Official Journals By StatPerson Publication
|
Table of Content Volume 10 Issue 3 - June 2019
Mycological profile of chronic suppurative otitis media in a tertiary care hospital
Ganesh M Kale1, Pallavi S Tatte2*, Mayuri P Bhise3, Pramod R Bhise4
{1Professor and Head, Department of ENT} {2Assistant Professor, 4Professor and HOD, Department of Microbiology} Dr. P. D. M. M. College and Hospital, Amravati, Maharashtra-444603, INDIA. 3Consultant Microbiologist, Dr. VMGM College, Solapur, Maharashtra-413003, INDIA. Email: pallavitatte@gmail.com
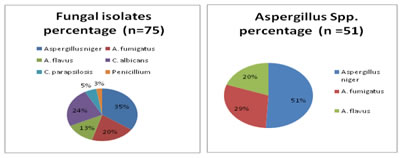
Abstract Background: CSOM is a chronic inflammation of middle ear and mastoid cavity with recurrent ear discharge lasting for more than 6 months. Otomycosis is increasing in recent years because of the indiscriminate use of broad spectrum antibiotics, corticosteroids and an increase in the number of immune deficiency disorders, swimming, use of oils and ear drops. Aims and objectives: The study aimed to find out the fungal agents responsible for causing CSOM among the patients who attended Out Patient Department of ENT in collaboration with Department of Microbiology, Dr. P.D.M.M. College and Hospital, Amravati. Material and Methods: A Total of 130 patients who were clinically diagnosed with CSOM of all age groups and both sexes were selected for study from April 2018 to March 2019. Ear discharge was collected under aseptic precautions using sterile cotton swabs and direct microscopic examination and fungal culture was done. Slide culture done for differentiation of morphology of different species. Results: A total of 130 patients, Fungus isolated from 75 cases. Of which 49 were males and 26 were females. Main fungal isolates were Aspergillus species 51 (68 %), followed by Candida albicans 18 (24 %), Non albicans Candida 4 (5. 33 %), Penicillium 2 (2.66 %). Conclusion: CSOM with Otomycosis produce serious complications and treatment failure. Hence in cases of persistent otorrhoea, aural fullness, otalgia or any symptoms which signifies chronic middle ear infection, then fungal infection should be suspected. If the discharging ear is not responding with antibiotics aural toilet and fungal culture and sensitivity should be done in refractory cases before starting antibiotic therapy. Key Word: Aspergillus niger, Candida albicans, CSOM, Otomycosis,
INTRODUCTION CSOM is an inflammatory condition of the ear that causes recurrent ear discharge through a perforation of the ear drum.1 It frequently requires long term treatment and follow up. Despite this ,there could be recurrences . 2.It is worldwide in distribution with a higher prevalence in the hot, humid and dusty areas of the tropics and subtropics.3,4 Overview of the literature reveals Otitis Media to be a common medical problem in India.5,6 The disease is worldwide in distribution. It is estimated that approximately 5-25% of the total cases of otitis externa are due to Otomycosis.7 This is more prevalent between 2nd and 3rd decades of life among individuals belonging to lower socioeconomic status keeping poor hygiene and malnutrition in children.8,9 Wide spectrum of fungal agents such as Aspergillus spp, Candida albicans, Non Candida albicans, Penicillium being the most common etiological agent.
MATERIALS AND METHODS This study was a prospective study carried out in Department of Microbiology in collaboration with Out Patient Department of ENT, Dr. PDMM College and Hospital, Amravati. Total 130 samples were collected from Out Patient Department of ENT during April 2018-March 2019. Ear discharge was collected under aseptic precautions. The clinical diagnosis was made based on the following symptoms- pruritus, hearing loss, otalgia, ear fullness, otorrhoea, headache and tinnitus. The specimen was then collected using two sterile cotton swabs. One swab was subjected to Microscopic examination by KOH wet mount preparation and the other swab was used for inoculation in Sabouraud’s dextrose agar (two tubes). Fungal growth obtained on SDA were examined for characteristics like rate of growth, colony morphology, colour of obverse and reverse, diffusible pigment production.10 Mycological Investigation:
RESULTS Out of 130 patients, no organism was isolated from 12patients (9.2 %) and bacterial pathogens were isolated in 43 (33.07%) patients. No anaerobes were found in the study. In 75 patients (57.69%), Mycological isolation was positive. The most common fungal isolates belonged to the species of Aspergillus accounting for 51 (68 %) of all fungal isolates. Out of Aspergillus positive samples, A. niger was the most common, followed by A. fumigatus, A. flavus. Species of Candida constituted 29.33% of fungal isolates including Non Candida albicans. Penicillium was 2.66%.
Table 1: Distribution of Fungal isolates from Otomycosis obtained in study
A total of 130 patients with Otomycosis were included in the study. The common symptoms presenting solely or in combination of each other encountered in the study group have been summarized in Table: 2. Otalgia [60%] was the most common complaint encountered followed by pruritis [50%], Ear discharge [27%], hearing impairment [20%], headache [15%] and fullness of ear [11%]. Table 2: Symptomatology of Otomycosis. N = 130
Table 3: Age and sex distribution of the Otomycosis patients (N=75)
A total of 75 patients with Otomycosis were included in the study among them 65.33% were males and 34.67 % were females. The age ranged from 8-70 years. The most prevalent age group was 21-30 age group [40%] followed by 31-40 [20 %] and 41-50 age group [13.33%]. The majority of the patients 52 % showing symptoms of Otomycosis visited the clinic between July to November (i.e. Rainy season ) followed by 33% in summer and minimum 15 % in winter season.
Table 4: Showing the results of of KOH examination and Culture
In the study group, 75/130 (57.69%), samples were both KOH examination and culture positive.
DISCUSSION The present study is to know the fungal etiological agents of Chronic Suppurative Otitis Media. The results are compared and correlated with the studies conducted by other researchers. Otomycoses is frequent in tropical and subtropical climates because of heat and humidity.2,13 Diagnosis of otomycosis is usually made by clinical findings with pruritus being the most common symptom followed by otalgia , ear discharges , Hearing impairment etc.14,15,16 In the present study, presumed diagnosis of Otomycosis was confirmed by laboratory findings in 75/130 (57.69%). The highest isolation rate for Aspergillus spp. was observed i.e. 68% and Candida spp. 29.33% and Penicillium 2.66%.
Table 5: shows studies conducted by other researchers.
Out of 130 CSOM patients, 75 patients with Otomycosis were included in the study among them 49 (65.33%) were males and 26 (34.67%) were females. Studies done by Pradhan et al2 and B. Vishwanatha et al23 reported that Otomycosis is more common in males. In the present study it has been observed that Otomycosis is prevalent in patients with age group between 21-30 yrs followed by 31-40 yrs and 41-50 yrs9,16,17,24 The high incidence can be attributed to the high degree of humidity and heat, the dusty environment and the fact that a large proportion of the population is made up of outdoor labourers and persons of low socioeconomic status.16,24 Otalgia and pruritus were the most common symptom followed by discharge, Hearing impairment, headache and fullness of ear, confirming the findings of earlier studies.2,7,9,16,17,24 The majority of the fungal pathogens isolated from the ear swabs belonged to Aspergillus spp. followed by Candida sp, NAC and Pencillium. Aspergillus spp are common in airborne dust and their heavy growth is added by earwax. Further more the PH level in the normal ear canal is on the acidic side and the common pathogenic Aspergilli experience optimal growth at a PH range of 5 to 7. The pathogenic fungi involved in otomycosis in this agriculturally dominated part of India, are similar to Iran, Turkey and other Mediterranean countries where the majority of the pathogenic fungi involved belonged to Aspergilli. Aspergillus niger was the commonest fungi isolated in our study, in accordance with the other studies.2,7,13,16,17,24 Another study conducted in Microbiology department, Thiruvananthapuram in 2003 showed that among the fungal pathogens causing CSOM, Aspergillus spp. accounts major contribution followed by Candida albicans.25 A study conducted by Dr. Sreekumar in ENT department, in Medical College, Thiruvananthapuram (2007) observed that Aspergillus niger and fumigates are the most common cause of otomycosis.26 In the study conducted by Loy(2002) on patients with CSOM Aspergillus niger, Aspergillus spp. and Candida spp. were main isolates27 Studies by Arya et al., (1966) shows equal distribution of Aspergillus niger and Candida albicans.28 Urmil Mohan and Neerja Jindal in 1998 done a study on fungal and bacterial flora of chronic suppurative Otitis Media in Punjab. They observed that Aspergillus spp. and Candida albicans are the most common fungal isolates causing CSOM.29 Baruah and Agarwal et al., isolated Aspergillus niger, Aspergillus fumigatus, Candida albicans, Candida tropicalis, and Mucor spp. as the causative agents of CSOM.30 Study by Talwar et al.,(1988) on fungal infections of ear with special reference to CSOM observed that Aspergillus niger, Aspergillus fumigatus, Aspergillus flavus, Penicillium, Candida albicans, Candida parapsillosis are the most common fungal pathogens.31 Prevalence of otomycosis during moist and humid conditions has been reported by other study.2 Our study reveals higher incidence in rainy season followed by summer and minimal in winter season. Moist and humid conditions coupled with suitable temperature facilitate fungal growth, are the factors responsible for the higher incidence of otomycosis. Conservative and the medical treatment was the first option for the uncomplicated cases which include topical antibiotics guided by culture and sensitivity and aural toilet.
CONCLUSION Clinical suspicion of otomycosis can prevent unnecessary use of antibiotics and potent steroids for prolonged periods, and presence of moisture leads to otomycosis which might lead to the alteration of the local flora of the ear and leads to the morbidity like hearing loss. Otomycosis is treated by debridment followed with topical azole anti fungals and symptomatically managed with oral antihistamines. Topical 1% clotrimazole drops yielded highest resolution rate with lowest recurrent rate. Aural toilet with the insertion of gauze saturated in Neomycin, Beclomethazone and Clotrimazole for consecutive three days was very effective for CSOM cases due to fungal infection. ACKNOWLEDGEMENT The authours are very grateful to Dr. G.M. Kale, Prof and Head, ENT Department for allowing the collection of samples and Dr. P. R. Bhise, Prof and Head .Department of Microbiology for giving proper guidance for the study.
REFERENCES
|
|
 Home
Home