Official Journals By StatPerson Publication
|
Table of Content Volume 12 Issue 3 - December 2019
Comparison of procalcitonin and c-reactive protein with blood culture in early diagnosis of neonatal sepsis
Swati Karad1, Desma D'Souza2*, Sujata Baveja3
1Resident Medical Officer, 2Assistant Professor, 3Professor and HOD, Department of Microbiology, 4th floor, College Building, LTMMC and GH, Sion, Mumbai, Maharashtra, INDIA. Email: drdesma@gmail.com
Abstract Background: Neonatal sepsis is an invasive infection which occurs in the first four weeks of life and is a leading cause of morbidity and mortality in neonates. Early diagnosis of neonatal sepsis is very important in controlling morbidity and mortality. The aim of present study was to evaluate C-reactive protein (CRP) and Procalcitonin (PCT) as diagnostic markers for early diagnosis of neonatal sepsis in comparison with conventional blood culture. Method: Total 72 clinically suspected cases of sepsis in neonatal intensive care unit (NICU) were analyzed for clinical profile and risk factors. Blood samples were obtained from each neonate prior to administration of antibiotics and processed for blood culture, CRP and PCT test. Results: Out of 72 cases, 36.11% showed growth in blood culture, 68.05% showed significantly high CRP levels and 56.95% showed significantly high PCT levels. Taking blood culture as gold standard the sensitivity, specificity, PPV and NPV of CRP was found to be 100%, 50%, 53.06% and 100% respectively and the sensitivity, specificity, PPV and NPV of PCT was found to be 100%, 67.39%, 63.41% and 100% respectively. There were 38 cases positive by both CRP and PCT and 20 cases negative by both CRP and PCT. 11 cases were positive by CRP and negative by PCT and 3 cases were PCT positive and CRP negative. Conclusion: Both CRP and PCT help in early diagnosis of neonatal sepsis. But PCT test has higher specificity as compared to CRP test, thus should be incorporated routinely for early diagnosis of neonatal sepsis. Key words: Neonatal Sepsis, C-reactive protein, Procalcitonin, Blood culture, Antibiotics, Sensitivity, Specificity.
INTRODUCTION Neonatal sepsis is a clinical syndrome characterized by signs and symptoms of infection with or without accompanying bacteremia in the first month of life. It encompasses various systemic infections such as meningitis, pneumonia, arthritis, osteomyelitis, and urinary tract infections 1.The incidence of neonatal sepsis varies from 1 to 4 cases per 1000 live births in developed countries. According to the data from National Neonatal Perinatal Database (NNPD 2002-03) it is 30 per 1000 live births in India. Nearly one-fifth of neonates with sepsis die in the hospital; the figure rises to 50% for those with culture proven sepsis. They stay longer in the hospital, consume more resources and are also at a high risk of major neurodevelopmental disabilities at a later age 2. Therefore timely diagnosis of neonatal sepsis is very important in controlling morbidity and mortality. The diagnosis of neonatal sepsis is based on clinical presentation and the laboratory investigations. Blood culture is the most valuable diagnostic method for neonatal sepsis and it is found to be positive in 25-54% cases.3 Although blood culture is gold standard for diagnosis of neonatal sepsis and allows targeted antimicrobial therapy, its result may be delayed for up to 48 hours and it may yield negative results in many cases of septic shock. Haematological parameters useful in evaluation of neonatal sepsis are complete blood count, white blood cell count, absolute neutrophil count and immature/total neutrophil ratio, however these tests have low sensitivity and are nonspecific 4. During the last decades efforts have been made to improve the laboratory diagnosis of neonatal sepsis by studying a large variety of inflammatory markers with diverse success. Some like PCT and CRP have demonstrated their benefit in clinical practice and have been implemented in neonatal intensive care units. Some studies reported that PCT is more reliable than CRP for the diagnosis of neonatal sepsis 5, 6 others did not find any advantage of PCT over CRP 7, 8. Thus the present study was undertaken to find out the correlation between blood culture, serum PCT and CRP positivity in clinically suspected cases of sepsis in neonates admitted in the hospital and to compare the efficacy of CRP and PCT tests.
MATERIALS AND METHODS After obtaining approval from the Institutional Ethics Committee, an observational study was conducted in Department of Microbiology at a Tertiary Care Hospital during the period of one year. A total of 72 patients admitted with suspected neonatal sepsis and antibiotic naive neonates were included in this study. Neonates with hematological disorders, any congenital abnormalities, neonates on corticosteroid / antimetabolite therapy and on antibiotics were excluded from the study. Written informed consent was taken from the guardian of child for participation in the study. A detailed history including the presenting complaints, past history and risk factor was elicited for each patient and duly recorded in the case record forms. Blood samples (2-3 ml) were collected from each neonate prior to administration of the antibiotics for the laboratory investigations of blood culture, serum CRP and serum PCT. The first 1 ml of blood was immediately inoculated into blood culture bottle containing tryptic soy broth after disinfecting the top of the bottle with an alcohol swab. Culture bottle was gently rotated to mix the blood and culture medium. Remaining 1-2 ml blood sample was collected in sterile vaccutainer tube. The blood culture bottle and sterile vaccutainer tube were transported immediately to the microbiology laboratory for further processing.
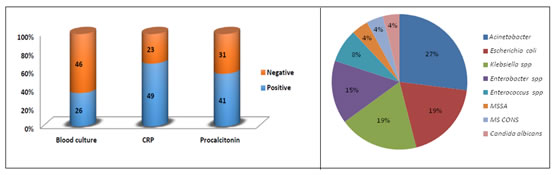
After receiving the blood culture bottle in microbiology laboratory it was incubated at 37°C overnight. After overnight incubation, first subculture was done on blood agar and MacConkey agar and plates were further incubated for 24 hrs at 37°C. The blood culture bottles were also re-incubated. Any growth on these plates was identified by standard biochemical tests 9. Antibiotic susceptibility test was put for each growth as per CLSI 2015 guidelines. If there was no growth in first subculture, second subculture was done on fourth day and third subculture on seventh day and the same procedure as above was repeated. The bottle was discarded after seventh day, if there was no growth at all. For serum separation 1-2 ml of blood collected in sterile vaccutainer tube was allowed to clot. After centrifugation for 3000 RPM for 15 minutes, serum was separated and divided into 2 aliquots. First aliquot of serum was used for CRP detection immediately. It was performed by Omega Diagnostics rapid latex agglutination kit. [Kit used: DZE201120978; Lot no: 201502; Exp. date: 2015-08]. A positive result was indicated by the obvious agglutination pattern of the latex in a clear solution and a negative result was indicated by no change on the test slide. The other aliquot was was used for procalcitonin analysis using Sunred human Procalcitonin ELISA kit. [Kit used:7049947; Lot No:2015-02; Expiry date:2017-10]. The positive and negative controls were included for each test. The absorbance values were plotted and calculated on standard linear regression equation. Statistical analysis Statistical analysis was performed with the software package: PASW statistic 18 for Windows. The significance of difference of proportion of categorical variables among groups was examined by the chi-square test and difference in mean by student’s t test. A value of P of ≤0.05 was considered significant for all statistical analysed. Out of 72 patients, 58.3% were male and 41.7% were female, (p>0.05). Male: Female ratio was 1.4:1. Maximum cases of neonatal sepsis belonged to age group less than 3 days (65.3%)followed by age group between 3-28 days (34.72%), (p<0.05).Mean age of the study cases was 4.6d ± 3.4days. Early onset neonatal sepsis (< 3days) was significantly higher than late onset sepsis (3-28 days). Most common presenting symptoms were poor feeding (68.1%),fever (25%) and birth asphyxia (22.2%) while jaundice (5.6%) and seizures (1.4%) were uncommon. This variation in percentage in presenting symptoms was found to be statistically significant (p<0.001). Out of 72 cases, 42 (58.3%) were term babies and 30 (41.7%) were preterm babies. The mean birth weight of the study cases was 1815g ± 342g, ranging from 820g- 2570g. Out of 72 cases, 26 (36.11%) were blood culture positive, 49 (68.05%) were CRP positive and 41(56.95%) were PCT positive as shown in figure 1. Taking blood culture as gold standard sensitivity, specificity, PPV and NPV of C-reactive protein and procalcitonin were analysed. (Table 1). All blood culture positive samples were analyzed for type of organism and antimicrobial susceptibility of the isolated pathogen. The distribution of organisms isolated in blood culture is shown in figure 2. The most common organisms isolated were Acinetobacter species(27%), Klebsiella pneumoniae (19%), E.coli (19%) and Enterobacter spp.(15%). Out of 7 Acinetobacter species 71.4% were sensitive to ciprofloxacin and imipenem, 57.1% were sensitive to piperacillin-tazobactam and netilmycin, 42.9% were sensitive to amikacin and ampicillin-sulbactam, 14.35% were sensitive to cefotaxime and piperacillin. 28.6% Acinetobacter species were resistant to carbapenem but all were sensitive to tigecycline and colistin. Out of 5 Klebsiella species, 60% were sensitive to amikacin, ciprofloxacin, cefotaxime and imipenem. 20% were sensitive to netilmycin. 40% Klebsiella species were resistant to carbapenem. Out of 5 Escherichia coli, 60% were sensitive to netilmycin and 40% were sensitive to amikacin, ciprofloxacin, imipenem, piperacillin-tazobactam and 60% Escherichia coli were resistant to carbapenem. Out of 4 Enterobacter species 50% were sensitive to ciprofloxacin and imipenem; 25% were sensitive to amikacin, piperacillin; 50% were sensitive to carbapenem and 50% were multi drug resistant. Out of 4 Gram positive cocci, 2 were Enterococcus species sensitive to vancomycin and linezolid. There was single isolate of Methicillin sensitive Staphylococcus aureus (3.8%) (MSSA) and Methicillin sensitive coagulase negative Staphylococcus (3.8%), (MSCONS) and both were sensitive to all drugs except penicillin. Blood culture positivity indicated definitive sepsis and this was analyzed with presence and absence of risk factors, also with platelet count and total leucocyte count (Table 2). The variation in percentage of risk factors was found to be statistically significant (p<0.001). Total of 69 cases were analyzed for outcome and 3 cases were excluded from the analysis as their actual outcome is unknown. Out of 25 blood culture positive cases 12(48%) expired and 13(2%) were discharged whereas out of 45 blood culture negative cases 5(11.4%) expired and 39(88.6%) were discharged. This difference was found to be statistically significant, (p=0.001). Table 1: Comparison of CRP and PCT positivity with Blood Culture as well as comparison of CRP positivity with PCT positivity (n=72)
*p value ≤ 0.05 is significant
Table 2: Correlation of Risk Factors, platelet and total leucocyte count (TLC) with Blood Culture Positivity
*p value ≤ 0.05 is significant Figure 1 Figure 2 Figure 1: Percentage Positivity of Blood Culture, C - reactive protein, Procalcitonin in Study Cases (n= 72); Figure 2: Distribution of organisms isolated in blood culture (n=26) Methicillin sensitive Staphylococcus aureus (MSSA), Methicillin sensitive coagulase negative Staphylococcus (MS CONS) DISCUSSION Male predominance was observed in the present study. Male: female ratio was 1.4:1. These findings are in concordance with the study done by M Mutlu et al 24 but discordant with the study done by Naglaa et al 29. Early onset neonatal sepsis (65.3%) was higher than late onset neonatal sepsis (34.72%) in this study as seen in the study done by Basu et al 30 and Zahedpasha et al 31. In current study the most common presenting symptom was poor feeding, fever, birth asphyxia and vomiting. Katua et al 32 and by NK Anand et al 11 also observed that refusal to feeds, lethargy, diarrhea, temperature abnormality, abdominal distension, jaundice and vomiting were among the most common presenting features. These studies show that clinical features of neonatal septicaemia are nonspecific and may be clinically indistinguishable from those occurring in non-infectious conditions during neonatal period. In the present study the most common maternal risk factors observed were PROM, UTI, chorioamnionitis and intrapartum fever. Similar findings were observed by Bhat et al 34 and Naher et al 5. Present study did not observe an association between prematurity and risk of neonatal sepsis and this finding correlates with the study done by Gebremedhin et al 12. However, in the study done by Vinay B S et al 36, Basu et al 30 and M Mutlu et al 24 prematurity was found to be a risk factor. In present study maximum cases had birth weight less than 2000 g. Mean birth weight was 1815 ± 342gm. These findings correlated well with study done by M Mutlu et al 24 and Basu et al 30. It was thus seen that infection was more common in low birth weight baby as compared to normal birth weight babies. Out of 72 cases 36.11% were blood culture positive and 63.89% were blood culture negative. Sepsis cannot always be excluded even when blood cultures are found to be negative. Inoculation of only 0.5-1 ml of blood decreases blood culture sensitivity, as approximately 60-70% of infants have a low level of bacteremia. Theoretically for optimal results, 6 ml of blood required which is not feasible 16 hence there is need for an alternative solution. CRP is an acute phase reactant and highly sensitive indicator of infection. It is synthesized by the liver and is increased up to 1000 fold within 4-6 hours of an inflammatory process.39 Its level rapidly declines with elimination half-life of 19 hours.38 Use of CRP for the diagnosis of neonatal sepsis has been widely studied. CRP is easy, rapid, cost effective and readily available test. In the present study 49 cases were C-reactive protein positive. 23 cases were positive by C-reactive protein and negative by blood culture. Taking blood culture as a gold standard sensitivity of C-reactive protein was 100%, specificity was 50%, positive predictive value was 53.06% and negative predictive value was 100%. The CRP sensitivity, specificity, PPV and NPV were found to be 100%, 75%, 77% and 100% respectively in a study by Gandhi T et al 40 and 100%, 87.3%, 88.3% and 100% respectively in a another study by Anuradha et al41. These findings correlate well with present study. In a study by Boo et al 42 CRP sensitivity, specificity, PPV and NPV were found to be 55.6%, 89.9%, 58.8% and 88.6% respectively. This finding is discordant with present study. PCT a precursor of calcitonin is a 116 amino acid protein secreted by the C cells of thyroid gland in normal situation but its levels increase in septicaemia, meningitis, pneumonia and urinary tract infection.44,45 It is also produced by macrophage and monocyte cells in severe bacterial infection and sepsis.46. In the present study 41 cases were procalcitonin positive. 15 cases were positive by procalcitonin and negative by blood culture. Taking blood culture as gold standard sensitivity of procalcitonin was 100%, specificity was 67.39%, positive predictive value was 63.41% and negative predictive value was 100%. The PCT sensitivity, specificity, PPV and NPV were found to be 92.8%, 75.0%, 59.0% and 96.0% respectively in a study by In Sucilathangam et al(37) and in another study by Vazzalwar et al 47, sensitivity of PCT was found to be 97% and the specificity was 80%. In a another study by Bonac et al43 sensitivity of procalcitonin was 59%, specificity was 82%,positive predictive value was 36% and negative predictive value was 96%. These findings are discordant with present study. In the present study all blood culture positive cases were positive by C-reactive protein and Procalcitonin test. Sensitivity of CRP and PCT was 100% in detecting neonatal sepsis. Specificity of PCT was 67.4% and specificity of CRP was 50%. Thus PCT has better specificity than CRP in detecting neonatal sepsis. Both PCT and CRP were found to have the same sensitivity and negative predictive value. Koksal et al 48 study also concluded that procalcitonin level was superior to CRP in terms of an early diagnosis of neonatal sepsis. PCT is highly specific for bacterial infection and it helps differentiating it from viral infection. PCT helps in an early diagnosis of the sepsis on the day of the admission itself, before the blood culture report is ready (usually after 3-5 days). PCT helps in avoiding antibiotic therapy where it is not 49 required and thereby reducing the cost and the occurrence of bacterial resistance. PCT can also be employed for the prognosis of sepsis. Nelly et al 50 concluded that PCT is more reliable than CRP for the diagnosis of neonatal sepsis. In contrast in Blommendahl et al 51, Janota et al 52, Koskenvuoet al 33 and Perez solis et al 35 study the specificity of PCT was found to be lower than that of CRP.
CONCLUSION Neonatal sepsis is an important cause of morbidity and mortality in developing countries. Therefore an early diagnosis of neonatal sepsis will help to reduce morbidity and mortality. Blood culture is routinely used diagnostic method for neonatal sepsis but it lacks timeliness to influence initiation of antibiotic therapy. Thus newer rapid diagnostic markers like CRP and PCT help in early diagnosis of neonatal sepsis. In this study both CRP and PCT tests showed 100% sensitivity but Procalcitonin ELISA test showed higher specificity (67.39%) as compared to C-reactive protein test which has specificity (50%) and should thus be incorporated routinely for early diagnosis of neonatal sepsis.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home