those patients who underwent surgery with general anaesthesia of less than duration of 3 hours (limited duration surgeries with minimal blood loss). Exclusion Criteria: Patients with diabetes mellitus, renal abnormalities, cardiac ailments, surgeries such as gastric outlet obstruction, surgeries involving large fluid shifts and major blood loss, any neuraxial blockade, prolonged surgeries requiring urinary catheterisation, cardiac surgeries and surgeries involving use of tourniquet. Patients were pre-medicated with oral Alprazolam 0.5 mg and ranitidine 150 mg on the night before and morning of surgery. After shifting patient to operation theatre, 18 G intravenous and 20G arterial cannulation was done in all patients after infiltration with 2% Lignocaine local anaesthesia. The standard monitoring used were electrocardiogram, pulseoximetry, invasive blood pressure, temperature and end tidal carbondioxide. Depending upon the group allocated, patients were started on a specified intravenous fluid for the preoperative fasting hours and replacement for this deficit (50% in first hour, 25% in 2nd hour and 25% in 3rd hour ), hourly maintenance and evaporative and blood loss replacement hourly. Baseline pulse rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, Systolic pressure variation and pulse pressure variation were noted. Baseline arterial blood gas was done. All the patients were pre-medicated with inj fentanyl 2µg/ kg followed by pre-oxygenation for 3 minutes. Induction was done with inj Thiopentone sodium in a titrated dose of 4-5mg/kg till the loss of eyelash reflex. After checking adequacy of mask ventilation, inj atracurium 0.5mg/kg was given for muscle relaxation. Patients were manually ventilated for 3min and then intubated with appropriate size endotracheal tube. Mechanical ventilation was done by volume controlled mode with tidal volume of 8-11ml/kg and inspiratory and expiratory ratio of 1:2. Respiratory rate was adjusted to maintain the end tidal carbondioxide within 35±5 mm of Hg. Intraoperative SPV was maintained within limits of 5 to 15 mm Hg and the MAP was maintained above 60mmHg with adequate fluid infusion and vasopressor (phenylephrine 0.5-1 microgram/kg) if needed. Intra-operatively patients were maintained on nitrous oxide, oxygen and isoflurane mixture (1 MAC) and intermittent boluses of inj Atracurium 0.25mg/kg. Normal body temperature was maintained using forced air warming device. Inj Paracetamol 1gm was given for analgesia in the intra-operative Period. At the end of surgery patients were reversed with inj neostigmine 0.05mg/kg and inj glycopyrrolate 0.01mg/kg. They were extubated after thorough oral suctioning and monitored in the post anesthesia care unit. Study Parameters: Arterial Blood Gases: Arterial blood gas sampling for analysis and studying various parameters was done at baseline, 1hour after baseline, end of surgery and 1 hour after extubation. The following parameters have been studied : pH, paO2(mmHg), paCO2 (mmHg), Lactate (mmol/L), Glucose (mg/dL), Calcium (mmol/L), Sodium (mmol/L), Potassium (mmol/L), Chloride (mmol/L), Bicarbonate (mmol/L), Base Deficit (mmol/L), Anion gap (mmol/L), Osmolality (mmol/Kg). All samples were analyzed using a blood-gas analyzer (ABL700, Radiometer, Copenhagen, Denmark). The analyzer measures the parameters using ion- selective electrodes at 37 degrees. Haemodynamic parameters: The following parameters were studied at baseline and at 15 minute intervals thereafter : Heart rate - HR (Beats/mt), Systolic blood pressure - SBP (mmHg), Diastolic blood pressure - DBP (mmHg), Mean arterial pressure - MAP (mmHg), Systolic pressure variation - SPV (mmHg), Pulse pressure variation – dPP (%) Rescue measures: The following rescue measures were followed for any deviation from the study protocol.
Though our main aim was only to study the effect of administering these four different intra venous crystalloids on ionic and acid base status haemodynamic parameters were studied with our assumption to show that they are comparable across the groups and do not contribute to the changes in acid base and ionic status. Data were expressed as mean and standard deviation for continuous variables (weight, age, HR, SBP, DBP, MAP, ABG parameters). Data was analysed using Statistical Package for the Social Sciences (SPSS) version 16. Skewness and kurtossis of data was evaluated for accepting normality of distribution. Baseline values of hemodynamic parameters were normally distributed. Comparison of continuous data between groups was done using one way analysis of Variance (ANOVA of means). P value less than 0.05 was considered statistically significant between groups. Post hoc analysis was performed to identify the place of significance both between and within the groups and p value of less than 0.05 was considered significant. RESULTS
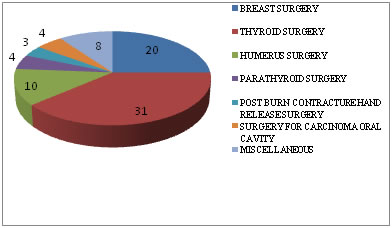
A total of 80 patients were recruited in our study. The types of surgical procedures performed in our study are illustrated as below:
Graph 1:
Miscellaneous – superficial swellings such as soft tissue swelling, parotid swelling, brachial cyst etc.
Table 1: Demographics with inter group comparisons (described as mean± standard deviation for age, height, weight and absolute numbers for gender)
Table 1 shows 37.5% of the total study population were men and the mean age was 41.4 yrs in our study. No biologically significant inter-group differences were observed in the patient demographics.
Table 2: Baseline parameters with intergroup comparison (mean±SD).
Table 2 shows that no statistically significant inter group difference was found in baseline blood urea, serum creatinine and haemodynamic parameters.
Table 3: Intergroup comparision of pH
*significant within group difference compared with baseline Intergroup comparision of pH revealed no statistically significant difference between the groups at different time points (baseline, 1hour, end of surgery, 1hour post-op)
Table 4: Intergroup comparison of partial pressure of oxygen, partial pressure of carbondioxide, lactate and glucose
*significant within group difference compared to baseline
Table 4 shows the intergroup comparison of PaO2 measured one hour postoperatively (p=0.016), revealed statistically significant difference between the groups. Intergroup comparison of partial pressure of carbondioxide, lactate and glucose revealed no statistically significant difference between the groups at different time points (baseline, 1hour, end of surgery, 1hour post-op). Table 5: Intergroup comparison of calcium, sodium, potassium and chloride
Table 5 shows intergroup comparison of calcium measured at the end of surgery ( p=0.022) and calcium measured one hour postoperatively (p=0.002), revealed statistically significant difference between the groups. Intergroup comparison of sodium, potassium, chloride revealed no statistically significant difference between the groups at different time points (baseline, 1hour, end of surgery, 1hour post-op) Table 6: Intergroup comparison of bicarbonate, base deficit, anion gap and serum osmolarity (Mean±Standard Deviation).
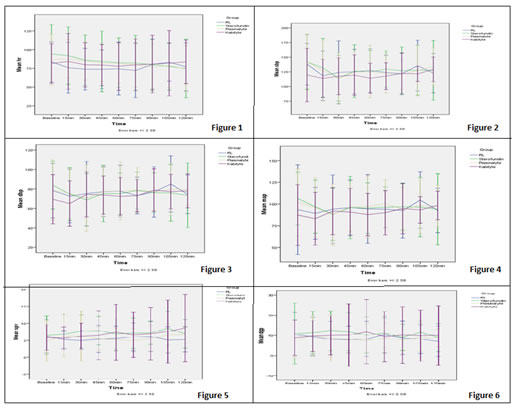
*significant within group difference compared with baseline Table 6 -Intergroup comparison of bicarbonate, base deficit, anion gap, serum osmolarity revealed no statistically significant difference between the groups at different time points (baseline, 1hour, end of surgery, 1hour post-op) Legend Figure 1: Heart rate at different time intervals in the four groups; Figure 2: Systolic blood pressure at different time intervals in the four groups; Figure 3: Diastolic blood pressure at different time intervals in the four groups; Figure 4: Mean arterial pressure at different time intervals in the four groups; Figure 5: SPV at different time intervals in the four groups; Figure 6: dPP at different time intervals in the four groups
Figure 1 shows the average heart rates compared between the study groups which were computed to be not significant statistically at all times( p> 0.05) except the Heart rates 15 and 30 minutes post induction ( p= 0.028 and 0.041 respectively). This statistically significant difference was observed in the sterofundin group(S) compared with Ringer’s lactate /control group(C). Figure 2 shows systolic blood pressure changes in four groups were comparable and statistically no significant difference was noted among the readings during study period. Figure 3 shows that diastolic blood pressure recordings showed a statistically comparable trend on intergroup analysis at all time points of measurements. (p> 0.05). Figure 4 shows that MAP recordings showed a statistically comparable trend on intergroup analysis at all time points of measurements. (p> 0.05) except at 15 minutes post induction ( p = 0.022). This statistically significant difference was observed in the sterofundin group (S), compared with Ringer’s lactate/control group (C) Figure 5 shows that SPV recordings showed a statistically significant difference on intergroup analysis at 45 (p=0.012), 60(p=0.007), 75(p=0.034) and 120(p=0.044) minutes post induction. This statistically significant difference was observed in the sterofundin group (S), compared with Ringer’s lactate/control group (C). Figure 6 shows that no statistically significant inter group difference was found in dPP measurements at any time of study.
DISCUSSION Research for the development of an ideal intravenous fluid to be used in the perioperative period is still ongoing. The best choice of fluid remains a topic of debate from ages inspite of multiple types of fluid being available in the market. The advantages and disadvantages of each fluid have been extensively investigated in many preclinical and clinical studies. In the meanwhile depending on the general condition, type of surgery and several other factors, a particular intravenous fluid becomes the choice. The present study was conducted to compare three different balanced salt solutions with a first generation unbalanced crystalloid with an anticipated variation in ionic and acid base status. The acid base analysis was expected to vary with respect to the composition of fluid, tonicity, osmolarity and volume infused. The study population belonged to normal physical status except for the concerned surgery related disease which did not involve major fluid shifts or losses. Our study results showed significant variation in the lactate and glucose levels in the RL group which was due to the conversion of lactate to bicarbonate and gluconeogenesis. Plasmalyte and Kabilyte group also showed an increase in the glucose levels over time. This could have been due to surgery related stress induced hyperglycemia. The absence of metabolizable anions like acetate in RL had resulted in the declining trend of bicarbonate and BD. The four fluids were comparable between each other with respect to acid base status. The variable composition of all the four fluids with respect to their in vitro pH, electrolyte composition (chloride, sodium, calcium) and other anions such as lactate is expected to cause a difference in final patient ionic and acid base status. On the contrary, intergroup comparison of ABG parameters in our study did not reveal any statistically significant values except for calcium levels measured 1 hour after induction and at the end of surgery. Calcium levels were maintained within normal limits with administration of sterofundin which contains calcium whereas other study fluids caused a slight decrease in calcium levels though not clinically significant. This is consistent with the finding in a study by Zdenek Zadak et al., comparing sterofundin and plasmalyte in healthy volunteers which showed sterofundin to cause a significant increase in serum calcium (though within normal physiologic limits)9. This might be of importance in prolonged surgeries or in patients with altered calcium levels. Though the in vitro pH of the fluids is variable and different from the normal plasma pH, the body’s buffering systems which include the liver, the kidneys and the lungs maintain a normal pH. Despite of some of the study fluids having a relatively higher levels of chloride (ringer’s lactate and sterofundin) compared to plasma, though less than that in normal saline, there is no significant change in blood chloride levels. This emphasises the fact that balanced salt solutions do not produce hyperchloremia which can be detrimental. All the fluids had within the group difference when pO2 was considered. This is because the baseline values had been taken on room air and the last value which is taken 1 hour after surgery was with oxygen by classical mask. In our study this could not be of any clinical significance. But this can be important when the oxygen consumption for metabolism of various ions like lactate, gluconate, malate and acetate are concerned with large fluid volumes and patients with impaired oxygenation. In routine clinical practice crystalloids are the choice of peri-operative fluid therapy. The first generation unbalanced fluids still remain the most commonly used fluids peri-operatively. However with the balanced solutions being available in the market, the trend is drifting towards their use. There are several studies comparing normal saline with lactated Ringer’s solution, normal saline with one of the balanced solutions. Several studies have already proven the superiority of RL over NS 2,10,11,12,13,14. However no studies have been conducted comparing the various balanced salt solutions with one another and with RL. In the present study the haemodynamic variations were not much different between the groups grossly. With respect to heart rate there was minimally significant difference when sterofundin and Plasmalyte were compared with RL at 15mins. The same trend was seen with diastolic blood pressure and mean arterial pressure in both groups. At about 45, 60, 75 and 120 mins the SPV had statistically significant difference between the Sterofundin group compared to RL. This variation can be attributed to depressant effects of anesthetic agents and the volume replacement with RL might be less effective than compared to other fluids. But yet over a period beyond 2 hours all the parameters had settled to normalcy. However the haemodynamic variations within each group showed statistical significance in certain parameters. The sterofundin group had an initial high heart rate which dropped to a statistically significant value over time and by the end of surgery came back to the baseline values. The SBP variations in this group followed the same trend as heart rate. The plasmalyte group showed a similar trend in heart rate and SBP variations. The Kabilyte group had statistically significant variation in MAP, DBP, SPV and DPP. These variations also could have been due to the depressant effects of anaesthetic agents rather than due to the type of fluid used. RL has been used for decades as peri-operative fluid. These hemodynamic variations were minimal and negligible. Hence all the fluids can be used for per-operative maintenance and replacement requirements without gross changes in haemodynamics. Ringer’s lacatate has been used for decades as perioperative fluid and these balanced salt solutions are comparable with respect to hemodynamics as per our study. Hence all the fluids can be used for perioperative maintenance and replacement requirements without gross changes in hemodynamics. The main aim of perioperative fluid management is maintenance of euvolemia which is regulated finely and efficiently in normal conditions by balanced salt solutions. This study therefore implies that RL and three balanced salt solutions can provide adequate homeostasis in the perioperative period in normal patients for surface surgeries. Mcfarlane et al compared plasmalyte and normal saline in the intra-operative period and concluded that usage of balanced salt solutions avoids intra-operative changes in electrolytes and acid base status 15. Another study by Zdenek Zadak comparing plasmalyte with sterofundin in healthy volunteers states the beneficial effects of acetate and malate in buffering physiological acid base status and ion fluctuation9. They also observed increase in serum ionised calcium concentration after sterofundin while it is decreased after plasmalyte. Raghunathan K et al; conducted a retrospective cohort study of patients admitted with sepsis, not undergoing any surgical procedures, and treated in an ICU by hospital day 2. They used propensity score matching to control for confounding and compared in-hospital mortality and other parameters after resuscitation with balanced versus with no-balanced fluids which showed resuscitation with balanced fluids was associated with a lower risk of in-hospital mortality16 Limitations: This study cannot be extrapolated to patients with multiple comorbidities and in surgeries with major fluid shifts. Hence to prove the effectiveness of balanced salt solutions in higher ASA grade patients and in major surgeries there is a need to conduct larger trials.
CONCLUSION The use of balanced salt solutions in surface surgeries and surgeries of short duration without major blood loss in patients of ASA 1 and 2 category is associated with stable ionic and acid- base profile and is not associated with significant advantage over Lactated Ringer’s solution. All the three balanced salt solutions used in our study i.e., plasmalyte-A, sterofundin and kabilyte gave similar outcomes with respect to electrolyte and acid-base status when compared with one another.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home