Official Journals By StatPerson Publication
|
Table of Content - Volume 7 Issue 3 -September 2018
A comparative study of spinal anaesthesia with 0.5% bupivacaine and 0.75% ropivacaine for percutaneous nephrolithotomy surgeries
Saif Ahmed1, Shilpa Gaikwad2*, Jyotsna Paranjpe3
1Sr.Resident,2Associate Professor,2Professor, Department of Anaesthesiology, Bharti Vidyapeeth Medical College and Hospital, Sangli, Maharashtra, INDIA. Email: sunshineshilpa@gmail.com
Abstract This prospective comparative study was conducted to study and compare the intraoperative anaesthesia and postoperative analgesia between 0.5% Bupivacaine and 0.75% Ropivacainefor spinal anaesthesia for percutaneous Nephrolothtomy surgeries (PCNL).The study was conducted in 80 patients with 40 patients in each group.Group B received sinal anaesthesia with 3-3.5 ml of 0.5% Bupivacaine and group R received spinal anaeshesia with 0.75%Ropivacaine 3-3.5 ml..Onset and duration of motor and sensory blockade was studied and compared. Postoperative analgesia was compared in both groups. Haemodynmic stability was also studied andcompared in both groups Key Words: PCNL, bupivacine, ropivacaine, sensory blockde, motor blockade, haemodynamic stability.
Percutaneous nephrolithotomy (PCNL) is the treatment of choice for large kidney and pelvic stones, staghorn calculus, multiple stones and those resistant to extracorporal shockwave lithotripsy. Advantages of spinal anesthesia are well established and widely accepted over general anaesthesia. such as low pulmonary complications, Various intrathecal additives have been used for PCNL surgeries which include fentanyl and dexmedetomidine withe bupivacaine to provide complete and satisfactory anaesthesia and postoperative analgesia. Hyperbaric Bupivacaine, an amide local anesthetic, is most commonly used for spinal anesthesia. It has high potency, long duration of action. Hyperbaric solutions of local anaesthetics in moderate doses provide mid thoracic spinal blockade which in turn is another cause of hypotension and bradycardia. Prolonged motor blockade with intrathecal hyperbaric Bupivacaine produces more discomfort and undesirable urinary retention. Isobaric solutions of local anesthetics such as Ropivacaine provides low thoracic and lumbar spinal blockade appropriate for PCNL. Ropivacaine, a amide local anaesthetic agent with more haemodynamic stability. The present study was undertaken to compare spinal anaesthesia with intrathecal isobaric Ropivacaine 0.75% and hyperbaric Bupivacaine 0.5% in percutaneous nephrolithotomy surgeries. We aimed our study to evaluate the effectiveness of Ropivacaine 0.75% and Bupivacaine 0.5% for intaoperative Anaesthesia and Postoperative Analgesia when used in spinal anaesthesia for Percutaneous Nephrolithotomy surgeries in patients of Bharati Vidyapeeth University Medical College and Hospital, Sangli with following objectives:
MATERIALS AND METHODS This prospective, randomised, comparative, double blind study was conducted after obtaining Institutional Ethical committee of our institution approval in 80 adult patients aged between 25-60 years undergoing elective PCNL surgeries under spinal anaesthesia. Clearance from Ethical Committee of Institution was obtained. Sample size was decided by statistician All patients were evaluated preoperatively and investigations including haemoglobin, complete blood count, BUN, serum creatinine, blood sugar, serum electrolytes-sodium and potassium, prostate gland size were noted. E.C.G findings recorded. Patients were also explained about Visual Analogue Scale (VAS) score and were taught how to express the degree of pain on the scale. Inclusion Criteria
Exclusion Criteria
1. Those with bleeding disorders and local sepsis. 2. Those on anticoagulant and antiplatelet agent. 3. Those allergic to amide anaesthetics. Statistical Analysis: The data collected in this study was analyzed by using Ms-Excel and Statistical Package for social sciences (SPSS) – version 22-(USA). Proportions and percentage for qualitative characters and Chi-square or Z test, ANOVA were applied for quantitative type of data wherever necessary. OBSERVATION AND RESULTS In this study groups the average age was 48.3 years in Group B and 53.6 years in Group R. Average weight was 60.92 killograms (kgs) in Group B and 62.3 kg in Group R. Average height of patients was 165.02 centimeters (cms) in Group B and 164.65 cms in Group R. The difference in age, height and weight was not statistically significant. Table 1: Mean demographic data in Ropivacaine and Bupivacaine Groups
Comparison of ASA grading between Ropivacaine and Bupivacaine: In this study in Group B 92.5 % ASA grade I patients, 7.5 % ASA grade II patients and in Group R 90 % ASA grade I patients, 10 % ASA grade II patients. There was no statistical significant difference among both groups.
Figure 1: Mean duration of surgery was (96.125±1.39 min) in Ropivacaine group and (97.1 ± 15.98 min) in Bupivacaine group. There was no significant difference in mean duration of surgery between two groups (P = 0.720).
Table 2: Comparison of duration of surgery (Minutes)
Table 3: Comparison of heart rate of patients in Bupivacaine and Ropivacaine groups
Preop Heart Rate - Group B = 89.97± 5.39 Group R =88.5±6.30 T= Time in minutes.
Table 4: Comparison of systolic blood pressure of patients in Bupivacaine and Ropivacaine groups
Preop Systolic BP- Group B = 132.5±5.57 Group R =132.15±3.79
Table 5: Comparison of diastolic blood pressure of patients in Bupivacaine and Ropivacaine groups
T = Time in minutes Preop diastolicBP- Group B= 91.5±4.40 Group R=90.95±3.50. The above table reveal that the mean diastolic blood pressure among Group B and Group R at 120 minutes show statistically significant difference. Table 6: Comparison of motor blockade, sensory blockade and time of onset of pain in Bupivacaine and Ropivacaine groups
*: Highly Significant
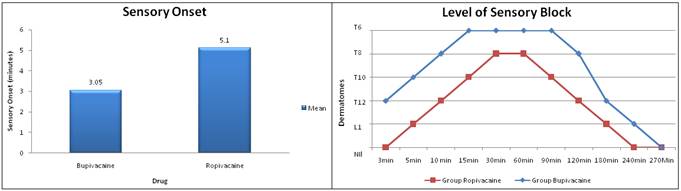
In this study the mean onset time of sensory blockade in Group B was (3.05 minutes) which was significantly low as compared to (5.1 minutes) in Group R. Onset of sensory block was assessed by asking whether patient has started feeling tingling sensation in lower limbs.The mean onset time of motor blockade was (6.1 minutes) in Group B which was significantly low as compared to (7.125 minutes) in Group R. In this study the mean time duration for motor blockade was (159.425 minutes) in Group R which was significantly low as compared (209.725 minutes) Group B.
Figure 2 Figure 3
Sensory blockade was assessed by pin prick method at 3, 5, 10, 15, 30, 60, 90, 120, 180, 240 and 270 mins interval in group B and group R.Group B showed highest sensory blockade level T6 at 15 min which was persistent for 90 mins after which it started regressing down. At120 mins we found two segment regression upto T8. Group R showed highest sensory blockade level T8 at 30 minswhich was persistent for 60 mins after which it started regressing down. At 90 mins we found sensory blockade regressed at T10 level.
Table 7: Comparison of postoperative analgesia by visual analogue scale (VAS) score
In group B 31 patients had mild VAS score whereas 9 patients had moderate VAS score.In group R mild VAS score was found 16 patients whereas moderate VAS score was found in 24 patients in group R.
Table 8: Comparison of duration of analgesia in Bupivacaine and Ropivacaine groups
Unpaired t test: 21.61 In our study mean duration of analgesia in group B was higher (272 + 3.84 minutes) as compared to group R (254.1 + 3.55 minutes).
Table 9: Comparison of side effects between Bupivacaine and Ropivacaine groups
Hypotension was observed in 15 patients in Bupivacaine group and 10 patients in Ropivacaine group.Cases of hypotension in Bupivacaine group (60%) are significantly more than in Ropivacaine group (40%) [P = 0.031]. Shivering was observed in 18 patients in Bupivacaine group and 23 patients in Ropivacaine group. It was statistically significant. Significant Bradycardia (<20%) was not observed in both the groups. Since all patients were premedicated with injection Ondansetron 4mg IV side effects like nausea, vomiting were not observed in both groups. Urinary retention was no detected as all patients were catheterized during the procedure. DISCUSSION Percutaneous Nephrolithotomy is a minimally invasive, effective and safe modality for removal of renal and upper ureteric calculi. Percutaneous Nephrolithotomy is used for the fragmentation and removal of large or multiple calculi from the renal pelvis and renal caliceal systems.PCNL under spinal anaesthesia has the advantage of shorter operative time, shorter hospital stay, earlier return to work, better postoperative pain relief, fewer episodes of nausea and vomiting, more benign postoperative recovery, avoidance of poly pharmacy as well as being cost effective. Our study was conducted on 80 patients undergoing PCNL under spinal anaesthesia to study and compare Ropivacaine 0.75% and Bupivacaine 0.5% in terms of motor and sensory blockade, hemodynamic stablity. We also studied operative anaesthesia and post op analgesia.Bupivacaine is a long acting local anaesthetic. It has high potency, long duration of action and is relatively more cardiotoxic when used in high concentration or when accidentally administered intravascularly. Ropivacaine is a long acting local anaesthetic that is structurally related to Bupivacaine. Ropivacaine is a pure S (-) enantiomer, developed for the purpose of reducing potential toxicity and improving relative sensory and motor block profiles.Ropivacaine is 4 to 5 times less lipophilic than Bupivacaine and this together with its stereo selective properties causes Ropivacaine to have a significantly higher threshold for cardio toxicity and CNS toxicity. Ropivacaine was developed as pure S (-) type of enantiomer and demonstrated to have altered affinity for different ion channels of sodium, potassium and calcium.In our study the demographic characteristics of the patients in the group B (Bupivacaine 0.5%) and group R (Ropivacaine 0.75%)were comparable with respect to age, weight, height, gender and ASA grade.We found that onset time of sensory blockade was faster (3.05±0.552 min) in group B while it was (5.1±1.58 min) in group R. The difference was statistically significant (P value<0.001) and onset of sensory block was significantly delayed with the isobaric 0.75% Ropivacaine as compared to 0.5% hyperbaric Bupivacaine. P.D.W.Fettes et al76 compared plain and hyperbaric solutions of Ropivacaine 0.5% for spinal anesthesia and found that the median time to onset of sensory block at T10 with hyperbaric Ropivacaine was (5 min) and with isobaric Ropivacaine was (10 min), which is statistically significant (p<0.01) which was similar with our study. This was explained as the increase in density of Ropivacaine produced by the addition of glucose would appear to result in a more even distribution, rapid spread of the drug along with the gravity presumably gravity encouraging spread of the bolus of drug down the slopes of the lumbar curve when the patient is placed supine after injection.The study conducted by B.Whiteside, D.Burke, J.A.Wildsmith et al(77)and V.R.R.Chari et al(78) to compare Ropivacaine and Bupivacaine in lower limb surgery found that sensory onset was significantly delayed in the Ropivacaine group (42.6±11.39 min) compared to Bupivacaine group (18.4±6.53 min) which was in accordance with our study. In our study we found that the onset time of motor blockade in group B was (6.1±1.29 min) while in group R it was (7.125±1.39 min). The difference was statistically significant (P value<0.001) and we found that onset time of motor blockade was significantly delayed with Ropivacaine 0.75% as compared to Bupivacaine 0.5%. V.R.R.Chari et al78, Surjeet singhet al79,Dharam nanavati et al80found that the time taken for the onset motor blockade was significantly delayed with Ropivacaine (55.4±13.01 min) when compared with Bupivacanie (27.5±8.03 mins) This result was in similar with our study.In our study sensory blockade regressed from T6 to L1 level within 4 hours in group B where as in group R sensory blockade regressed from T8 to L1 level at 3 hours.Gautier PE et al81Surjeet singh et al79 found that mean duration of sensory blockade was significantly shorter with isobaric Ropivacaine 0.75% than hyperbaric Bupivacaine 0.5%. duration of sensory blockade was (191.38 ±3.562 minutes) in Group B and (191.24±3.414 minutes) in Group R.Helena Kallio, Eljas. Veli Snall et al82compared intrathecal Plain Solutions containing Ropivacaine 20 or 15 mg Versus Bupivacaine 10 mg in lower limb surgeries. They found that both ropivacaine 15mg and Bupivacaine 10 mg provided similar duration of sensory blockade. We also observed same results with our study.In our study we found mean duration of analgesia in Group B was (272±3.84 minutes) where as in Group R was (254.1±3.55 minutes). Jack W van Kleef83et al noted median analgesia time of (358 minutes) with intrathecal isobaric Ropivacaine 0.75%. D.A.McNamee et al84noted mean analgesia time of (180 minutes) where he used only 2.5 ml of intrathecal isobaric Ropivacaine 0.75%, where this low dose may be the reason for shorter duration of analgesia.In our study there was statistically significant difference in duration of motor blockade between two groups. Mean duration time of motor blockade in Bupivacaine group was (209.725±2.01 minutes) which was significantly higher as compared to (159.425±1.95 minutes) in Ropivacaine group. V.R.R.chari et al78concluded duration of motor blockade was significantly prolonged in Bupivacaine group (190.2 ± 28.37 minutes) compared to Ropivacaine group (149.7 ± 8.60 minutes) which was in similar to our study.Helena Kallio, Eljas Veli Snallet al82,Sanchez et al85concluded that Ropivacaine provides significantly faster motor recovery as compared to Bupivacaine which was comparable to our study. The mean time duration for motor block was (121.04 minutes) in Group R which was significantly low as compared (189.92 minutes) Group B.Michela Camorica, Giorgio Capogna et al86studiedthe relative potencies for motor block after intrathecal Ropivacaine, Levobupivacaine and Bupivacaine. They found that intrathecal Ropivacaine and Levobupivacaine are significantly less potent than Bupivacaine, which may explain the lesser motor blocking effects of intrathecal Ropivacaine and Levobupivacaine.Mantouvalou et al87 compared the anesthetic efficacy and safety of three local anesthetic agents: racemic Bupivacaine and its two isomers; Ropivacaine and levobupivacaine, in patients undergoing lower abdominal surgery. The onset of motor block was significantly faster in Bupivacaine group than in Ropivacaine group and almost same of that in levobupivacaine group (P<0.05). Ropivacaine presented a shorter duration of both motor and sensory block than Bupivacaine and levobupivacaine (P<0.05).The Pka of Bupivacaine and Ropivacaine are identical but Ropivacaine is less lipid soluble, envisaging that Ropivacaine will block αA fiberes more slowly than Bupivacaine. Thus Ropivacaine would cause less motor block than Bupivacaine, which is confirmed in this study. This evidence suggests that there is greater degree of sensory-motor separation when using Ropivacaine.In our study postoperatively we observed that in Ropivacaine group 24 patients and in Bupivacaine group 9 patients had moderate VAS score which was not statistically significant. A.R.Bhure, Prasad et al88comparedintrathecal Bupivacaine with Ropivacaine in twodifferent strengths for quality of anaesthesia and postoperative analgesia in lower abdomen hernia surgery. They concluded that the VAS scores in groups Ropivacaine 0.75% and Bupivacaine 0.5% were comparable. In our study Shivering was observed in 18 patients in Bupivacaine group and in 23 patients in Ropivacaine group. Side effects like bradycardia, nausea, vomiting and urinary retention were not observed.In our study we found that the hemodynamic changes due to subarachnoid block were modest with Ropivacaine group and the sympathetic block was less gradual in Ropivacaine group as compared to Bupivacaine group. We defined hypotension as a decrease of systolic blood pressure of more than 20% of baseline. The hypotension occurred in 10 patients in Ropivacaine group where no vasopressors were required but giving fluid challenge with 100ml of Ringer’s lactate was sufficient. In Bupivacaine group hypotension occurred in 15 patients who responded well to the 1 to 2 doses of Injection Ephedrine 3 mg intravenously with fluid challenge. In our study number of cases of hypotension were significantly more in Bupivacaine group {15 (60%)} than in Ropivacaine group {10 (40%)}. The systolic blood pressure showed statistically significant difference at 30 minutes (P value= 0.007) where as diastolic blood pressure showed statistically significant difference in both the groups at 120 minutes (P value=0.006). Surjeet Singh et al79, Whiteside et al77, V.R.R.chari et al(78) also found that incidence of hypotension was more frequent in Bupivacaine group 14 patients when compared with 6 patients of Ropivacaine which was similar to our study Mehta, V.Gupta, R.Wakhloo et al(89) compared intrathecal administration of isobaric Bupivacaine 15mg and Ropivacaine 15mg undergoing lower limb surgery. They found that, there was slight decrease in mean heart rate and arterial blood pressure over 30 minutes after anesthesia which was statistically non significant.Surjeet Singh et al79(2012) compared the intrathecal efficacy and safety of 0.75% isobaric Ropivacaine for caesarean delivery with 0.5% heavy Bupivacaine in 46 parturients of ASA grade I and II. The parturients were randomized to receive either 12.5 mg of 0.5% hyperbaric Bupivacaine or 24 mg of 0.75% isobaric Ropivacaine intrathecally.. Baseline demographic variables were similar in the 2 groups (p value>0.05). The time to achieve sensory block to T10 (3.2±1.5 vs. 2.5±1.3 minutes) or to the maximal level (9.8±3.1 vs. 7.9±2.3 minutes) was longer in the Ropivacaine group (p value = 0.048) but the median maximal level of sensory block was similar between the two groups (p value >0.05).Duration of sensory block was shorter in the Ropivacaine group {(160.5±22.2 vs. 182.3±30.5 minutes) (p value = 0.03)}. Duration of motor block was also significantly shorter than Bupivacaine group {(112.5±45 vs. 165.3±26) (p value 0.004)}.This study conclude that spinal anaesthesia for elective caesarean delivery with intrathecal 24 mg of 0.75% isobaric Ropivacaine provided clinically effective surgical anaesthesia of shorter duration without compromising neonatal outcome and can be used as an effective and safe alternative to BupivacaineV.R.R.Chari et al78 (2013) compared intrathecal efficacy of isobaric Ropivacaine 0.75% with hyperbaric Bupivacaine 0.5% in lower abdominal and lower limb surgeries. They found that sensory and motor onset was delayed in Ropivacaine group than Bupivacaine group. Duration of motor blockade was significantly prolonged in the Bupivacaine group than Ropivacaine group. Duration of postoperative analgesia was similar in both the groups. This study concluded that Ropivacaine might be superior to Bupivacaine in terms of longer sensory block and shorter motor block duration. Therefore 0.75% isobaric Ropivacaine can be safely used in lower limb and lower abdominal surgeries especially in cases where early ambulation is desired.In our study mean duration of analgesia was (272±3.84 mins) in group B where as in group R it was (254.1±3.55 mins).A. R. Bhure, Prasad Ingley et al88(2014) compared intrathecal hyperbaric Bupivacaine with Clonidine, Fentanyl and Midazolam for quality of anaesthesia and duration of postoperative pain relief in patients undergoing elective caesarean section clinical efficacy and safety of intrathecal isobaric Ropivacaine in two different strengths 0.75% with Hyperbaric 0.5% Bupivacaine. 90 patients scheduled for elective lower abdomen hernia surgery were randomly divided into 3 groups of 30 each to receive 3.4 ml of isobaric Ropivacaine 0.5% and 0.75% compared with control group receiving 3.4ml Hyperbaric 0.5% Bupivacaine. The onset of surgical anaesthesia at L1 was delayed with both the Ropivacaine groups compared to Bupivacaine group. Total duration of analgesia was comparable in Bupivacaine and Ropivacaine 0.75% groups. Total duration of motor block was much longer with Bupivacaine group than Ropivacaine groups. So they concluded intratheacal Ropivacaine 0.75% was found to be a good alternative to 0.5% Hyperbaric Bupivacaine in terms of less hemodynamic changes, faster regression of both motor and sensory block and early mobilization of patient. The patient can be mobilized more quickly, as in patients of daycare surgery. In this p study the onset of surgical anaesthesia at L1 was early in Clonidine group as compared to Fentanyl, Midazolam and Control groups (p compared to Fentanyl, Midazolam and Control groups (p The duration of analgesia with Fentanyl was (284.66 minutes) 12.5µg Fentanyl produced analgesia that lasted for (248 ± 11 minutes) and duration of analgesia with 25µg Fentanyl was noted to last for (305 ± 89 minutes). The duration of analgesia with Midazolam was (270.54 ± 36.22 minutes) in this study. However, in a study with intrathecal lignocaine and 2 mg Midazolam in LSCS patients, analgesia lasted for (196.5 ± 3.3 minutes).Dharam S. Nanavati et al80(2015) in their study compared Bupivacaine heavy (0.5% ) 3ml with isobaric Ropivacaine (0.75% ) 3ml, intrathecally in patients posted for lower abdominal and lower limb surgery for sensory and motor effects and hemodynamic stability. 100 patients aged 12 years or older (ASA grade I, II, III) scheduled for various lower abdominal and lower limb surgeries were randomly distributed in two groups. In group B (n= 50) 15mg of hyperbaric Bupivacaine (0.5%, 3ml) and in group R (n=50) 21.5 mg of isobaric Ropivacaine (0.75%, 3ml) was given intrathecally. Onset of sensory block which was 2 minutes (range2-5 min) in ropivacaine group and 2 min (range 2-9 min) in bupivacaine group. Administration of 0.75% isobaric Ropivacaine intrathecally was found to have shorter duration of motor blockade and similar duration of analgesia as compared to Bupivacaine with hemodynamic stability and without significant side effects.One of the reasons to use intrathecal ropivacaine and to replace lidocaine, especially for ambulatory spinal anesthesia, is that, at equal doses, it has a shorter duration of action than Bupivacaine. Neurotoxic effects have been associated with intrathecal lidocaine, prompting the research of alternatives to lidocaine, especially for ambulatory anesthesia. The use of intrathecal ropivacaine was suggested because it does not affect the spinal cord blood flow90and does not induce neurotoxic effects after intrathecal administration in dogs91and rabbits.92
CONCLUSIONSFrom our study we conclude, Both Bupivacaine and Ropivacaine given intrathecally, produce satisfactory anaesthesia for Percutaneous nephrolithotomy surgeries.Spinal anaesthesia with 0.5% hyperbaric Bupivacaine was more prolonged than 0.75% isobaric Ropivacaine.Intrathecal Ropivacaine 0.75% provides more hemodynamic stability than intrathecal Bupivacaine 0.5%.Bupivacaine provides prolonged duration of analgesia than RopivacaineSo, Ropivacaine can be a useful choice of spinal anaesthetic in percutaneous nephrolithotomy surgery, though Bupivacaine provides prolonged post op analgesia in ASA grade I and II patients posted for elective PCNL surgeries.
REFRENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home