Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 2 - November 2018
A prospective study on role of melatonin in attenuation of haemodynamic responses to laryngoscopy intubation and extubation
Adithi Devi E1, W R Pathanjali Rao2*, Pavani Kalyanam3
1Assistant Professor, 2Associate Professor, 3Professor, Department of Anesthesiology, Osmania Medical College, Hyderabad, Telangana, INDIA. Email: drpathanjalirao@gmail.com Abstract Background: Endotracheal intubation is translaryngeal placement of Endotracheal tube into the trachea. Laryngoscopy and tracheal intubation are commonly accompanied by increasing arterial BP and HR. Complications that might arise are acute LVF, dysrhythmias, IC haemorrhage, pulmonary oedema, or MI. Pressor response is exaggerated in hypertensive patients even though rendered normotensive preoperatively by anti hypertensive medication. Aims: Aim of the study is to compare the effect of Melatonin with Placebo in attenuating Haemodynamic responses during laryngoscopy and endotracheal intubation. It also aims to observe whether melatonin helps in maintaining stable hemodynamics intraoperatively and in attenuating extubation response. Materials and methods: It is a prospective randomized control study conducted in Osmania general hospital and in Govt. ENT hospital from Nov2016 to Nov2017.The study was conducted on 60 patients. They were divided into two groups. Group M, who received capsule melatonin 6 mg, Group C who received placebo (Vitamin D3) 120 minutes before surgery. Results: The increase in HR during laryngoscopy and intubation was significantly less in melatonin group compared to control. (P0.0029). Variation in heart rate during extubation, and post extubation was also very significantly less in melatonin group than placebo. Systolic BP was significantly less in melatonin group after the induction, during laryngoscopy and intubation and all the time during post intubation period till 10 minutes. Intraoperatively, systolic BP was significantly less in melatonin group. There was extremely significant decrease in SBP in melatonin group during extubation and post extubation period compared to placebo.
Diastolic BP was less in melatonin group compared to placebo during laryngoscopy and intubation and at 1 minute, 5 minutes and at 10 minutes after intubation. Intra op DBP was significantly less in melatonin group. During extubation and post extubation period, also DBP was significantly less in melatonin group. MAP during intraoperative period was also significantly less in melatonin group. During extubation, and post extubation period, there was an extremely significant difference in both the groups. Conclusion: The study concludes that exogenously administered melatonin 6mg orally 120mnts prior to intubation helps in attenuation of haemodynamic responses to laryngoscopy, intubation and extubation. It also helps in maintaining a stable hemodynamics intraoperatively. INTRODUCTION Endotracheal intubation is translaryngeal placement of Endotracheal tube into the trachea. Laryngoscopy and tracheal intubation are commonly accompanied by increasing arterial BP and HR. The magnitude of haemodynamic changes observed may be dependent on various factors such as depth of anaesthesia, measures taken prior to airway manipulation, the anaesthetic agent used, duration of laryngoscopy and intubation. The principle mechanism in hypertension and tachycardia is sympathetic response which may be the result of increase in catecholamine activity.1A majority of patients presented with reflex tachycardia and hypertension well before the act of intubation which was often enhanced by intubation. Increase in heart rate and BP is transient, variable and unpredictable. The systolic pressure may increase to a mean of +45 mm Hg. It is usually accompanied by pulse rate changes especially sinus tachycardia and even ventricular tachycardia.2Transient hypertension and tachycardia are probably of no consequence in healthy individuals. But either or both may be hazardous to those with hypertension, myocardial insufficiency, cerebral vascular diseases, raised intracranial pressure, or aneurysmal vascular disease. Complications that might arise because of cardiovascular response to laryngoscopy and intubation are acute LVF, dysrhythmias, IC haemorrhage pulmonary oedema, or MI. Pressor response is exaggerated in hypertensive patients even though rendered normotensive preoperatively by antihypertensive medication. Common dysrhythmias are nodal rhythm, atrial and ventricular extrasystoles and pulsusalternans, less commonly, multifocalextrasystoles, pulsus bigeminy and atrial fibrillation. Various strategies have been tried to attenuate this response in high risk individuals. IV anaesthetic induction agents do not adequately or predictably suppress the circulatory response evolved by endotracheal intubation. Additional pharmacological measures like use of volatile anaesthetics, topical and IV lidocaine, opioids like fentanyl, alfentenyl, calcium channel blockers like verapamil, diltiazem, sympatholytics likeclonidine, dexmedetomidine, methyldopa, beta blockers like esmolol, propranolol, benzodiazepine like midazolam, alprazolam, barbiturates, pregabalin, peripheral vasodilators like SNP, NTG etc. have been tried. However, each agent has some limitations such as respiratory depression, hypotension, tachycardia, bradycardia, rebound hypertension or allergic reaction. Hence, there has always been a need for a better agent. Melatonin (N-Acetyl 5 Methoxytryptamine) is an endogenous sleep regulating hormone secreted by pineal gland. It is best known by medical professionals and lay persons for its hypnotic actions. It is also a potent analgesic. It produces no hangover effect and lacks negative effects like addiction, dependence as compared to BZD. It has got anti-inflammatory, antioxidant and antihypertensive effects. Melatonin decreases the dose of IV propofol for induction of anaesthesia. There are only limited number of studies about melatonin as a premedicant in anaesthesia.3 Exogenous administration of melatonin facilitates sleep onset and improves the quality of sleep. It is different from BZD and their derivatives in that it produces natural sleep patterns and does not lead to impairment of cognitive functions. Various researchers have used this drug in different dose patterns as premedication in both adults and children. The mechanism of effect of melatonin on circulation is complex. The blood pressure lowering effect may be attributed to the specific binding of melatonin to melatonin receptorsin blood vessels interfering with vascular response to catecholamines. The present study is undertaken to find the efficacy of oral melatonin in attenuating laryngoscopy, intubation and extubation response and to maintain a stable hemodynamics intraoperatively.
MATERIALS AND METHODS This prospective randomized control study was conducted after obtaining permission from the hospital ethics committee and informed consent from patients. This was done in Osmania general hospital and in Govt. ENT hospital, under Osmania Medical college. The study was conducted from Nov. 2016 to Nov. 2017.The study was conducted on 60 patients belonging to ASA grade I and II aged in between 20 and 45 years including either gender, scheduled for elective surgical procedures under general anaesthesia. This study was conducted in patients who had undergone ENT, Head and Neck, procedures like hyroidectomy, Mastoid exploration, FESS, Urology procedures like PCNL, Neurosurgical procedures like Laminectomy etc. Inclusion Criteria: ASA physical status Grade I and II, Age: 20-45 Years Male or Female, Weight of 40-65 Kg, Surgery requiring general anaesthesia for a duration of 2Hrs or more. Exclusion criteria: Diabetes, Hypertension, Psychiatric illness, Intake of anti psychotics, sedatives, anxiolytics, antiepileptics, Sleep disorder, Obesity, Drug Allergy, Anticipated difficult intubation, Intubation requiring more than one attempt or more than 20 seconds for laryngoscopy, Pregnancy, Lactation and ECG abnormalities All patients were assessed clinically. Presence of any medical disorder and history of drug intake were ruled out. Patients with history of chest pain, palpitation, syncope, history of respiratory, liver or renal problems were excluded from the study. Airway assessments were done to exclude any difficult intubation. All patients underwent the following investigations namely complete blood picture, RBS, CUE, LFT, RFT, Serum Electrolytes, Chest X-ray and ECG. Procedure was explained to the patients and written informed consent was taken. The patients were randomly allocated into two groups. Group M and Group C received 6 mg melatonin (2 capsules) and placebo (2 capsules of vitamin D3) respectively 120 minutes before surgery. There were 30 patients in each group. The study drugs were administered in the preoperative room with sips of water120 minute before surgery. Continuous monitoring of PR, RR, BP, and arterial oxygen saturation (SpO2) was done in preoperative period in preoperative room. On receiving the patient in the operation theatre, routine monitoring was commenced which included HR, ECG, Arterial SpO2 and NIBP. Crystalloid infusion was started with 18 Gauge IV cannula. The premedication, induction agent, and muscle relaxant to facilitate intubation were standardized for both the groups. Injection glycopyrrolate 0.004 mg/Kg, injection ondansetron 0.08 mg/Kg and fentanyl 1 μg/Kg were administered intravenously. All patients were administered 100 % oxygen for 3 minutes before induction. Induction was obtained with Inj propofol 2 mg/Kg IV. Preservative free lignocaine 2% 3cc was given IV before propofol injection. Succinylcholine was given 2mg/Kg IV to facilitate endotracheal intubation with proper sized cuffed ETT tubes with the aid of Macintosh laryngoscopic blade by same person each time. Maintenance of anaesthesia was obtained with Sevoflurane 1 MAC, withN2O: O2 = 3:2. Muscle relaxation was achieved with Vecuronium bromide administered in the dose of 0.06 to 0.08 mg/KG IV as loading dose and one fourth of initial dose as maintenance dose. Mechanical ventilation was adjusted to maintain normocapnia (ETCO 2 value of 35-38 mmHg). Surgery was not allowed to commence till the 10 minutes after intubation as some of the surgeries required change in position of the patients. IV administration of injection Ketorolac 60 mg was given slow IV intraoperatively. Injection fentanyl 1 microgram/Kg IV was given after 10mins of intubation intraoperatively. After completion of surgery, Inj Neostigmine 50 μg/Kg and injection glycopyrrolate 10 μg/Kg were administered IV to reverse the residual neuromuscular blockade. Haemodynamic parameters were recorded using Philips Sure Signs Vm8 monitor. Heart rate, Systolic BP, Diastolic BP and Mean Arterial BP were recorded preoperative(Baseline), 120 minutes after the study drug, Just after induction, During laryngoscopy and intubation,1,2,3,5,10 mins after intubation, 30, 60, 90, 120 minutes intra operatively, During, 1,3,5 mins after extubation. All the patients were followed up in the postoperative period. Patients received the standard postoperative care, and monitored heart rate, NIBP, respiratory rate and arterial saturation. All patients were observed for any episodes of nausea, vomiting headache, dizziness, respiratory depression, arrhythmias, hypotension and restlessness for 24 Hrs. Statistical data were entered into Microsoft Excel and analysed with the data analysis modules. RESULTS Both the study groups were identical in terms of age, gender distribution, weight, ASA status and duration of surgery. Table-1: Variables
Table 2: Heart rate at various points of time
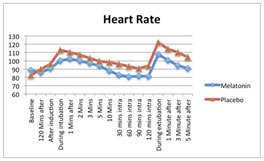
Figure 1: Heart Rate at various point of time P value less than 0.05 implies significant difference between two groups. P value > 0.05 implies no significant difference between two groups. The increase in HR was significantly less in melatonin group compared to place boduring laryngoscopy (P value 0.0029) at 1 min (P value 0.046) and at 10min after intubation (P value 0.0042). HR was significantly less in melatonin group compared to placebo at 30minutes (P < 0.0001), 60 minutes (P 0.0004), 90 minutes (P 0.0069) and120 minutes (P < 0.0001) during intraoperative period. The HR increased during extubation in both melatonin and placebo groups. But the increase in HR was significantly less in melatonin group during extubation (P 0.0013), 1minute after extubation (P 0.0007), 3 minute after extubation (P < 0.0001) and at 5 minute after extubation (P < 0.0001).
Table 3: Systolic Blood Pressure (SBP) at various points of time
The baseline SBP in two groups were comparable without statistical significance (P value 0.1227). The increase in SBP was significantly less inmelatonin group compared to control after induction (P value < 0.0001), during laryngoscopy (P = 0.0134). 1 minute after intubation (P 0.0020), 2minutes after intubation (P 0.0193), 3 minutes after intubation(P 0.0161).5 minutes after intubation (P 0.0104) and 10 minutes after intubation (P< 0.0001). SBP was significantly less in melatonin group compared to placebo uringintra operative period, at 30 minutes (P 0.0017), 60 minutes (P 0.0005), 90 minutes (P 0.0086). SBP increased during extubation in both the groups. But this was significantly less in melatonin group during extubation (P0.0002), 1 minute (P < 0.0001), 2 minutes (P < 0.0001) and 5 minutes (P < 0.0001) post extubation.
Table 4: Diastolic Blood Pressure (DBP) at various points of time
Baseline DBP was comparable without statistical significance (P 0.8892). The increase in DBP was significantly less in melatonin group compared toplacebo at 1 minute after intubation (P 0.0125) at 5 minutes (P 0.0047) and at 10 minutes (P < 0.0001) post intubation. DBP was significantly less in melatonin group compared to placebo at30 minutes (P 0.0098), 60 minutes (P 0.0011), 90 minutes (P 0.0056) and at 120 minutes (0.0277) intraoperatively. Increase in DBP was significantly less in melatonin group during extubation (P 0.0087), 1 minute (P 0.0123), 3 minutes (P 0.0005) and 5 minutes (P < 0.0001) after extubation. Table-5: MAP at various points of time
Figure2: Mean Arterial Pressure at Various Point of tome
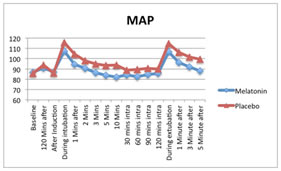
Baseline MAP were comparable among the two groups (P 0.5902). The MAP of control group was higher than the melatonin group throughout. The increase in MAP was significantly less in melatonin group at 1 minute (P0.0241), 5 minutes (P 0.0193) and 10 minutes (P < 0.0001) post intubation. MAP was significantly less in melatonin group at 60 minutes (P 0.0047), 90 minutes (P 0.0227) intraoperatively. The increase inMAP was statistically less in melatonin group during extubation (P 0.0177), 1 minute (P 0.0021), 3 minute (P 0.0019) and 5 minute (P< 0.0001) after extubation. It can be observed that the Placebo group has unstable haemodynamic response during laryngoscopy, intraopperiod, and extubation while melatonin group has stable behaviour.
DISCUSSION The present study is aimed at assessing the role of melatonin in attenuating haemodynamic responses to laryngoscopy and intubation. Stress response under anaesthesia may be in the form of endocrine or autonomic disturbance. The reflex cardiovascular effects in anaesthetised patients include rise in arterial pressures (SBP, DBP, MAP) and heart rate, and they peak approximately30-45 seconds after laryngoscopy. The haemodynamic changes are due to reflex sympathetic discharge caused by epipharyngeal and laryngopharyngealstimulation. The increase in HR and BP are usually transient, variable andunpredictable.1,2 Transient hypertension and tachycardia are probably of no consequence in healthy individuals. But either or both may be hazardous to those with hypertension, myocardial insufficiency and cerebrovascular disease. The peri intubation period is one of the stressful moments of general anaesthesia. These changes are the maximum at one minute after intubation and last for five to ten minutes. Stretching of pharyngeal and laryngeal tissue during laryngoscopy is the major cause of haemodynamic response. Different pharmacological agents were used to attenuate haemodynamic response. Surface anaesthesia of larynx and pharynx with lidocaine spray proved unsuccessful because of the need to perform laryngoscopy with resultant stretching and pressure on tissues of larynx and pharynx. Lidocaine1.5 mg/Kg does not markedly attenuate the stress response. Deep plane of anaesthesia with volatile agents control changes in heart rate and arterial pressure. But it is not useful for rapid sequence intubation, and it may also lead to hypotension and prolonged recovery.3 Vasodilators4 may cause intra operative hypotension and may require invasive arterial pressure monitoring. Other drugs like labetalol, diltiazem, verapamil, nicardipine, opioids like fentanyl, buprenorphine, alpha2agonistdexmedetomidinehave been in use.5 The search for an ideal technique or agents and its proper dosing and timing of administration still continues. Recent studies with melatonin have demonstrated beneficial effects in attenuating the haemodynamic response to intubation. Studies with melatonin in anaesthesia are less. The present study, intends to assess the response of melatonin in intubation response, intra operative haemodynamic stability and extubation response. Problems associated with extubation, recovery and emergence are more common than problems at intubation. Many aspects are controversial with no clear guidelines or protocols. Tracheal extubation is associated with a 10-30 percent increase in arterial pressure and heart rate lasting 5 to 15 minutes. Patients with CAD experience a 40-50 percent decrease in ejection fraction. The response may be attenuated by pharmacological interventions including Injesmolol (up to1.5 mg/Kg IV, 2-5 minutes before extubation), glyceryl trinitrate, magnesium, propofol infusion, remifentanil or alfentanil infusion, IV lidocaine 1 mg/Kg over two minutes, topical lidocaine 10 percent, perioperative oral nimodipine, labetalol, alternatively tracheal intubation can be converted to LMA before extubation. Melatonin is a pineal gland hormone which controls the circadian rhythm. It has been used for sleep disorders, jet lag, perioperative anxiolysis and sedation, without impairment of cognitive and psychomotor function.6 It has got hypnotic and analgesic properties due to inhibitoryaction on CNS. It has sympatholytic action. Perioperative melatonin helps in modification of surgical stress response.7 Previous studies have shown that melatonin could reduce MBP in healthy men and women. All these factors make melatonin an excellent premedicant. It may help in diminishing haemodynamic variation during laryngoscopy and intubation. It may also help in maintaining stable haemodynamics intraoperatively and during extubation. The peak effect of exogenous melatonin ranges from 60-150 minutes.8Based on this melatonin can provide haemodynamic stability during laryngoscopy and intubation when given 120 minutes before the procedure. So it has been decided to give melatonin 6 mg 120 minute before induction of anaesthesia. It has been studied that melatonin reduces mean blood pressure in healthy volunteers. The BP lowering effect may be attributed to the specific binding of melatonin to melatonin receptors in the blood vessels interfering with the vascular response tocatecholamines.9 It may interfere with the peripheral as well as central autonomic system causing a reduction in adrenergic outflow and resulting catecholamine levels. It may induce relaxation of arterial wall smooth muscles by enhancing the availability of NO. It may also act via specific receptors, melatonin type 1 or type 2 located peripherally in the blood vessels and centrally in blood pressure regulating area of brain. It also has free radical scavenging effect leading to dilatation of blood vessels and it may work viaepigenetic mechanism at area postremain the brain. The BP lowering effect could also be due to sedative action of orally administered melatonin. The sedative effect is mainly due to binding at GABA-A receptors and exerting an anaesthetic effect .10 The role of melatonin in anaesthesia and critical care has been elaborately discussed in literature. The use of melatonin for attenuation of haemodynamic responses before laryngoscopy and intubation is superior to few other drugs studied for the same purpose. Dexmedetomidine is associated with significant bradycardia and hypotension. Esmolol has more selective action on HR than BP. As compared to remifentanil, melatonin is easily available and easy to administer. Remifentanil is associated with severe hypotension. Melatonin has hypnotic, anxiolytic and analgesic properties. It has got antioxidant and immune modulatory function. It attenuates surgical stress response and improves surgical outcome. It has got an excellent safety profile. It will not cause hangover effect or drug dependence compared to Benzodiazepines (BZD).11There are limited number of studies which has examined the potential of melatonin in anaesthesia for attenuating haemodynamic responses. This study attempts to further examine melatonin’s potential as a premedicant for the role in the attenuation of haemodynamic response to intubation12inpatients undergoing general anaesthesia. And also to compare the haemodynamic stability and extubation response in the patients. BP stabilizing effect of melatonin can be possibly explained by 1. Sedative, hypnotic, anxiolytic, analgesic effects due to GABAergic system activation. Melatonin administration produces significant dose dependant increase in GABA concentration in CNS. 2. Decreased surgical stress response and catecholamine release due to its sympatholytic activities. 3. BP lowering effect. Melatonin modifies peripheral arterial responsiveness to noradrenaline. It may also influence peripheral as well as central autonomic nervous system causing a reduction in adrenergic responses and catecholamine levels. Melatonin acts via melatonin type 1 or type2 receptors located peripherally in blood vessels and centrally in BP regulating areas of brain. 4. Free radical scavenging effect also helps in vaso dilatation. CONCLUSIONS REFERENCES
|
|
 Home
Home