Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 3 - December 2018
Evaluation of the hemodynamic effect of bupivacaine wound instillation in modified radical mastectomy
Vinutha M1, Rashmi N R2*, VB Gowda3
1,2,3Department of anaesthesiology and pain relief, Kidwai memorial institute of oncology, Bangalore – 560029, Karnataka, INDIA. Email: vinutha881988@gmail.com
Abstract Background and aim: Breast cancer are a leading cause of cancer death among women. Modified Radical Mastectomy (MRM) is the commonest surgery done for operable breast malignancies. Majority of operated patients will experience some degree of postoperative pain. Poorly managed postoperative pain may cause activation of the stress response leading to stress over several major organ. This study has been designed to determine hemodynamic effects of bupivacaine wound instillation for postoperative pain relief in patients undergoing MRM for cancer breast. Methods: In this comparative prospective randomized clinical study 66 patients aged 30–65years were divided into three groups D, S and C. All patients received general anesthesia. Axillary and chest wall drains were placed at the end of surgery. Group D received 40ml of 0.25% bupivacaine 20ml through each drain. Group S received 40ml of normal saline 20ml through each drain. Group C was the control with no installation. After instillation of study drug, the drains were clamped for period of 10mins. After extubation, pain score for pain was evaluated using visual analog scale and then 4thhourly till 24 hrs. Rescue analgesia was injection tramadol, if the VAS ≥4. The patient’s hemodynamic parameters were monitored postoperatively 4th hourly for 24 hrs. Statistical analysis was performed using software SPSS 18.0, and R environment ver.3.2.2. Result: the parameters monitored were pulse rate, mean arterial pressure and SpO2%. The mean of these hemodynamic parameters was calculated and compared with the other groups. It was found to be statistically not significant. Conclusion: The wound instillation of bupivacaine into surgical drain in modified radical mastectomy provides an effective post-operative analgesia with better hemodynamic stability and reduced adverse effect related to the drug and minimal or no complication associated with instillation of the drug. Key Word: Local anaesthesia, bupivacaine, postoperative pain, modified radical mastectomy
INTRODUCTION Most surgical procedures are associated with tissue damage and majority of operated patients will experience some degree of postoperative pain. Poorly managed postoperative pain may have both acute and chronic negative effects and may influence morbidity and mortality.1,3 Transmission of painful stimuli from the periphery to the CNS causes neuroendocrine stress responses, which are characterized by an increased secretion of catabolic hormones including cortisol, catecholamines, adrenocorticotropic hormone, antidiuretic hormone, glucagon, aldosterone, renin and angiotensin II. Furthermore, anabolic mediators such as insulin and testosterone are inhibited.4 Postoperative pain may activate the sympathetic nerve system. This sympathoadrenal stress response may increase myocardial oxygen consumption and decrease myocardial oxygen supply due to coronary vasoconstriction. In addition, gastrointestinal activity may be decreased.2 There are many options available for treating pain after surgery, including systemic analgesia (i.e., opioid and non-opioid drugs), regional analgesic techniques(i.e., neuraxial and peripheral), local anaesthetic wound infiltration and or a combination of these. It is important to assess the risks and benefits of each treatment modality. Infiltration of local anaesthetics (LAs) into surgical wounds is a simple method to provide postoperative analgesia. The basic concept of this technique is to block pain at the origin due to local application of anaesthetics. LAs block voltage-gated sodium channels and consequently the transmission of pain from the surgical wound is reduced or abolished. In addition, the inflammatory response to the injury is suppressed.5
MATERIALS AND METHOD This is a comparative prospective randomized clinical included 66 female patients who underwent modified radical mastectomy for carcinoma breast belonging to ASA grade 1 and 2 and those who fulfilled the inclusion and exclusion criteria and were willing to participate in the study were enrolled for the study. The patients then were randomly allocated to one of the three groups either group D (0.25% bupivacaine), or group S (saline) or group C (control) based on the computer-generated randomization table. Apreanesthetic check-up is done on a day before the surgery and during preanesthetic check-up a detailed clinical history will be taken including and comorbid illness and drug therapy for comorbid illness. a detailed general examination and systemic examination is done and documented. Basic laboratory investigations are revived and documented. All patients were explained regarding the surgical procedure and informed written consent will be obtained from the patients willing to be part of the study. They were familiarized with pain scoring VAS scale. All patients received Tab. Alprazolam 0.5mg and Tab. Ranitidine 150mg the night before surgery and were kept nil per oral 8 hours prior surgery. On day of surgery NPO status was confirmed, routine non-invasive monitors i.e., pulse oximetry, NIBP, ECG, was connected in the operation theatre. Basal vitals were noted. Adequate intravenous access will be secured. Premedication, Induction and maintenance of general anaesthesia was standardized according to hospital protocol. At the end of the surgical procedure, axillary and chest wall drains were placed. Group D received 40ml of 0.25% bupivacaine 20ml through each drain. Group S received 40ml of normal saline 20ml through each drain. Group C was the control with no installation. After instillation of study drug, the drains were clamped for period of 10mins. After extubation, pain score for pain was evaluated using visual analog scale and then 4th hourly till 24 hrs. Rescue analgesia was injection tramadol, if the VAS ≥4.The patient’s hemodynamic parameters were monitored postoperatively 4th hourly for 24 hours. the parameters monitored were pulse rate, mean arterial pressure and SpO2%. The mean of these hemodynamic parameters was calculated and compared with the other groups Statistical analysis was performed using software SPSS 18.0, and R environment ver.3.2.2 OBSERVATION AND RESULT The three groups were compared with respect to demographic data (age, sex, weight), ASA grade, procedure and duration of surgery.
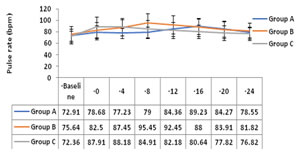
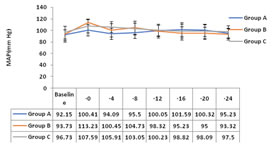
VAS score was significantly lower in group D compared to group S and C (p<0.001). Group D mean VAS score was 3.68±0.65 and 3.59±0.96 during the period of 16th and 20th hour versus 3.27±0.55, 2.59±0.73 and 3.09±075, 2.59±0.50 in group S and C respectively. Group S the mean VAS score was 4.18±0.66 during 8th hour compared to 2.09±0.53 and 3.82 ±0.50 in group D and C respectively. Group C mean VAS score was 4.32±0.72 during 0-hour compared to 2.00±0.69 and 0.77±0.61 in group S and group D respectively. The patient’s hemodynamic parameters were monitored postoperatively for 24 hrs. the parameters monitored were pulse rate, systolic and diastolic blood pressure, mean arterial pressure and SpO2% the mean of these hemodynamic parameters was calculated and compared with the other groups. Group D showed slight increase mean heart rate to 89.23 and 84.27 from the baseline 72.9 during 16th and 20th hour of postoperative period. Group S showed increased in mean heart rate of 95.45 and 92.42 from 75.64 during 8th to 12th hour. Group C with the baseline mean heart rate of 72.36 there was increase to 87.81 and 88.16 during 0 to 4th hour postoperatively. These changes were noticed during onset of pain in the respective groups. It was statistically insignificant. Figure 1: Pulse rate distribution in three groups Figure 2: Mean arterial pressure distribution in three groups
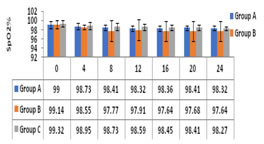
There was no significant difference between the groups with respect to postoperative MAP, SPO2. The three groups had similar MAP, SPO2values throughout the postoperative period. (ANOVA test with Post-Hoc Tukey test, with in group analysis: Student t test).
Figure 3: SpO2 distribution in the three groups DISCUSSION A wound instillation is a method of postoperative analgesia efficient in the various surgical procedures. With the advances in the discovery of the drugs and to the introduction of local anaesthetics with prolonged action, less adverse reactions and considerable analgesic effects, this technique is more frequently used. This method is simple and inexpensive and was developed to reduce opioid consumption, achieve painless recovery period, better patient comfort and to improve patient outcome, with minimal side effects as the spread of local anaesthetic is limited to the surgical wound. Sidiropoulou et al., in his study concluded that continuous wound infiltration of local anaesthetic provided similar postoperative analgesia compared to paravertebral block after mastectomy with axillary dissection, hence it’s an effective alternative to complex procedures like blocks6. In a study conducted by Manaa E et al., in patients who underwent breast augmentation he concluded that local anaesthetic irrigation reduces opioid rescue analgesia requirement and postoperative pain intensity level7. In any patient the maximum dose of bupivacaine injected was 100mg, which is within the recommended maximum safe dose for bupivacaine i.e.,3mg/kg. Nevertheless, we must keep in mind the potential for systemic toxicity in the setting of inadvertent intravenous injection In our study, we noticed there was no statistical significance in the change in the heart rate between the three groups. Though, group D showed slight increase mean pulse rate from the baseline pulse rate of 72.9bpm to 89.23bpm and 84.27bpm during 16th and 20th hour of postoperative period respectively, group S showed increased in mean pulse rate from 75.64bpm to 95.45bpm and 92.42bpm during 8th to 12th hour respectively, whereas in group C with the baseline mean heart rate of 72.36bpm there was increase to 87.81bpm and 88.16bpm during 0 to 4th hour postoperatively. This change in the pulserate was consistent with the increase in VAS score thereby reflecting that this increase in pulse rate was associated with pain and with adequate pain control patients had a better hemodynamic stability. In our study, there was no significant difference between the groups with respect to postoperative MAP. The three groups had similar MAP values throughout the postoperative period. Thus, the hemodynamic stability with respect to MAP was maintained in all groups. There was no significant difference between the groups with respect to postoperative SPO2.
CONCLUSION The wound instillation of bupivacaine into surgical drain in modified radical mastectomy provides an effective post-operative analgesia with better hemodynamic stability and reduced adverse effect related to the drug and minimal or no complication associated with instillation of the drug. Local anaesthetic drugs can be safely used to provide post-operative analgesia provided they are used in correct doses in wound instillation.
REFERENCES
|
|
 Home
Home