Changing trends in resistance pattern of methicillin resistant staphylococcus aureus in a tertiary care hospital, Maharashtra, India
Kasturi1, Rupali Satyen Mantri2*, Nitin Anil Ambhore3
1,2Assistant Professor, 3Professor and HOD, Department of Microbiology, Government Medical College, Akola, Maharashtra, INDIA.
Email: r.mantri@rediffmail.com, kasturi07081@gmail.com
Abstract Background: Staphylococcus aureus is a common cause of hospital and community‑acquired infections worldwide. The resistance patterns of prevalent Methicillin Resistant Staphylococcus aureus (MRSA) strains in any setup are liable to continuous changes over a period of time. Materials and Methods: 167 Staphylococcus aureus isolated from various clinical specimens were tested for Methicillin resistance using Cefoxitin disc. Antimicrobial susceptibility testing was performed by Kirby Bauer disk diffusion method. Results: A total of 64.67% MRSA were detected. Out of these, 15.74% were community-acquired MRSA (CA-MRSA) and 84.23% were hospital-acquired MRSA (HA-MRSA).We observed an increased resistance towards Ciprofloxacin and Erythromycin as compared to a previous study done in the same hospital. All MRSA isolates were sensitive to Vancomycin, Linezolid. Inducible clindamycin resistance was higher amongst HA-MRSA (14.29%) as compared to CA- MRSA (11.76%).Conclusion: The reported rate of MRSA incidence is alarming. Periodic surveillance of antimicrobial susceptibility pattern, formulation of a definite antibiotic policy, patient isolation, implementation of proper personal hygiene, hand washing will be helpful.
Key Words: MRSA, community-acquired MRSA, hospital-acquired MRSA, Inducible clindamycin resistance, periodic surveillance.
INTRODUCTION
Staphylococcus aureus is a common cause of hospital and community‑acquired infections worldwide, manifesting from minor skin diseases to life‑threatening infections.1,2 The ability of the organism to cause a multitude of infections is probably due to the expression of myriads of different toxins, virulence factors and also cell wall adhesion proteins and Staphylococcal superantigen like proteins involved in immune evasion.1,3 Methicillin resistant staphylococcus aureus (MRSA) is a resistant variant of Staphylococcus aureus which has evolved an ability to survive treatment with beta antibiotics which includes penicillin, methicillin, cephalosporins and to various other groups of antimicrobial agents.4
Once prevalent in healthcare setup for more than 40 years, MRSA has migrated to the community in recent years.5 The prevalence of multidrug-resistant strains in Indian hospitals i.e. hospital acquired MRSA (HA-MRSA) ranges from 15 to 70%6 Community-acquired MRSA (CA-MRSA) has evolved as a novel emerging pathogen in patients who had no contact with health care setup.5 Unlike HA-MRSA which typically are resistant to multiple antibiotics, CA-MRSA tend to be susceptible to other antibiotic classes and often are resistant to only β lactam antibiotics.7 The resistance patterns of prevalent MRSA strains in any setup are liable to continuous changes over a period of time, owing to changes in antibiotic prescription patterns, infection control measures and awareness among healthcare workers 8.These facts clearly highlight the need of a characterization of MRSA strains at a regular basis at all levels. Hence, the present study was undertaken to find out the incidence of MRSA isolates, proportion of HA-MRSA and CA-MRSA, and to determine changing resistance patterns of MRSA infection in our hospital over past five years.
MATERIAL AND METHODS
This retrospective observational study was conducted for a period of 10 months, from September 2018 to June 2019 in the Department of Microbiology, Government Medical College, Akola. 167 Staphylococcus aureus isolated from various clinical specimens such as pus, wound swab, blood, urine, sputum and other body fluids were considered for the study.
Detection of methicillin resistant Staphylococcus aureus
Methicillin resistant Staphylococcus aureus detection was done using cefoxitin disc of 30 μg. Those isolates showed zone of inhibition <21 mm were considered as MRSA 9.
Antibiotic susceptibility testing
Antibiotic susceptibility test was performed by Kirby-Bauer disk diffusion method. Drugs used were Erythromycin (15 μg), Clindamycin (2 μg), Ciprofloxacin (5 μg), Cefoxitin (30 μg), Tetracycline (30 μg), Co- trimoxazole (1.25/23.75μg), Vancomycin (30 μg) and Linezolid (30 μg) (Hi-Media Pvt. Ltd., Mumbai, Maharashtra, India). Staphylococcus aureus ATCC 25923 was used as the control strain for antibiotic sensitivity testing.
Isolates that were Clindamycin susceptible and Erythromycin resistant were tested for inducible resistance by the use of D-zone test as per CLSI guidelines.
Categorization of methicillin resistant Staphylococcus aureus isolates into hospital acquired-methicillin resistant Staphylococcus aureus and community acquired-methicillin resistant Staphylococcus aureus
Based on the history of the patient, the MRSA isolates were categorized into CA or HA. Basically if an infection occurs among the out patients or inpatients with an MRSA isolate earlier than 48 hours of hospitalization, is considered as CA-MRSA, and if MRSA strain isolated after 48 hours of hospitalization or from a patient with a history of hospitalization for surgery or dialysis, or of a residence in a long-term care facility within 1 year of the MRSA culture date will come under HA-MRSA 10.
RESULTS
A total of 64.67% (108/167) MRSA were detected from various clinical samples using Cefoxitin disc diffusion technique. Out of these, 15.74% (17/108) were community-acquired MRSA (CA-MRSA) and 84.23% (91/108) were hospital-acquired MRSA (HA-MRSA).
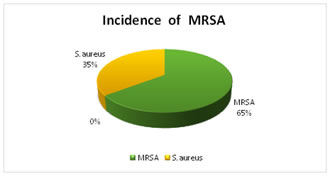
Figure No.1: Incidence of MRSA
Antibiotic sensitivity results:
All the isolates were sensitive to Vancomycin (100%) and Linezolid (100%). The HA-MRSA strains were more resistant to the drugs used as compared to the CA-MRSA strains. When compared to the previous study done in the same hospital in 2014, it was found that the MRSA strain have shown alarming increase in resistance patterns for most of the drugs except Clindamycin.
Table 1: Antibiotic Resistance pattern of CA-MRSA and HA-MRSA
Antibiotics |
CA-MRSA
n=17 |
HA-MRSA
n=91 |
Cefoxitin (30μg) |
17 (100%) |
91 (100%) |
Clindamycin (2μg) |
5 (29.41%) |
36 ( 40.95%) |
Ciprofloxacin (5μg) |
6 ( 35.29%) |
33 (36.26%) |
Erythromycin (15μg) |
7 (41.12%) |
42 (46.15%) |
Tetracycline (30μg) |
8 (47.06%) |
53 ( 58.24%) |
Cotrimoxazole (1.25/23.75μg) |
9 (52.94%) |
59 (64.84%) |
Linezolid (30μg) |
0 |
0 |
Vancomycin (30μg) |
0 |
0 |
Table 2: Comparison of antibiotic resistance of MRSA from previous study done in the same hospital
Antibiotics |
2014
n=112 |
2019
n=108 |
Clindamycin (2μg) |
59 (52.67%) |
41 (37.96%) |
Ciprofloxacin (5μg) |
25 (22.32%) |
39 (36.11%) |
Erythromycin (15μg) |
32 (28.57%) |
49 (45.37%) |
Tetracycline |
62 ( 55.35%) |
61 (56.48%) |
Cotrimoxazole (1.25/23.75μg) |
68 (60.71%) |
68 (62.96%) |
Linezolid (30μg) |
0 |
0 |
Vancomycin (30μg) |
0 |
0 |
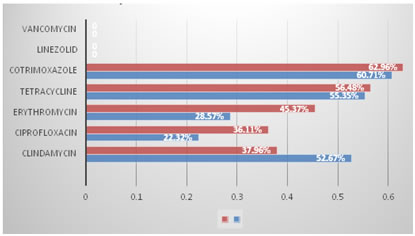
Figure 3: Comparison of antibiotic resistance of MRSA from previous study
D-Test Results of MRSA
In the present study, D test positivity was seen in 13.88% (15/93) of the MRSA isolates. D test was positive in 11.76 % of CA-MRSA and 14.29% of HA-MRSA isolates.
Table 3: D-Test Results of MRSA
|
D-test positive |
D-test negative |
CA-MRSA |
2 ( 11.76%) |
15 (88.24%) |
HA-MRSA |
13 ( 14.29%) |
78 (85.71%) |
Total |
15 (13.88%) |
93 (86.12%) |
DISCUSSION
Incidence of MRSA in our study is 64.67% which resembles with the reports of Majhi et al.11 Studies done by Subramanian et al.12 reported a higher percentage whereas Gade et al.13 and Chadha et al.7 recorded a lower percentage of MRSA isolates. Thus, the prevalence of MRSA varies in different parts of India and is not uniform. Reports from a Delhi hospital showed a prevalence rate of 51.6% in 2001, where as it was reported as 38.44% in the same hospital in 2008.14 The present study reported a higher percentage of HA-MRSA (84.23%) than CA-MRSA (15.74%). Also, the HA-MRSA isolates were more resistant to antibiotics when compared to CA-MRSA. It is in accordance to other studies done by Chadha et al7 and Vysakh and Jey et al.15 Both HA-MRSA and CA-MRSA possess different gene like mecA gene and PVL gene respectively, which enhance resistance to antibiotics and inappropriate use of antibiotics also promotes resistance that could be a possible reason for the difference in resistance pattern of HA-MRSA and CA-MRSA.10 We observed 13.88% inducible clindamycin resistance amongst total MRSA isolates which correlated with the findings of Chadha et al.7 and Saikia et al.16 It was also observed that percentage of inducible clindamycin resistance was higher amongst HA-MRSA (14.29%) as compared to CA- MRSA (11.76%). Chadha et al7 also reported similar results. However, Patil Nilima et al17 suggested that inducible clindamycin resistance is more common in community acquired than in hospital acquired Staphylococcus aureus isolates. Different patterns of resistance to clindamycin observed in various studies may be due to different geographical region for the study, age group, methicillin susceptibility pattern and from hospital to hospital.17 This study analysed antibiotic resistance pattern of MRSA isolates and found three major changes in antibiotic resistance over five years. Firstly, an increased resistance towards Ciprofloxacin and Erythromycin. Secondly, all the isolates were sensitive to Vancomycin and Linezolid. So, Glycopeptides and Linezolid continue to remain the mainstay for treatment for MRSA infections Thirdly, overall resistance to the drug Clindamycin has decreased over the years. However, the emergence of inducible clindamycin resistance is an important issue. The incorporation of D-test into routine Kirby–Bauer disk diffusion method has enabled us in guiding the clinicians regarding judicious use of Clindamycin.
CONCLUSION
In developing country like India, MRSA infection and its resistance towards the commonly used antibiotics have imposed a high burden on the healthcare system. HA- MRSA infection is a major cause of concern to the health care workers. Further spread of MRSA among community, that is, CA-MRSA is a current challenging problem. This emphasizes on the importance of regular surveillance of hospital-associated infections, monitoring of antimicrobial susceptibility pattern of MRSA and formulation of a definite antimicrobial policy. In addition, implementation of prevention strategies, including proper personal hygiene, hand washing and pre-screening for carrier status before hospital admission will help us to control the drug resistance.
REFERENCES
- Gebremariam TT, Zelelow YB. A systemic review of antimicrobial resistance pattern of methicillin-resistant Staphylococcus aureus. Saudi J Health Sci 2014;3:71-4.
- Mir BA, Srikanth. Prevalence and antimicrobial susceptibility of methicillin resistant Staphylococcus aureus and coagulase‑negative staphylococci in a tertiary care hospital. Asian J Pharm Clin Res 2013;6:231‑3.
- Shambat S, Nadig S, Prabhakara S, Bes M, Etienne J, Arakere G. Clonal complexes and virulence factors of Staphylococcus aureus from several cities in India. BMC Microbiol 2012;12:64.
- Bhavsar R, Garala NJ, Garala RN, Patel P, Javadekar TB, Patel H, Tadvi J, Mehta K. Antimicrobial susceptibility pattern of methicillin resistant staphylococcus aureus isolated from various clinical samples at SSG hospital, Baroda. J Res Med Den Sci 2015;3(1):43-6.
- Basak S, Mallick SK, Bose S. Community associated methicillin resistant Staphylococcus aureus- an emerging pathogen: Are we aware? J Clin Diagn Res 2010;4:2111-5.
- Arakere G, Nadig S, Swedberg G, Macaden R, Amarnath SK, Raghunath D. Genotyping of methicillin resistant Staphylococcus aureus strains from two hospitals in Bangalore, South India. J Clin Microbiol 2005;43:3198-202.
- Chadha T, Kulsum SN, Adlekha S, Mailapur PC. Comparison of antibiotic susceptibility pattern of community- and hospital-acquired methicillin-resistant Staphylococcus aureus with special reference to inducible clindamycin resistance in a tertiary care hospital in southern India. Med J DY Patil Univ 2014;7:439-42.
- More S.R., Tadvi Khan Saleha Kauser, Kandle SK ,Rathod V.S. Changing Trends in Resistance Pattern of Methicillin Resistant Staphylococcus aureus in Burn Patients. Int.J.Curr.Microbiol.App.Sci. 2019;8(01): 22-27.
- M 100-S 25. Performance standards for antimicrobial susceptibility testing 24th informational supplement CLSI; Clinical Laboratory Standards Institute January 2014.
- Abbas A, Nirwan PS, Srivastava P. Prevalence and antibiogram of hospital acquired-methicillin resistant Staphylococcus aureus and community acquired-methicillin resistant Staphylococcus aureus at a tertiary care hospital National Institute of Medical Sciences. Community Acquir Infect 2015;2:13-5.
- Majhi S, Dash M, Mohapatra D, Mohapatra A, Chayani N. Detection of inducible and constitutive clindamycin resistance among Staphylococcus aureus isolates in a tertiary care hospital, Eastern India. Avicenna J Med 2016;6:75-80.
- Subramanian A , Chitalia V , Vaidya S P, Warke RV , Chowdhary A , Deshmukh RA Detection of Macrolide, Lincosamide and Streptogramin Resistance among Methicillin Resistant Staphylococcus aureus (MRSA) in Mumbai JKIMSU, Vol. 4, No. 3, July-September
- Gade, N.D., Qazi, M.S. 2013. Inducible clindamycin resistance among Staphylococcus aureus isolates. Indian J. Basic Appl. Med. Res., 2(8): 961-967.
- Tiwari HK, Sapkota D, Sen MR. High prevalence of multidrug-resistant MRSA in a tertiary care hospital of northern India. Infection and Drug Resistance 2008;1:57-61
- Vysakh PR, Jeya M. A comparative analysis of community acquired and hospital acquired methicillin resistant Staphylococcus aureus. J Clin Diagn Res 2013;7:1339-42.
- Saikia L, Nath R, Choudhury B, Sarkar M. Prevalence and antimicrobial susceptibility pattern of methicillin resistant Staphylococcus aureus in Assam. Indian J Crit Care Med 2009;13:156-8.
- Patil Nilima R, Shah Shilpa R,Mali Ulhas S,Jadhav Suvarna T. Study of community and hospital associated methicillin resistant Staphylococcus aureus with special reference to inducible clindamycin resistance in a tertiary care hospital J Pharm Sci Innov. 2015;4(1):68-71.