Official Journals By StatPerson Publication
|
Table of Content - Volume 5 Issue 3 -March 2018
Comparison of intracuff dexamethasone, lignocaine and normal saline on post extubation response - A prospective study
Soumya M V1, Sanjeev G M2*
1Senior Resident, 2Associate Professor, Department of Anaesthesiology, District Hospital, Chamarajanagar Institute of Medical Sciences, Chamarajanagar-571 313, INDIA. Email: soumyamv23@gmail.com
Abstract Background: Endotracheal intubation, being a definitive method has been known to cause post-intubation airway related adverse effects, including postoperative cough, restlessness, hoarseness, sore throat, bronchospasm, and laryngospasm. Cough induced by endotracheal tube can result in potential dangerous complications including hypertension, tachycardia, dysrrhythmia, increased intraocular pressure, increased intracranial pressure, wound dehiscence etc. Also intubation causes irritation and inflammation of airway. Sore throat and hoarseness incidence varies from 14.4 to 50%. Lignocaine administered intracuff has repeatedly been shown to reduce the incidence of post-intubation airway related adverse effects. Dexamethasone, a potent corticosteroid by its anti-inflammatory actions, reduce the incidence of postoperative cough, restlessness, hoarseness and sore throat. Aim and Objectives: The aim of this study is to evaluate and compare the effectiveness of intra-cuff dexamethasone and lignocaine with normal saline as a control group, in reducing post-extubation airway related adverse effects like incidence of cough, sore throat, and hoarseness. Methodology: Study was conducted on 150 patients,divided in three groups, belonging to ASA physical status Grade I and Grade II. ETT cuffs in the first to third groups will be filled with normal saline, dexamethasone, and 2% lidocaine, respectively. The patient will be assessed for coughing on the ETT, restlessness before extubation and hoarseness in the recovery area before discharge. Hemodynamic indices, and incidence of post-extubation sore throat, cough and hoarseness at 1 hour, 6 hour, 12 hours was assessed. The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data Results: Lignocaine used to inflate the cuff of an endotracheal tube results in better tolerance of the endotracheal tube. Dexamethasone has lesser incidence of cough, sorethroat, hoarseness compared to lignocaine but not statistically significant. AMBU cuff pressure manometer is reliable for intracuff measurement. Key Words: intracuff dexamethasone, lignocaine.
Respiration normally involves a well-developed neurophysiological process that enables the exchange of air by inspiration and expiration through well adapted anatomical structures. The airway extends from the nostrils and lips to the terminal alveoli. The basic indications for endotracheal intubation in the operating room are airway protection, maintenance of patent airway, application of positive pressure ventilation and maintenance of adequate oxygenation.11 Intubation causes irritation and inflammation of airway. Sore throat and hoarseness incidence varies from 14.4 to 50%.2 Incidence and severity of sore throat post-intubation is related to cuff design, cuff pressures etc. Cuff pressures above 30 cm of H2O are shown to reduce trachea mucosal microcirculation.3. Post-intubation airway related adverse effects, includes postoperative cough, restlessness, hoarseness, sore throat, bronchospasm, and laryngospasm. Lignocaine diffusion (first described by Sconzo et al (1990).6) was possible as the ETT cuff is semi-permeable, thus making it a potential drug reservoir.4 6 Studies using topically applied steroid, intravenous dexamethasone and inhaled fluticasone propionate have shown favourable results in reducing postoperative sore throat.7,8,9,10 The Endotracheal tube cuff pressure manometer fills, monitors and adjusts cuff pressure of low pressure endotracheal, endobronchial and tracheostomy tubes. They help in minimizing damage to the mucous membranes of the tracheal wall when used to monitor cuff pressure Thus the purpose of this study was to study is to evaluate and compare the effectiveness of intra-cuff dexamethasone and lignocaine with normal saline as a control group, in reducing post-extubation airway related adverse effects like incidence of cough, sore throat, and hoarseness. MATERIALS AND METHODS Source of Data: The study was conducted on 150 patients admitted for various surgeries to be done under general anesthesia. Method of Collection Of Data Procedure: After having obtained institutional ethics committee approval and written, informed consent, 150 ASA physical status Grade I and Grade II patients, of either sex, aged between 18 to 60 years with surgery lasting between 30 to 360 minutes were considered. They were distributed into 3 groups of 50 patients each, randomly according to computer generated randomized table. A detailed pre-anesthetic evaluation was done including history and general examination. All patients will receive Tab. Alprazolam 0.5mg and Tab. Pantoprazole 40mg the night before sleeping and was kept nil per oral from 12am onwards. Patients were shifted to OT. An intravenous line was secured with 18 gauge cannula; a slow infusion of Lactated Ringer’s solution was started. Airway cart was kept ready. In the OT, standard monitoring included non-invasive blood pressure monitoring, pulse oximetry, electrocardiogram and capnograph. The patients were connected to the monitors and the pre-induction systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), heart rate (HR) and oxygen saturation (SPO2) are recorded. All patients were given Inj. Glycopyrrolate 0.01mg/kg, Inj. Midazolam 0.02mg/kg, Inj. Ondansetron 4 mg. After preoxygenation 100% oxygen for three minutes of the patient, anesthesia was induced with Inj. Fentanyl 1.5mcg/kg and with Inj. Propofol 2mg/kg. On loss of verbal contact, assuring face mask ventilation was possible, a bolus dose of Succinylcholine 1.5mg/kg was then administered. Single use polyvinyl chloride ETTs (Portex® Profile tracheal tube) with low-pressure-high-volume cuffs, of inner diameter size 7.0-7.5 mm for females and 8.0-8.5 mm for males was used. Direct laryngoscopy was then performed using either a Macintosh 3 or 4 laryngoscope blade followed by intubation. The ETT cuffs will then be inflated according to the randomized protocol. The ETT cuffs in the first to third groups was filled with normal saline, dexamethasone, and 2% lidocaine, respectively. The tracheal tube cuff was injected with fluid at a peak airway pressure of 20 cm H2O until no leakage could be heard.22 The initial cuff pressure was measured and recorded with a cuff pressure gauge. Patients, who had intubation unsuccessful on the first attempt, were excluded. Anaesthesia was then maintained with a 50% -50% Oxygen-Nitrous oxide mixture, isoflurane and vecuronium 0.05mg/kg. i.v bolus of vecuronium bromide was repeated intermittently to maintain one to two twitches on train-of-four stimulation of ulnar nerve. At the end of the surgery, the cuff pressure was again measured and recorded. Isoflurane was discontinued, 100% oxygen was administered and residual neuromuscular blockade antagonized with glycopyrrolate 0.01 mg/kg and Neostigmine 0.05 mg/kg. Oral suctioning was done with care under direct vision just before extubation. Upon fulfilling extubation criteria, the patient was extubated. 100% oxygen was administered via face mask. The patient was assessed for coughing on the ETT, restlessness before extubation and hoarseness in the recovery area before discharge. An anesthesiologist assessed the patient during emergence for hemodynamic indices, and incidence of post-extubation sore throat, cough and hoarseness at 1hr, 6hr, and 12hours. The incidence of post-extubation sore throat and severity of post-extubation sore throat was evaluated with the visual analogue score scale (VAS, 0-10 ) at 1hr, 6 hours,12hours 24hours in the recovery room.
Table 1: Pain scores12
Table 2: Hoarseness was similarly graded on a 4 point scale.13
Table 3: Cough was similarly graded:13
Statistical Methods: Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean±SD (Min-Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance. The following assumptions on data are made. Assumptions: 1. Dependent variables should be normally distributed, 2. Samples drawn from the population should be random, and cases of the samples should be independent. Analysis of variance (ANOVA) has been used to find the significance of study parameters between three or more groups of patients. Chi-square/Fisher Exact test has been used to find the significance of study parameters on categorical scale between two or more groups. Statistical software: The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data and Microsoft Word and Excel have been used to generate graphs, tables etc.
OBSERVATIONS AND RESULTS One hundred and fifty (150) patients in ASA grade I and II of either sex meeting the inclusion criteria, posted for elective surgery under general anaesthesia were selected for the study. The study was conducted to evaluate the effectiveness and safety of endotracheal tube cuffs filled with lignocaine, saline or dexamethasone on post extubation sequelae. Study was A comparative three group study design.Age, Gender distribution and Type of Surgery distribution in three groups of patients studied had no significant difference in mean. However, there was significant difference in duration of surgery between groups. All the three groups had almost similar proportions of subjects within first two category. Highest numbers of participants were in 90-180 min duration in all three groups followed by 0-90 min category. All the three group had a steady decrease in Cuff pressure.
Table 4: Cough: A comparative assessment @ ET, 30 min, 60 min, 12 hour and 24 hour
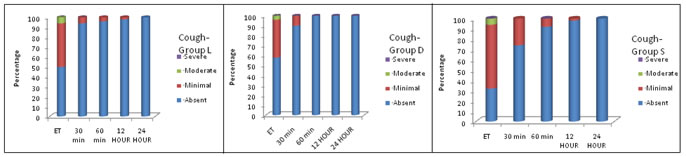
Chi-Square test/Fisher Exact test Figure 1: Cough: A comparative assessment @ ET, 30 min, 60 min, 12 hour and 24 hour In saline group, 34/50 (68%) participants had cough at extubation which significantly reduced to 13 (26%), 4(8%), 1(2%), 0 at 30 min, 60 min, 12 and 24 hr after extubation respectively. This change was statistically significant. In lignocaine group, 25/50 (50%) had cough at extubation which significantly reduced to 3(6%), 2(4%) 1(2%), and 0 at 30 min, 60 min, 12 and 24 hr after extubation respectively. This change was statistically significant. In dexamethasone group 21/50 (42%) had cough at extubation which significantly reduced to 5(10%),0(0%) 0(0%),and 0 at 30 min, 60 min,12 and 24 hr after extubation respectively. This change was statistically significant. This decreasing trend is significantly different in each group. Dexamethasone and lignocaine group seeing steeper decrease (almost to nil). Saline group had significantly higher proportion of cough at all points than lignocaine group and dexamethasone. However, lignocaine group when compared to dexamethasone group had higher proportion of cough only at extubation and 30 min after extubation.
Table 5: Sore Throat: A comparative assessment@ ET, 30 min, 60 min, 12 hour and 24 hour
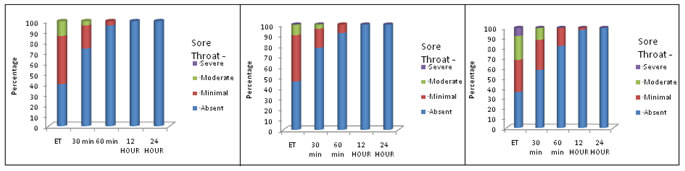
Chi-Square test/Fisher Exact test Figure 2: Sore Throat: A comparative assessment @ ET, 30 min, 60 min, 12 hour and 24 hour In saline group, at extubation severe sore throat was seen in 4 (8%) of patients, moderate in 12 (24%), minimum in 16 (32%) and absent in 18 (36%) of cases. At 30min, it reduced to 0%, 6 (12%), 15 (30%) and 29 (58%) of cases respectively. At 60min, it was 0%, 0%, 9 (18%) and 41 (82%) of cases respectively. This decreasing trend was statistically significant. In lignocaine group, at extubation severe sore throat was seen in 0(0%) of patients, moderate in 7(14%), minimum in 23 (46%) and absent in 20 (40%) of patients. At 30min, it reduced to 0(0%), 2(4%), 11(22%), and absent 37(74%) respectively. At 60min, it was minimum in 2 (4%) of cases. At 24hours, it was seen only in 0% of cases as minimum sore throat. This decreasing soreness and its severity over time were statistically significant. In lignocaine group, there was no one with severe sore throat at any point of time. Moderate sore throat at extubation was seen in 14% and minimal sore throat at extubation was 46% reduced to 22% at 30min and decreased significantly by 24 hr to 0. This decreasing soreness and its severity over time were statistically significant. In dexamethasone group, at extubation severe sore throat was seen in 0 (0%) of patients, moderate in 5 (10%), minimum in 22(44%) and absent in 23(46%) of patients. At 30min, it reduced to 0 (0%), 2(4%), 9(18%), and absent 39 (78%) respectively. At 60min, it was minimum in 4(8%) of cases. At 12 hours and 24 hours, it was seen only in 0% of cases as minimum sore throat. This decreasing soreness and its severity over time were statistically significant. In dexamethasone group also, there was no one with severe sore throat at any point of time. Moderate sore throat at extubation was seen in 5(10%) and minimal sore throat at extubation was 22(44%) reduced to 9(18%) at 30min 4(8%) and decreased significantly by 24 hr to 0. This decreasing soreness and its severity over time were statistically significant. The saline group had significantly higher sore throat score compared to lignocaine group and dexamethasone at extubation. At 30 min after extubation, saline had still higher sore throat score compared to both lignocaine and dexamethasone group. Dexamethasone group had least sore throat. At 60 min after extubation also saline had highest sore throat score, and it was statistically different from lignocaine group and dexamethasone. Lignocaine and dexamethasone groups had significantly lesser sore throat scores than of saline group. The overall trend of sore throat score over time after extubation is significantly different in three groups. Saline group had higher score at beginning and lesser decrease and other two groups had lesser score from beginning and greater decrease to almost nil score by 24 hours.
Table 6: Hoarseness: A comparative assessment @ ET, 30 min, 60 min, 12 hour and 24 hour
Chi-Square test/Fisher Exact test Figure 3: Hoarseness: A comparative assessment @ ET, 30 min, 60 min, 12 hour and 24 hour
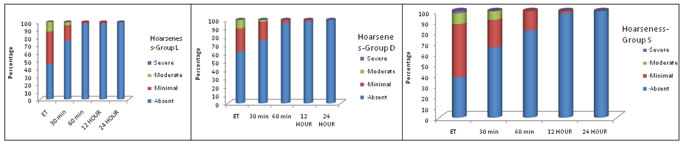
The severe hoarseness of voice was 1 (2%) in saline group and 0 (0%) in lignocaine group and 0 in dexamethasone group at extubation. So, saline group had highest incidence of hoarseness at extubation. Hence, severe hoarseness is more in saline group, at all time and it decreased over time and nil by 24 hours. In saline group, 19 (38%) had no hoarseness at extubation and it increased to 33 (66%), 41 (82%), 49 (98%), 50(100%) at 30 min, 60 min, 12 and 24 hours respectively. This trend was statistically significant. In saline group, hoarseness of all severity decreased over time from extubation to 24 hours. This decreasing hoarseness and its severity over time were statistically significant. In lignocaine group, 23 (46%) had no hoarseness at extubation which was better than saline group, and it increased to 38 (76%), 49 (98%), 49(98%), 50 (100%) at 30 min, 60 min, 12 and 24 hours respectively. This trend was statistically significant. In dexamethasone group 31(62%) had no hoarseness at extubation, which was better than saline group. This increased to 38(76%), 48(96%), 49(98%), 50(100%) by 30 min, 60 min, 12hours and 24 hour respectively. Even, in dexamethasone group severe hoarseness was nil at extubation itself. Thus, dexamethasone group had best hoarseness of voice profile at extubation. This decreasing hoarseness and its severity over time were statistically significant. The normal saline group had significantly higher hoarseness score followed by lignocaine group and dexamethasone group at extubation. This decrement was statistically significant. At 30 min, after extubation, saline had still higher hoarseness score compared to both dexamethasone and lignocaine group. However, there was no significant difference between dexamethasone and lignocaine at this point. At 60 min, after extubation also saline group had highest score for hoarseness of voice, followed by lignocaine and dexamethasone group. The overall trend of hoarseness score over time after extubation is significantly different in three groups. Normal saline group had higher score at beginning and lesser decrease and other two groups had lesser score from beginning and greater decrease to almost nil score by 24 hours.
Table 7: Change in cuff volume
P<0.001**
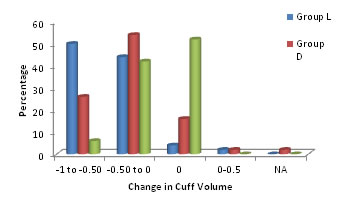
Figure 4: Change in cuff volume There was statistically significant. However, the saline group there was statistically significant decrease in cuff volume by about 0.14 ml. The lignocaine group also witnessed about 0.45 ml decrease which was statistically significant. Similarly, the Dexamethasone group also witnessed about 0.30 ml decrease which was statistically significant.
DISCUSSION Endotracheal tube cuff design, cuff pressure, tube size and tube lubrication are the important factors that affect the incidence of sore throat.1 Most modern tubes are made of polyvinyl chloride. Diffusion of nitrous oxide into the cuff is dependent on the permeability coefficient of the cuff wall and inversely proportional to the thickness of the cuff wall..1,2,3 Estimation of endotracheal tube cuff pressures by can be done by both minimal occlusive volume technique and AMBU cuff pressure gauze to assess the adequacy of intracuff pressure. Change in the cuff volume from intubation to extubation differs depending on the inflating agent used. Although the exact pathophysiology of post intubation airway symptoms is not fully elucidated, mucosal damage occurring at the cuff level is thought to be an important causative factor for tracheal morbidity. Decrease in tracheal mucosal perfusion occurs when the cuff exerts pressure greater than 30 cm H2O.7 Lignocaine has been shown to diffuse across the cuff of an endotracheal tube made of PVC, a largely hydrophobic chemical substance. It can act as a potential reservoir for local anaesthetic allowing diffusion and subsequent anaesthesia of the underlying mucosa. This not only reduces the incidence of sore throat but also enables improved ETT tolerance and helps in producing smooth extubation. Intracuff lignocaine prevents a significant rise in the cuff pressure during N2O anesthesia, secondary to continuous drug diffusion. This balance maintains adequate cuff pressure and protects the airway against air leak or aspiration of gastric content. The principal effect of the use of saline is to keep endotracheal cuff pressure low during the course of an operative procedure by the prevention of inward diffusion of nitrous oxide. On the other hand dexamethasone a potent corticosteroid by controlling the biosynthesis of potent mediators of inflammation such as prostaglandins and leukotrienes thereby decreasing edema and inflammation. In this study, it could be possible that dexamethasone diffused through the ETT cuff, acting on the tracheal mucosa in contact with it, thus reducing the inflammatory process occurring in the tracheal mucosa. Measurement and detection of dexamethasone levels in venous blood samples of patients who had their ETTs inflated with dexamethasone might have confirmed this. Overinflation of cuff pressure can exert too much pressure against the trachea and obstruct mucosal blood flow leading to ischemic complications and damage to tracheal wall. But, the pressure varies with nitrous oxide anaesthesia. So, the study was taken up to compare the cuff pressures and to evaluate and reduce postoperative problems associated with filling the endotracheal tube cuff with saline, lignocaine and dexamethasone.
Table 8: Results of the present study
CONCLUSIONS From the present study it can be concluded that,
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home