|
Table of Content Volume 16 Issue 1 - October 2020
A study of incidence of pulmonary tuberculosis in chronic asthmatic patients
Adchitre Hitesh Ramesh1, D B More2*, Megha Jaraje3
1Post Associate Professor, Department of Microbiology} {2Associate Professor, Department of Chest} {3Medical Officer, RNTCP} SBH Government Medical College, Dhule, Maharashtra, INDIA. Email: dbmore62@gmail.com
Abstract Background: Chronic obstructive pulmonary disease (COPD) and tuberculosis (TB) are two important causes of mortality and morbidity in our country. Asthma is most commonly observed COPD in the developing countries. Aim and objective: To study the incidence of Pulmonary Tuberculosis in chronic Asthmatic patients at a tertiary health care centre Methodology: Present study was a prospective study carried out on 150 asthmatic patients who were taking treatment for more than 5 years. Data was collected with pre tested questionnaire. Data included demographic data, clinical history and clinical examination. All the patients were subjected to chest x-ray, sputum examination for acid fast bacilli by Zeil nelson stain. Data was analysed with appropriate statistical tests. Results: Mean age of the patients was 38.5± 3.1 years. Male to female ratio was 1.73:1. Majority of the patients (40.67%) belonged to lower middle class followed by upper lower class (28%). The incidence of pulmonary tuberculosis in our study was 4%. Patients with smoking habits, use of steroids developed pulmonary tuberculosis. Key Word: pulmonary tuberculosis.
INTRODUCTION Respiratory disorders like asthma, Bronchitis, Tuberculosis and pneumonia are major burden of disease in India. These diseases are mainly attributed with exposure to indoor pollution, solid-cooking fuels, poor housing, low nutritional status and sanitary conditions. The association of respiratory disorders with geographical region may be relevant with population density, industrial and textile pollutants, and tobacco consumption.1 India has the highest TB burden in the world accounting for 27% of the global cases with an estimated incidence of 2.74 million.2 India is the highest TB burden country in the world and hence is likely to harbor significant burden of TB-associated COPD. India has a growing population of COPD and is in second place for harboring the most number of morbidity and mortality cases from obstructive airway disease, after China.3 Various predisposing factors for tuberculosis include malnutrition, overcrowding, alcoholism, smoking and immune compromised states. Chronic obstructive pulmonary disease (COPD) affects 65 million people worldwide and is the third leading cause of death. Among these deaths, 90% deaths are in low- and middle-income countries which has maximum number of pulmonary tuberculosis (TB). The interrelationship between TB and COPD is very complex. A substantial number of TB patients develop post tubercular airway disease or TB-associated COPD. 4-7 Various studies were done in relation to TB and COPD. Different associations were published regarding TB and COPD. COPD is a common comorbidity in patients with TB. Patients with history of tuberculosis have increased frequency of exacerbations of COPD. COPD patients are also at high risk of developing pulmonary TB. COPD influences the clinical presentation of TB and is a risk factor for increased morbidity and mortality from TB.8-15 The use of steroids, physical and mental stress and poor socio economic status because of loss of wages due to asthma may predispose the patient to tuberculosis. Tobacco smoking is a major aetiological factor in the development of COPD. Several early studies supported an association between tobacco smoking and the tendency to develop TB. Use of steroids is also associated with development of TB in these patients due to immunosuppression. In asthmatic patients due to chronicity changes in the mucosa and lining epitheliam is often present. They are more prone to secondary bacterial infection which lead to exacerbation of asthmatic attacks. They are frequently treated with steroids and antibiotics this causes immunosuppression. Usually they respond to antibiotics but if they do not respond then sputum culture is advised and as per antibiotic sensitivity pattern antibiotics were given still if the patient doesn’t respond then other possibilities were taken into consideration. Most of the studies were carried out on TB associated COPD and patients developing COPD who are having tuberculosis. Very few studies have seen the development of tuberculosis in COPD patients. Asthma is most commonly prevalent COPD in our country so present study was aimed at finding incidence of tuberculosis in chronic asthmatic patients at a tertiary health care centre.
MATERIAL AND METHODS Present study was a prospective study carried out at tertiary health care centre. Study population was 150 asthmatic patients who were taking treatment for more than 5 years. Inclusion criteria: 1. Patients with history of asthma for more than five years and taking treatment Exclusion criteria: 1. Patients with history of asthma less than 5 years 2. Patients not willing to participate in the study. Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. Data was collected with pre tested questionnaire. Data included demographic data like age, sex and occupation. Detailed clinical history was taken from the patients. Clinical history related to duration of asthma, treatment taking for asthma, frequency of asthmatic attacks, past history of tuberculosis, family history of asthma was noted. A through clinical examination of the patients was done. All these patients were treated with antihistaminics steroids, antibiotics bronchodilators meter dose inhaler pumps on and off frequently. Routine investigations like complete blood count, renal and liver function tests were done. ESR is the main haematological investigation done but is found to be inconclusive as the patients are treated with steroids. All the patients were subjected to chest x-ray, sputum examination for acidfast bacilli by zeil nelson stain. Data was subjected to statistical analysis using Statistical package for social sciences (SPSS v 21.0, IBM). Descriptive statistics like frequencies and percentage for categorical data, Mean and SD for numerical data has been depicted.
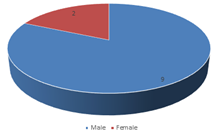
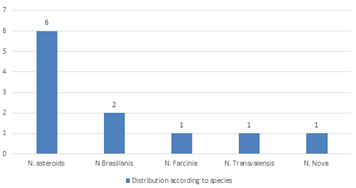
RESULTS Table 1 shows distribution of patients according to age group. Majority of the patients were from the age group of 31-40 years (30%) followed by 41-50 years (20.67%). Patients in the age group of 51-60 were 18.67%. 18-30 years age group patients contributed 17.33%. Patients above 60 years were 13.33 %. Mean age of the patients was 38.5± 3.1 years. Majority of the patients in our study were males 95(63.33%). Female population in our study was 55 (36.67%). Male to female ratio was 1.73:1. Socioeconomic status of the patient was determined by using Kuppuswamy scale of socioeconomic status. Majority of the patients (40.67%) belonged to lower middle class followed by upper lower class (28%). Patients in upper middle class were 14%. Patients in extremes of the class I.e upper class and lower lower class were 2% and 15.33% respectively. (table 2) In our study out of 150 patients 130 patients were outside workers and 20 females were housewife. In our study, we enquired about the smoking habit in the patients. Out of 150 patients, 80(53.33%) were non smokers. Current smokers were 40(26.67%). 20% of the patients have stopped smoking. Duration of smoking in current smoker ranges from 1-23 years. (table 3) All patients were treated with antihistaminics, steroids, antibiotics bronchodilators meter dose inhaler pumps on and off frequently. Majority of the patients used inhaled steroids 60(40%) followed by bronchodilators 48 (32%). Pulmonary function test were done in 150 patients and results were in favour of obstructive lung pathology. All the patients were subjected to chest x-ray, sputum examination for acidfast bacilli by Zeil nelson stain. Fig 2 shows incidence of pulmonary tuberculosis in patients with chronic asthma (duration more than 5 years). Out of total 150 patients 6 patients were found positive for acidfast bacilli on ZN stain. Only TWO X-ray were suspecting koch’s out of 150 patients. Thus the incidence of pulmonary tuberculosis in our study was 4%. Among the positive patients one was female and 5 were male. Regarding the smoking habits, the female was non smoker. Among the remaining 5 patients 4 were current smokers with duration of smoking ranging from 2-17 years. One patient was past smoker, he left smoking 3 years back. Among the positive patients all were using inhaled steroids. Mean duration of use of inhaled steroid was 9.41± 2.7 years. Due to unavailability of AFB culture facility and Gene expert study we were not able to talk about MDR cases in this study. Table 1: Distribution of patients of chronic asthma according to age group
Table 2: Distribution of patients of chronic asthma according to Socioeconomic status
Figure 1: Distribution of patients of chronic asthma according to sex
Table 3: Distribution of patients of chronic asthma according to smoking habits
DISCUSSION In our study, Majority of the patients were from the age group of 31-40 years (30%) followed by 41-50 years (20.67%). Mean age of the patients was 38.5± 3.1 years. Similar to our study, Lee et al. observed the mean age of the COPD cases as 54.5 ± 22.9 years. 8 Majority of the patients in our study were males 95(63.33%). Female population in our study was 55 (36.67%). Male to female ratio was 1.73:1. Similar to our study Lee et al. observed a male–female ratio of 1.6:1. 8 We found that, majority of the patients (40.67%) belonged to lower middle class followed by upper lower class (28%). The relationships between socio-economic status and respiratory diseases like COPD, tuberculosis is proved in previous studies. 16 Out of total 150 patients 6 patients were found positive for acidfast bacilli on ZN stain. Thus the incidence of pulmonary tuberculosis in our study was 4%. In a study by Popescu et al., where in 90% of the patients, bronchial asthma developed after tuberculosis and 10% patients presented with bronchial asthma and subsequently developed pulmonary TB. 17 In our study, Out of 150 patients, 80(53.33%) were non smokers. Current smokers were 40(26.67%). 20% of the patients have stopped smoking. Duration of smoking in current smoker ranges from 1-23 years. Among the positive patients 4 were current smokers with duration of smoking ranging from 2-17 years. One patient was past smoker. Cigarette smoking also increases the risk of developing TB by 3–5 folds. 18-19 Smoking suppresses the innate and adaptive immune response with decreased levels of pro-inflammatory cytokines and circulating immunoglobulins and reduces the activity of alveolar macrophages, dendritic cells, and natural killer cells. 20-21 Majority of the patients used inhaled steroids 60(40%) followed by bronchodilators 48 (32%). Among the positive patients all were using inhaled steroids. Mean duration of use of inhaled steroid was 9.41± 2.7 years. In a study on patients with inhaled corticosteroids researches observed that Multivariate Cox regression showed ICS use was an independent risk factor for the occurrence of pulmonary TB in patients who had a normal chest radiograph. (hazard ratio, 9.079; 95% CI, 1.012-81.431; P = .049) 22 There are many mechanisms by which steroids can increase the risk of tuberculosis. Steroids have profound effects on the cellular immune response. Glucocorticoids inhibit the lymphokine effect and monocyte chemotaxis and also block Fc receptor binding and function . 23-25 Glucocorticoids decreases the number of peripheral blood monocytes as well as monocyte functions it leads to decreased bactericidal activity and production of interleukin-1 and TNF-α. 26 Glucocorticoids also inhibit T cell activation, leading to reduced proliferative responses and cytokine production, and they also induce a redistribution of lymphocytes (predominantly T cells) out of the circulation, leading to peripheral lymphocytopenia. 27 These various effects of glucocorticoids on the cellular immune system may play a significant role in predisposing to tuberculosis infection.
CONCLUSION All chronic ashamatic patients should be screened for AFB by Zn stain.
REFERENCES
Fauci AS, Dale DC, Balow JE. Glucocorticosteroid therapy: mechanisms of action and clinical considerations. Ann Intern Med 1976;84:304.
Policy for Articles with Open Access
|
|
 Home
Home