Official Journals By StatPerson Publication
|
Table of Content Volume 12 Issue 3 - December 2019
Speciation and resistant pattern of candida by VITEK-2 XL at a tertiary care teaching hospital in Western Uttar Pradesh, India
Neelam Gupta1, Dharmender Gupta2*
1Assistant Professor, Department of Microbiology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, INDIA. 2Associate Professor, Department of Pharmacology, Varunarjun Medical College and Rohilkhand Hospital, Banthra, Uttar Pradesh Shahjahanpur, INDIA. Email: neelam.10apr@gmail.com
Abstract Background: Candida species are normal flora of human skin and mucosa. In recent decades deep fungal infection as well as candidemia has a high impact on public health due to increased hospitalization. Overuse of broad spectrum antimicrobial for bacterial ifection disturb the normal flora of body which in turns increase the incidence of candidiasis. Aim: An increase in infection by non-albicans species is also noted due to frequent use of azoles. Present study to isolate and know the antifungal drug sensitivity pattern of various candida albicans and non albicans candida (NAC). Material and Methods: This study was conducted from June 2016 to May 2017 in microbiology department of SRMSIMS Bareilly. Total 149 candida like growth were isolated on SDA in various samples including urine, blood, and sputum. All isolates were identified and their antifungal sensitivity test was done in VITEK 2-XL using ID-YST and AST-YST kits respectively. Result: Out of 149 isolates 53 (35.57%) were Candida albians and 96 (64.43%) were NAC. Among NAC Candida tropicalis (48.9%) was most common. About antifungal sensitivity test Fluconazole resistance was detected in 8 (5.37%) candida species followed by voriconazole i.e.5 (3.36%) followed by Amphotericin B i.e. 4 (2.68%). Resistance for fungins was detected in only 2 candida albicans isolates NAC were sensitive. Conclusion: Candida albicans and non albicans candida species are emerging as an important cause of infection. Antifungal resistant strains underline the demand of antifungal sensitivity testing for these isolates. Key Word: Non albicans candida, Sensitivity Pattern, Antifungal Drugs, SRMSIMS.
INTRODUCTION Candida species are part of the normal flora of skin, gut and genitals and is capable of causing a variety of infections and is emerging as an important nosocomial pathogen. ¹ The increasing incidence of HIV infections, widespread use of antibiotics, organ transplantation, use of immunosuppressive agents and emergence of resistance to antifungal agents has contributed to the increased incidence of Candida infections. The genus is composed of a hetrogenous group of organism, and more than 17 different Candida species are known to be the etiological agents of human infection. However, more than 90% of invasive infections are caused by C. albicans, C. tropicalis, C. parapsilosis, C. glabrata, C. krusei.⁹ We studied the prevalence of various Candida species in hospitalized patients at a tertiary care centre along with their antifungal susceptibility pattern to commonly used antifungal drugs by VITEK-2, an automated system. This study was done to identify species from different isolates and to determine the resistance of various candida albicans and non albicans candida by vitek 2 automated system.
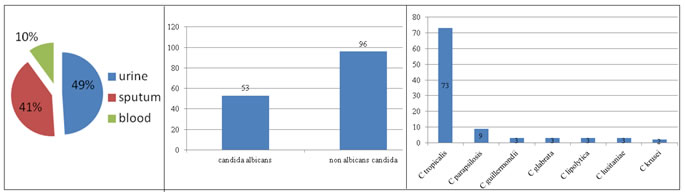
MATERIAL AND METHODS The study was carried out from June 2016 to May 2017, in microbiology department of SRMSIMS Bareilly. Total 149 Candida like growth were isolated on SDA in various samples including urine, blood, and sputum. All isolates were confirmed by gram staining and germ tube test and then identified with VITEK 2 Compact (Biomerieux, France) using VITEK 2 cards for identification of yeast and yeast-like organisms (ID-YST cards) kits. Antifungal susceptibility testing was performed with AST YS07 Kits on VITEK 2 compact. Standard operative procedures as described by the manufacturer were followed.5 RESULTS The study included 149 samples processed in the Vitek 2 compact system. Samples included: 73(49%) urine, 61(41%) sputum, 15(10%) blood. Figure 1 Figure 2 Figure 3: Number of Non albicans candida Out of 149 isolates Non albicans candida (NAC) were 96 (64.4%) and Candida albicans were 53(35.6%).
Resistance for fluconazole 5.36%, voriconazole 3.35%, caspofungin 1.34%, micafungin 0.67%, amphotericin B 2.68%, flucytosine 1.34% were respectively.We observed that candida albicans was less resistant to all drugs as compared to non albicans candida species. Antifungal Resistance pattern of Candida species in various samples In the urine sample, C. albicans was 100% sensitive to fluconazole, fungins, amphotericinB and flucytosine except voriconazole,92.3% sensitive, while non albicans 89.36% sensitive to fluconazole, 95.74% sensitive to voriconazole, 93.61% sensitive to flucytosine and 100% sensitive to fungins and amphotericin B. In sputum, C. albicans 100% sensitive to fluconazole, voriconazole and flucytosine except fungins were sensitive 96.15% and amphotericin B sensitive 92.30%. While non albicans 94.28% sensitive to fluconazole and amphotericin B, 97.14% sensitive to flucytosine, 100% sensitive to fungins and voriconazole. In blood, C.albicans 100% sensitive to all drugs, while non albicans 92.85% sensitive to azoles and 100% sensitive to fungins, amphotericin B, and flucytosin. Table 2: ANTIFUNGAL RESISTANCE PATTERN OF CANDIDA SPECIES IN VARIOUS SAMPLES
Table 3
DISCUSSION In the present study, we observed that non albicans Candida species had predominance over C. albicans, which is consistent with the published report from different parts of the world.⁶⁷⁸ C. tropicalis was the most common isolate in all samples, followed by C. albicans. S Prassna et al,reported the susceptibility profile of candida isolates maximum fluconazole and voriconazole resistance was seen in C.tropicalis followed by C.albicans and others.²
CONCLUSION Species-level identification and antifungal susceptibility assessment of Candida strains should be obviously performed to achieve better clinical results. Early antifungal therapy improves the outcome.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home