Official Journals By StatPerson Publication
|
Table of Content Volume 10 Issue 3 - June 2019
Prevalence of subcutaneous mycosis in a tertiary care centre
Emekar Supriya M1, More Sanjaykumar R2*, Rathod Vimal S3, Kandle Suresh K4, Mudholkar Vishal G5,Muddamwar Vijaya G6
{1Assistant Professor, 2Professor & HOD, 3,4Associate Professor,Department of Microbiology} {5,6Assistant Professor,Department of Pathology} Government Medical College, Nanded, Maharashtra, INDIA.
Abstract Background: The incidence of subcutaneous mycosis and associated fungal species varies in different geographic region. It seems to be increasing in some tropical region.Objective:1. To determine the prevalence of infectious etiology (especially fungal) of chronic subcutaneous swellings. 2. To determine prevalence, clinical variation, common etiological agents of subcutaneous mycosis in these patients. Material and methods: In this retrospective study, a total of 3280 patients with chronic subcutaneous swellings(from Jan 2016 to Feb 2017) were screened for infectious and non infectious etiology. Those patients who fulfilled the inclusion criterion were included. The detail data of clinical observations and specific investigations which include fine needle aspiration cytology (FNAC)/Histopathology examination and conventional microbiological culture findings on aspirated/ biopsy material was obtained.Results: A total number of 301/3280 (9.17%) patients had infectious etiology. Out of these, tuberculosis and non tuberculosis etiology were found in 285/301 (94.68%) and 16/301 (5.31%) respectively based on FNAC examination. Among these, fungal infections (14/16) 87.5% and parasitic (02/16) 12.5% were seen. Males with age group of 40 to 80 years were commonly affected. A total of 12/14 (85.71%) lesions were found commonly on extremities .A total of 35.71% samples were culture positive. The fungal species identified were Exophiala jeanselmei (01), Cladosporium cladosporioides species (02), Pheoacremonium species (01), Mucor species (01). Conclusion: The subcutaneous mycosis with no clinical suspicion were found in 14/301 (4.65%) cases which is quite high. It was associated with rare fungal etiology. Key Word: subcutaneous mycosis, phaeohyphomycosis
INTRODUCTION Subcutaneous mycosis is heterogeneous group of chronic infections of dermis and subcutaneous tissue which rarely disseminates.1, 2 It is caused by soil saprophytes of regional epidemiology usually after trauma. It occurs in both immune competent and immune compromised (IC) patients.It is important to understand their epidemiology and clinical presentations to improve their outcomes.3 To the best of our knowledge, very few cases have been reported in literature. Hence we decided to study the occurrence of subcutaneous mycosis and its etiology in this region.
MATERIAL AND METHODS A retrospective study was carried out in the Fine needle aspiration cytology (FNAC) and mycology section of clinical laboratory of our institute for the year Jan 2016 to Feb 2017. The required data (clinical and investigational) of patients was obtained. Inclusion criteria: chronic cutaneous swelling with FNAC findings positive for fungal elements. Exclusion criteria: chronic cutaneous swelling with FNAC findings negative for fungal elements. A total of 3280 patients with chronic subcutaneous swelling were noted for the year Jan 2016 to Feb 2017. Clinical observations and findings of FNAC/ histopathology examination were studied to confirm its infectious and non infectious nature. The fine needle aspiration cytology from lesion can also reveal most of the information about the fungal infection, biopsy may be taken from local site when FNAC fails to reveal any positive findings. If histopathology shows neither fungal elements nor tissue reaction, there is likehood of fungal isolate be merely a contaminent. Therefore, in combination both histopathology and fungal culture provide complete diagnostic lead to any mycotic infection.4The H and E stain is a routine procedure in histopathology laboratory and stains most of the fungi sufficiently to be recognized in tissue section. The specific fungal stains ,such as periodic acid Schiff (PAS), Grocott –Gomori’s methenamine silver stain and Gridley stains are widely used for demonstration of fungi in tissues.4 We have noted down the direct microscopy findings of collected specimen with 20% KOH/ Haematoxylin and Eosin stain (H and E) and Periodic acid Schiff (PAS) stain.A total of 14 patients found positive for fungal elements on FNAC examination were included in the study for which fungal culture done in mycology laboratory. The confirmation of fungal species was done in mycology section. We used Sabouraud dextrose agar with chloramphenicol for isolation of fungi. This media was inoculated and incubated at 25 ̊̊ C and 37 ̊C and was maintained up to 8 weeks for each sample. This was followed by lactophenol cotton blue mount and /or slide culture on corn meal agar to study the detail morphology of the isolated fungus by using standard protocol.4 RESULTS (n=14) Infectious and non infectious nature: Based on FNAC examination (H and E stain), 2979/3280 (90.82%) patients with chronic subcutaneous swellings had etiology as non infectious (benign, malignant and nonspecific inflammatory lesion) and 301 (9.17%) patients had infectious etiology (bacterial, mycobacterial, fungal and parasitic).Among 301 patients, 285 (94.68%) were diagnosed as extra pulmonary tuberculosis based on clinical diagnosis, the findings of FNAC (H and E Stain) and ZN stain. A total of 16/301 (5.31%) were found to have non tuberculous etiology. Among these patients, a fungal and parasitic etiology was found in 14/ 16 (87.5%) and 2/16 (12.5%) samples respectively.
Table 1: Infectious and non-infectious etiology of chronic subcutaneous swelling based on FNAC examination (H and E stain)
Subcutaneous mycosis: The subcutaneous mycoses with no clinical suspicion were found in 14/301 (4.65%) cases which was quite high. The commonest type of swelling was seen on extremities 12/14 (85.71%) and was of soft to firm in consistency. This was followed by cystic swelling and firm to hard with or without sinuses. The majority cases had the findings on local examination as size (2 cm to 10cm), mobile, non tender and well defined. Only 50% patients gave history of injury. a. Age, sex, duration of symptoms: The most patients (78.57%) were between the age group of 40 to 80 years followed by 15 to 40 years. Majority patients were males who were engaged in outdoor activities. Male to female ratio was found as 6:1. The most patients (50%) had duration of symptoms between six months to one year followed by two to six months (28.57%). b. direct microscopy and culture findings: In majority patients, the specimen was aspirated material (purulent/ serous/serosanguinous). The various forms of fungal elements were observed on direct microscopy as septate hyphae, chlamydoconidia (of size 5X 8 um) in chains along the hyphae, yeast like cells, pseudohyphae along with granular necrotic background with degenerative polymorphs, lymphocytes, eosinophills and foamy macrophages with or without foreign body giant cells at few places (Figure 1). All the three cases of mycetoma had the typical histopathology findings as neutrophillic infiltrate along with epitheloid and giant cell formation surrounding the actinomycotic/fungal colony. All three samples were culture negative.Only one of three cases of mycetoma had gram positive filaments in smear.This shows that FNAC/ histopathology with H and E Stain, was more sensitive than KOH or PAS stain examination in detecting fungal element.
Table 2: Results of Three different direct microscopy methods in detecting fungal elements on FNAC aspirate
c. Isolated fungal species: The rare fungal species that were isolated and identified as Exophiala jeanselmei (01) Figure 2, Cladosporium cladosporioides species (02) Figure 3, Pheoacremonium parasiticum species (01) Figure 4, Mucor species (01) based on characteristic colony morphology and microscopic findings. Table 3: showing the relationship between FNAC examination (H and E) andmycology culture method.
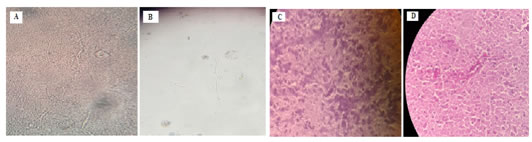
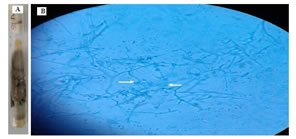
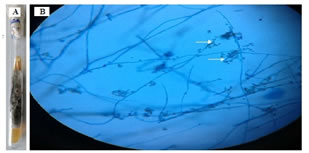
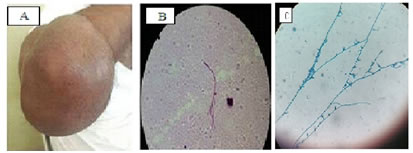
d. Treatment history: In our study the majority cases had received empirical treatment of varied duration with antibacterial/ antitubercular/ antifungal drugs and few had history of surgical excision. This may be because of its rarity that the clinician didn’t consider it as a differential diagnosis. Figure 1: A] 20% KOH Preparation Shows septate to moniliform hyphae with few large vesicular conidia along the hyphae B] KOH preparation shows yeast like cells and pseudohyphae (40X ) C] H and E stain shows distinct septate hyphae with chlamydoconidia arranged in chain along the hyphae as well as at its tip. (40X) D] PAS stain showing distinct pink coloured septate hyphae with large spherical or oval conidia along the hyphae, also some large yeast like cells in field. (40X) Figure 2: A] Culture on SDA- slow growing, on 9thday; smooth, velvety dark brown to blackish color fungal colony on obverse side B] Septate, pigmented hyphae and conidiophores that have taperedtip, oval and spherical conidia singly or in clusters seen at its tip and scattered (40X) Figure 3: A] SDA at 13 th day; brownish black, velvety on obverse surface. B] LCB stain of slide culture; pigmented septate hyphae, conidiophore are long, branched andgiving rise to branching chains of darkly pigmented budding conidia,also branch point seen as prominent attachment scars (shield cells)seen.(40X)
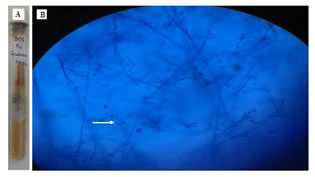
Figure 4: A]SDA at 11th day;dark olive gray toblackish white which changes to black discolouration B] septate pigmented hyphae, cylindrical phialides with oblong,some curved conidia clustered at its tip.(40X)
DISCUSSION Pheohyphomycosis, mycetoma, zygomycosis: The common subcutaneous mycosis included mycetoma followed by phaeohyphomycosis and zygomycosis.2,9Pheohyphomycosis is rare but tends to be more common in warm climates.10 Cutaneous is one of the five major clinical forms of zygomycosis9 Geographic variation:Subcutaneous mycosis is rare group of disorders.2Subcutaneous phaeohyphomycosis occurs throughout the world in all climates. In India, the climate ranges from tropical to temperate and the disease has been reported from the extreme north to south, except for the western and eastern regions.11 Many cases have been reported from sub-Himalayan belt, few cases from western coast and eastern coast but the central and north western arid zones of the country seem to be free of the disease. This had been attributed to environmental conditions (i.e.humidity and rainy season) which favours the survival of the pathogenic fungi in that area.12Our findings are consistent with the literature.Cutaneous and subcutaneous mycosis are an evolving field. Clinicians all over the world should be aware of the common manifestations of these diseases - infectious diseases - as they are increasingly reported and may lead to or be associated with dissemination.29 Infectious and non infectious nature of chronic cutaneous swellings:In our study, majority were of non infectious in origin (90.82%) than infectious one (9.17%). Histopathological examination of tissue specimens can readily establish the diagnosis.6 The demonstration of fungus in tissue section, provides ideal feedback and effective co-relation of particular culture isolate.4 We found majority (285/301) 94.68% of cases were tuberculosis origin while few (16/301) 5.31% had fungal (14/301) 4.65% and parasitic (02/301) 0.66% aetiology. Aditi chhonkar et al also reported three rare cases of cutaneous hyphomycosis.16 Subcutaneous mycosis:a. Clinical presentation:In the present study, the subcutaneous mycoses with no clinical suspicion were found in 14/301 (4.65%) cases.The subcutaneous mycosis is more of a histopathological than a clinical entity 15,17 Subcutaneous mycotic swelling were found commonly on extremities 12/14 (85.71%). This was similar to the findings of Bhat RM et al (64%).2 In our study, the commonest type of swelling was soft to firm in consistency. This was followed by cystic nature and firm to hard with or without sinuses. This was consistent with findings in study by Bhat RM et al2and Pang KR et al9 The cutaneous form of phaeohyphpmycosis include cyst and progressive soft tissue infection. 6, 10, 20We also found the three cases of typical clinical presentation of mycetoma. b. Age, sex and duration of symptoms, history of trauma: In our study, outdoor farm activities wascommonly associated findings. This was consistent with two studies. 15, 19 This could be attributable to trauma by vegetative matter, plant material or entry of contaminated soil into wounded area.2, 8 We didn’t find history of trauma in some patients as patients tend to forget minor traumatic incidences. This was similar to the study by Sharma NLet al.19 Infections not preceded by injury have also been reported 21We observed the most patients (78.57%) in present study, had age between 40 to 80 years followed by 15 to 40 years. The age group affected in a study by Sharma et al19 was 3 to 60 years.We also found male to female ratio as 6:1 which was very similar to (5.8:1) as found in study by Bhat RM et al.2 No race, sex, or age group is predisposed in study by Ziefer A et al10, and G. Bohelay et al18 The most patients (50%) had duration of symptoms between six months to one year as noted by Nand Lal Sharma et al12 c. Previous treatment history: In our study, the majority cases had received varied duration of empirical treatment with antibacterial, antitubercular, antifungal drugs. The similar history was found in (48%) cases in the study by Bhat RM et al2, and Pang KR et al 9 The management of these infections continues to be challenging. An approach that involves early diagnosis, the use of systemic antifungal agents (newer azoles) and local therapies, including surgical removal of lesions (or combined therapy) is the basis of the treatment of these diseases. 3, 19 d. Direct microscopy and culture:The laboratory diagnosis of fungal infections relies largely on direct as opposed to indirect methods. Considerable importance should be placed on direct microscopy in addition to isolation of organism.22 All of the 14 patients (100%) in this study had evidence of fungal infection based on FNAC examination (H and E stain). The majority samples were also PAS positive (71.42%). This approaches to 85% as observed by Bhat RM et al2. Histopathological stains have been useful to document tissue invasion. The direct examination of clinical specimens from the patient with eumycotic mycetoma or pheohyphomycosis demonstrates yellowish brown, septate to moniliform hyphae with or without budding yeast cells. The colonies of slow growing dematiacious molds are similar to one another and requires identification based on microscopic morphology.20We found typical histopathological/ FNAC findings of mycotic origin as seen in a study by Kiran kumar et al,15 Many more dematiaceous fungi have been found to cause infections associated with hyphal forms in the tissue, large ovoid yeast like cells ,aspects of pseudohyphae..8,18,23 FNAC/ Histopathology examination was found more sensitive to conventional microbiological culture methods in our study. Bhat RM et al2 and Sanjay G. Revankar8 had noted the same. The reports of the conventional pathological and mycological culture findings were noted to confirm the diagnosis. This had also been recommended in a review by Sanjay G. Revankar8. Repeated isolation of certain fungal species had importance to confirm its pathogenic potential.8 e. Fungal speciation: The culture was positive in 35.71 % cases in our study. This was similar as 36% to the study by Bhat RM et al2. This low culture positivity rate may be due to the fact which was mentioned in the literature. 22 as the fungi are much less abundant than bacteria in affected clinical material. The growth in culture may also be severely suppressed or absent in the individuals receiving antifungal therapy. 8 We have isolated rare fungal species in rare cases of subcutaneous mycosis. Bhat RM et al2 also noted the same. We have isolated Exophila jeanselmei (01), Cladosporium cladosporioides Spp. (02), PhaeoacremoniumParasiticum (01), and Mucor Spp. (01). We also found the associated positive findings for fungal infection on direct microscopy examination. Hence we confirm its pathogenic association with the concerned clinical lesion.Several species of Exophiala, Phialophora, Cladosporium, Xylohypha, Curvularia, Exserohilum, Bipolaris, Lecythophora, Alternaria, and other genera have been recognized as agents of subcutaneous phaeohyphomycosis .7, 24, 20Exophilaspp. has been increasingly reported in the literature as clinical pathogens. 25, 5E jeanselmei should be suspected in immunocompetent patients presenting with chronic subcutaneous lesions. 5Several cases of phaeohyphomycosis have been reported due to Cladosporium cladosporioides24, 26 including few from immune competent individuals.23Crouset al.27 proposed to accommodate the isolates that caused human infections, including Phaeoacremonium parasiticumand two new species, P. Inflatipes and P. rubrigenum. 27 The occurrence of Phaeoacremonium infections in humans has increased over the past two decades, and although most cases have been ascribed to known species, several unknown species have also been recorded.28 Morphologically, the genus Phaeoacremoniumis intermediate between the genera Acremonium and Phialophora. It is distinguished from Acremonium by its phaeoid vegetative hyphae and from Phialophoraby its narrow conidigenous cells and the inconspicuous collarets. 14 Our findings were consistent with pheoacremonium parasiticum. This was similar to the study by VP Baradkaret al14,Kiran Kumar K et al.15Thus we conclude that cases of phaeohyphomycosis found more prevalent in our region.Cystic or soft tissue chronic subcutaneous swellings (where Pheoacromonium parasiticum, Cladosporium cladosporioides. Exophila jeanselmei had been isolated) in immune competent individuals responded well to the treatment. The maximum chance of cure in immune competent individuals emphasizes the importance of the specific investigations.7,1,8,14,15 The limitations of our study:As this is a retrospective study we couldn’t found records of HIV status/ immune status of these patients which could have an impact on occurrence and severity of subcutaneous mycoses in these patients.As subcutaneous fungal infections were found as more common, widely disseminated, rapidly progressive and at greater risk of treatment failure in HIV positive individuals.5, 8We didn’t perform the antifungal sensitivity testing. Hence the further research is required in this arena. Our findings are based on conventional pathological and mycological techniques only. Even though the prolonged time was required to confirm the aetiology, this had an effect to reduce the long delay in specific treatment of these cases. The positive results in both the type of specific investigations confirm its pathogenic role. We also performed slide culture which had demonstrated typical fungal microscopic findings which helped in specification. The fungal culture is still considered the gold standard in diagnostic mycology.29
CONCLUSION The common infectious aetiology among the chronic subcutaneous swellings was found as extra pulmonary tuberculosis based on clinical and FNAC findings. This was followed by fungal and parasitic cause based on detail specific investigations. We found subcutaneous mycosis and its associated rare causative fungi as more prevalent (4.65%) in clinically non suspected cases. These findings emphasizes the clinician to consider it as important differential diagnosis. A high index of suspicion should be kept while dealing with such patients. The confirmation needs be done with mycological culture methods for the timely treatment of the condition.
ACKNOWLEDGEMENT We are thankful to the all the doctors and staff working in Surgery, Orthopedic and Pathology department of our institute for their kind co operation. Special thanks to Dr Shubha Deshpande and Dr Hanmannte for their guidance and kind support.
REFERENCES
|
|
 Home
Home