Official Journals By StatPerson Publication
|
Table of Content Volume 10 Issue 1 - April 2019
Study of seroprevalence of syphilis from the patients attending tertiary care centre Saurashtra region, Gujarat, India
Hitesh R Ahir1, Parul C Patel2*
1,2Assistant Professor, Department of Microbiology, GMERS Medical College, Junagadh, Gujarat, INDIA. Email: dr_hitesh84@yahoo.com
Abstract Objectives: Main objective of our study is to be detect cases of syphilis from patients attending tertiary care teaching hospital, Saurastra region, Gujarat, India by Standard test for syphilis named Rapid Plasma Reagin Test (RPR). To detect syphilis cases we were used RPR tests for screening antenatal women in a tertiary care hospital from March 2018 till February 2019. Methods: A total of 10485 samples received from various patient groups including prenatal Cases were screened for syphilis by rapid test by RPR based passive agglutination test. All RPR positive sample were confirmed by the TPHA test. Also all positive RPR sample were tested for HIV at the ICTC center. Results: Among the 10485samples collected, 3 were positive by RPR test. Among 3 positive by RPR test were confirmed by Treponema pallidum hemagglutination Assay(TPHA). The cumulative Seroprevalence over one year was found to be 0.028% in pregnant women attending antenatal clinic. Not a single case showed the co infection of HIV and syphilis. Conclusions: The Seroprevalence of syphilis among pregnant women in this hospital in Saurastra region was considerably Lower. Co infection of syphilis and HIV is still not noted in this region. More extensive studies are needed for correlation of HIV and syphilis. Key Word: Syphilis, RPR test, TPHA Test, HIV Co-infection
INTRODUCTION Syphilis is found to be a significant cause of preventable prenatal death in developing countries in which more numbers of women remaining untested and untreated. Syphilis is found worldwide an estimated 12 million cases occurred every year. An estimated average 50% of these pregnancies will end in fetal or prenatal death, low birth weight babies, still births or babies born with congenital syphilis. In United States, syphilis is the third most common among sexually transmitted diseases1. One of the most serious complications of the syphilis with pregnancy is the congenital syphilis, occurs when babies contract syphilis from their mother either through the placenta or when passing through the vagina at birth. The early signs of congenital syphilis generally appear from three to eight weeks after a baby is born. Even though these symptoms develop soon after birth, most cases go unnoticed until late congenital symptoms appear in childhood or adolescence2. According to the Centers for Disease Control and Prevention (CDC), untreated syphilis during pregnancy results in stillbirth or death of the infant in 40% of the cases. The CDC also reports that women who acquired syphilis and were untreated in the four years preceding pregnancy passed it on to their baby in 70% of the cases Infants of pregnant women adequately treated with penicillin during pregnancy have a minimal risk of developing congenital syphilis3. Syphilis infection remains an important STI due to its prevalence, infectiousness, and toll on both infected individuals and health systems. Its importance is exacerbated by the fact that its ulcerative lesions facilitate HIV acquisition; another important aspect of syphilis is its potential vertical transmission4-6. Early diagnosis and treatment of pregnant women who tested positive for syphilis have been shown to be effective in reducing stillbirth, neonatal death and congenital infection by more than 55%7,8 . Importantly, these interventions have been estimated to be highly cost-effective even in low income countries 7. Despite the availability of inexpensive and effective antibiotic therapy, syphilis remains a prevalent disease in developing countries and has re-emerged as a public health threat in developed nations 9. Unprotected sex, blood transfusion, needle sharing and vertical transmission from mother to the child are major modes of syphilis transmission10- 12.
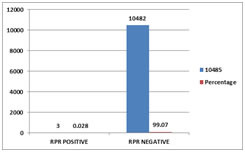
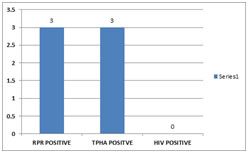
MATERIALS AND METHODS The study was conducted in a tertiary care teaching hospital in Saurastra region, Gujarat, India from March 2018 till February2019. A retrospective analysis of laboratory log book maintained for syphilis tests was used for this purpose. A total of 10485 samples were received from antenatal cases. Screening for syphilis was performed by RPR Rapid plasma reagin (RPR) test. A specific treponemal test, Treponema pallidum hemagglutination assay (TPHA) was performed on samples positive in the quantitative RPR. Samples positive in both tests were designated as seropositive for syphilis. All positive samples by TPHA were screened for HIV testing at ICTC center by rapid test supplied by the GSACS. RESULTS Figure 1: Prevalence of syphilis among study participants. Figure 2: Comparision of RPR, TPHA and HIV According to the figure out of 3 RPR positive sample were positive by confirmatory test by TPHA. And all were negative for the HIV.
DISCUSSION According to the graph and out of 10485 sample 3 (0.028%) were positive for Syphilis and 99.07% were negative for syphilis. As shown in figure 1. Various studies from the different zone showed the following prevalence of syphilis. All RPR positive samples are positive by the confirmatory tests TPHA. none of them showed the co infection with the HIV as shown in figure 2.
CONCLUSION The Seroprevalence of syphilis among pregnant women in this hospital in Saurastra region was considerably Lower. Co infection of syphilis and HIV is still not noted in this region. More extensive studies are needed for correlation of HIV and syphilis.
REFERENCES
|
|
 Home
Home