Official Journals By StatPerson Publication
|
Table of Content Volume 10 Issue 2 - May 2019
Microbiological study of patients with VAP admitted to ICU
Pallavi Priya1, Shailendra Kumar2*, Namrata Kumari3
1Senior Resident, Department of Microbiology, Indira Gandhi Institute of Medical Sciences, (I.G.I.M.S.) Raja Bazar, Patna, INDIA. 2Senior Resident I.G.I.M.S. Patna, INDIA. 3Department of Microbiology, I.G.I.M.S. Patna, INDIA. Email: drshailendra97@gmail.com
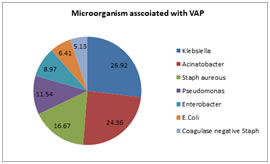
Abstract Background: Ventilator-associated pneumonia (VAP) is a significant cause of morbidity and mortality in critically unwell patients within the intensive care unit (ICU) who undergo invasive mechanical ventilation (MV) via an endotracheal tube (ETT) or tracheostomy. Aims and Objectives: To study Microbiological study of patients with VAP admitted to ICU. Methodology: This was a cross-sectional study carried out in the patients of Ventilator associated Pneumonia (VAP) in the patients admitted to ICU of a tertiary health care centre during the one year period i.e. Oct 2017 to Oct 2018. In the one year period there were 78 confirmed patients of VAP were enrolled to study. The analysis done by excel software for windows 10. Result: The majority of the patients were in the age group of >60 Yrs. were 32.05%, followed by 50-60 Yrs. were 24.36%, 40-50 were 21.79%, 30-40 Yrs. were 15.38%, 20-30 Yrs. were 6.41%. The majority of the patients were Male i.e. 57.69% and Female were 42.31%. The majority of the patients were positive with Microorganism Klebsiella in 26.92%, followed by Acinatobacter in 24.36%, Staph aureous in 16.67%, Pseudomonas in 11.54%, Enterobacter in 8.97%, E. Coli in 6.41%, Coagulase negative Staph in 5.13%. no patients of fungal infections found in our case this difference may be due to different set up or sterilization of hospital environment may differ place to place. Conclusion: It can be concluded from our study that the majority of the patients were in the age group of >60, The majority of the patients were Male and most common organisms isolated were gram negative organism like Klebsiella, Acinatobacter, Staph aureous, Pseudomonas, Enterobacter, E. Coli, Coagulase negative Staph Key Word: VAP (Ventilator associated Pneumonia), Micro-organism of VAP, Intensive care unit (ICU)
INTRODUCTION Ventilator-associated pneumonia (VAP) is a significant cause of morbidity and mortality in critically unwell patients within the intensive care unit (ICU) who undergo invasive mechanical ventilation (MV) via an endotracheal tube (ETT) or tracheostomy. Early diagnosis and adoption of practices known to prevent VAP can reduce mortality and decrease the development of multidrug–resistant organisms.1 VAP is a type of hospital-acquired pneumonia that occurs more than 48 hours after endotracheal intubation. This can be further classified into early onset (within the first 96 hours of MV) and late onset (more than 96 hours after the initiation of MV), which is more commonly attributable to multidrug–resistant pathogens.2 VAP is estimated to occur in 9-27% of all mechanically ventilated patients, with the highest risk being early in the course of hospitalization.3,4 It is the second most common nosocomial infection in the intensive care unit (ICU) and the most common in mechanically ventilated patients.5,6 So we have seen Microbiological study of patients with VAP admitted to ICU
METHODOLOGY This was a cross-sectional study carried out in the patients of Ventilator associated Pneumonia (VAP) in the patients admitted to ICU of a tertiary health care centre during the one year period i.e. Oct 2017 to Oct 2018. In the one year period there were 78 confirmed patients of VAP were enrolled to study. All routine investigations done. All of the patients undergone microbiological investigations by standard procedures of sample collections to staining procedures. The details of the patients like age, sex and identified microorganism was entered to excel sheet and analyzed by excel software for windows 10. RESULT Table 1: Distribution of the patients as per the age
The majority of the patients were in the age group of >60 were 32.05%, followed by 50-60 were 24.36%, 40-50 were 21.79%, 30-40 were 15.38%, 20-30 were 6.41%
Table 2: Distribution of the patients as per the sex
The majority of the patients were Male i.e. 57.69% and Female were 42.31%
Table 3: Distribution of the patents as per the microbiological profile
Figure 1: Distribtion of the patients as per microorganism associated with VAP The majority of the patients were positive with Microorganism Klebsiella in 26.92%, followed by Acinatobacter in 24.36%, Staph aureous in 16.67%, Pseudomonas in 11.54%, Enterobacter in 8.97%, E.Coli in 6.41%, Coagulase negative Staph in 5.13%. DISCUSSION The mortality with VAP is considerably high, varying from 24 to 50% and can reach as high as 76% in some specific settings.7 The etiologic agents widely differ according to the population of patients in an intensive care unit, duration of hospital stay, prior antimicrobial therapy and co-morbid conditions. Despite the advancements in antimicrobial regimes, VAP continues to be an important cause of morbidity and mortality. Inadequate antimicrobial therapy, such as inappropriate antimicrobial coverage, or delayed initiation of antimicrobials has been associated with higher hospital mortality in subjects with hospital acquired pneumonia (HAP) or VAP.8 The key to the development of VAP is the presence of an ETT or tracheostomy, both of which interfere with the normal anatomy and physiology of the respiratory tract, specifically the functional mechanisms involved in clearing secretions (cough and mucociliary action). 12Intubated patients have a reduced level of consciousness that impairs voluntary clearance of secretions, which may then pool in the oropharynx. 11 This leads to the macroaspiration and microaspiration of contaminated oropharyngeal secretions that are rich in harmful pathogens. Normal oral flora start to proliferate and are able to pass along the tracheal tube, forming an antibiotic-resistant biofilm which eventually reaches the lower airways. 12 Critically unwell patients exhibit an impaired ability to mount an immune response to these pathogens, leading to the development of a pneumonia.9,10The presence of additional predisposing factors such as pulmonary oedema in these patients can also accelerate the process 11. Early-onset VAP, occurring within the first four days of MV, is usually caused by antibiotic-sensitive community-acquired bacteria such as Haemophilus and Streptococcus. VAP developing more than 5 days after initiation of MV is usually caused by multidrug–resistant bacteria such as Pseudomonas aeruginosa. 10 In our study we have seen that The majority of the patients were in the age group of >60 were 32.05%, followed by 50-60 were 24.36%, 40-50 were 21.79%, 30-40 were 15.38%, 20-30 were 6.41%. The majority of the patients were Male i.e. 57.69% and Female were 42.31%. The majority of the patients were positive with Microorganism Klebsiella in 26.92%, followed by Acinatobacter in 24.36%, Staph aureous in 16.67%, Pseudomonas in 11.54%, Enterobacter in 8.97%, E.Coli in 6.41%, Coagulase negative Staph in 5.13%. no patients of fungal infections found in our case this difference may be due to different set up or sterilization of hospital environment may differ place to place. These findings are similar to Baby Latha Jampala 13 et al they found it was more common in males compared to females (65.62%) Gram negative organisms were most commonly isolated. Among them Klebsiella, Pseudomonas, Acinetobacter were the commonest organisms. Gram positive bacteria were Staphylococcus aureus, Coagulase negative staphylococci and Pneumococci. In 2% of cases Candida spp were isolated.
CONCLUSION It can be concluded from our study that The majority of the patients were in the age group of >60, The majority of the patients were Male and most common organisms isolated were gram negative organism like Klebsiella, Acinatobacter, Staph aureous, Pseudomonas, Enterobacter, E.Coli, Coagulase negative Staph.
REFERENCES
|
|
 Home
Home