|
Table of Content Volume 16 Issue 2 - November 2020
Virulence factors and antibiogram of Escherichia coli - The causative agent of urinary tract infection among pregnant women of Bidar district
Sudheendra Kulkarni1*, Chandrakanth Chillarge2
1Assistant Professor, 2Professor and HOD, Department of Microbiology, Bidar Institute of Medical Sciences, Bidar 585401,Karnataka, INDIA. Email: sudheekulkarni86@gmail.com
Abstract Background: Urinary tract infection (UTI) due to Escherichia coli (E. coli) is reported frequently among pregnant women. Understanding and analysing the disease in this section of population is more vital because UTI may cause complications in pregnancy. Uropathogenic Escherichia coli strains have been documented to encode a horde of virulence factors. These factors aid the bacteria in colonizing the urinary tract and assist the bacteria in persevering against the highly effective host defence. Such a mechanism could lead to the emergence of drug resistance. Aims:This study was aimed to investigate UTI among pregnant women due to E. coli, to know its antimicrobial drug susceptibility pattern and correlate antibiogram with phenotypic virulence factors. Settings and Design: The participants for the study were pregnant women. These women were enlisted from among those attending an antenatal care (ANC) clinic of a teaching hospital in north-eastern Karnataka. Methods and material: One hundred fifty mid-stream urine samples were processed for culture and antimicrobial drug susceptibility testing. Extended-spectrum beta-lactamases (ESBL) production and detection of virulence factors like biofilm and haemolysin by E. coli was performed. Results: E. coli could be isolated from 61 samples. Of these, 39 isolates showed in vitro biofilm formation. Haemolysin production was seen in 25 isolates and 49.18% of the isolates were positive for ESBL detection. Biofilm forming isolates showed highest resistance to the antibiotic Ampicillin, followed by Amoxicillin clavulanic acid, Cefuroxime and Ceftriaxone with significant p value. Conclusion: Significant correlation between virulence factors of E. coli and its antibiogram was seen. It is strongly recommended to undertake routine urine culture in pregnancy to know the virulence factors and antibiogram pattern to provide appropriate treatment to reduce complications. Key Words: Antibiotic resistance, ANC, Biofilm, UTI, Uropathogenic E. coli, Virulence factors.
INTRODUCTION Urinary tract infection (UTI) is the foremost bacterial infections among pregnant women along with other disorders such as anaemia and hypertension. Investigating and understanding the role of these infections is of high priority because UTI has been reported to cause complications such as pyelonephritis, chronic renal failure, premature delivery and foetal mortality. The fundamental reason for pregnant women being more prone to both symptomatic and asymptomatic UTI is because of the physiologic modifications associated with pregnancy. During pregnancy, women tend to have shorter urethra and a distended pregnant belly. In addition, pressure of the gravid uterus causes stasis of urine flow. These morphological changes impede proper maintenance of hygiene and normal urine flow, thereby making UTIs more prone among this population.1 UTI occurs approximately in 5-10 % of all pregnancies.2,3 It is well known and documented that pregnant women are more susceptible to develop recurrent UTIs1 and if not treated, increase the frequency of premature delivery and neonates with low birth weight.4 Screening for UTI must be scheduled along with the other standard tests and scans for pregnant women. Such measures could help identify UTI quickly so that appropriate therapy may be initiated. These measures help in controlling the associated complications.5 Therefore pregnant women should have a routine urine test in pregnancy and a repeat urine culture should be done in the third trimester to avoid complications. If left untreated, it may develop into acute cystitis or pyelonephritis.6 UTI in pregnancy is caused by the same organisms which are responsible for UTI in non-pregnant women. UTI is caused by several gram-negative bacilli. Among these, Escherichia coli (E. coli) is responsible for 80-90% of the infections.7 Staphylococcus saprophyticus, Klebsiella pneumoniae, Proteus mirabilis and group B Streptococci are some of the other common pathogens of the urinary tract. UTI continues to persist in several women regardless of positive antimicrobial therapy. It is known to recur despite treatment with a broad array of prescriptions. Recurrent and relapse of UTIs may be attributed to the presence of bacterial virulence factors. The uropathogenic E. coli (UPEC) display several of these factors, which have been demonstrated to play an important role in pathogenesis and cause significant antimicrobial resistance.8 The importance of these factors is accredited to the fact that they facilitate colonization of the bacteria by assisting the organism overcome host defences, thereby infesting the urinary tract. Virulence factors of UPEC develop multi-drug resistant. Apart from these, antimicrobial resistance may develop on account of abuse of broad-spectrum antibiotics. Among the various identified virulence factors, the most significant are adhesins or fimbriae, which cause biofilm formation, and haemolysin, which produces toxin. Biofilm is a production of an extracellular polymeric substance and formation of multicellular bacterial communities in which cells stick to each other and often also to a surface. Biofilms are responsible for reversible and irreversible binding to surfaces or to the objects and are commonly found in persistent and chronic human infections. [9] In the urinary tract, biofilm has been noted to develop on catheters and epithelial cells.10,11 This is a matter of concern because, in a biofilm, bacteria are more resilient to antimicrobial agents in contrast to planktonic bacteria.12 In addition, UPEC strains secrete and express a toxin called haemolysin. The presence of this toxin enhances the virulence of UPEC strains. Haemolysin has potent pro-inflammatory attributes. This feature results in the discharge of IL-6 and chemo-toxins, which generally establish the pathogenesis of renal diseases. Haemolysin has been observed to be associated with severe forms of the infection.13 The toxicity of haemolysis is determined by its capability of producing a clear zone in blood agar around or beneath the bacterial colonies, thereby destroying 5 per cent sheep erythrocytes following overnight incubation. 14 During pregnancy, oral antibiotics are the popular treatment of choice for symptomatic and asymptomatic bacteriuria and cystitis. Antimicrobial agents deemed safe in pregnancy are Nitrofurantoin, β-lactam antibiotics, penicillins and cephalosporins. [13] However, the option for antimicrobials is restricted. This is primarily because several of the drugs develop resistance. In addition, E. coli produces Extended Spectrum Beta-Lactamases (ESBL), which have been noted to be correlated with Multi-drug resistance (MDR). All these reasons limit the choice of antibacterials, with the issue being further problematic in the presence of MDR.15,16,17 Therefore, clinicians need to have a better understanding regarding the prevalence rates of UTI in their geographic region, comprehending the local antibiotic resistance pattern of E. coli. In addition, they need to continually evaluate the capability of the drugs used in treatment. This ensures that medication for UTI is effective, thereby eliminating probable complications. The incidence of UTI among pregnant women of Bidar district of Northern Karnataka is not familiar and no studies have been conducted so far in this region to compare the phenotypic expression of virulence factors in E. coli and antibiogram from pregnant women under antenatal care (ANC). Consequently, the prevalence rate of UTI due to E. coli was determined among pregnant women. In addition, the study endeavoured to recognise the prevailing phenotypic virulence factors, as well as antibiotic sensitivity pattern. Finally, the association between virulence factors and antibiogram of E. coli isolated was established.
MATERIALS AND METHODS Study population and sample collection: This prospective study was conducted at the Microbiology laboratory, Bidar Institute of Medical sciences (BRIMS) Bidar. Participants were recruited from among pregnant women attending ANC clinic of BRIMS Teaching hospital after taking informed consent. Mid-stream urine samples were obtained in a sterile wide-mouth container. A total of 150 samples were collected. The following data was also gathered from the participants: maternal age, gravidity and residence. The collected samples were directly transported the laboratory. Bacteriological analysis of the urine samples: The samples were processed for culture and antimicrobial drug susceptibility tests following routine microbiological techniques. Semi quantitative urine culture using a calibrated loop was performed to isolate bacterial pathogens on Blood and MacConkey’s agar as per the recommendations of Kass. [18] The culture plates were incubated at 37°C for 24 hours. The negative (growth) culture plates were incubated for an additional 48 hrs. Bacterial strains were isolated from the cultures and identified using standard biochemical tests. UTI was diagnosed on the basis of pathogens being present at least 105 colony forming unit (CFU)/ml of urine. However, the study dealt with only the E. coli isolates present. Antibiotic sensitivity testing: Antibiotic sensitivity testing was performed according to Kirby Bauer’s disc diffusion method on Mueller Hinton agar. CLSI guidelines were followed during the experimentation. [19],[20] Sensitivity was tested against the following antibiotics: Ampicillin (AMP 10mcg), Amikacin (AK 30 mcg), Amoxicillin-clavulanic acid (AMC 30 mcg), Cefriaxone (CTR 30 mcg), Cefuroxime (CXM 30mcg), Ciprofloxacin (CIP 5mcg), Gentamicin (GEN 10mcg), Imipenem (IPM 10mcg), Nitrofurantoin (NIT 300mcg), Norfloxacin (NX 10mcg), and Piperacillin-tazobactam (PIT 100/10 mcg) (HiMedia Laboratories, Mumbai, India). Statistical analysis Statistical software package SPSS version 22 (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.) was used to analyse the data. Unpaired t test was applied to calculate significance differences of resistance among biofilm producing and non-biofilm producing isolates. P-value ˂0.05 was considered statistically significant.OBSERVATIONS AND RESULTS Prevalence of UTI and patients profile: Among 150 samples tested, E. coli could be isolated from 61 samples with colony count of 105 CFU/ml of urine and a prevalence rate of 40.66% (Table 1). The majority of pregnant women were in their 2nd and 3rd trimester (1st trimester- 6.2%, 2nd -14.53%, 3rd - 22.6%). The mean age of the participants was 24 years. Most of the urine samples were obtained from pregnant women in the age range of 18 to 23 years (55.73%; 43 in number). Pregnant women in the age range of 27 to 29 years contributed to the least number of samples (3.27%; 26 in number) (Table 2). The rate of infection was high among the participants in the age group of 18-23 years. Among those infected, 69.2% were from the urban locality and 30.76% from rural areas. Most of them attended ANC unit on need basis and not regularly.
Table 1: Prevalence of E. coli
Table 2: Percentage distribution of E. coli isolated from pregnant women according to age
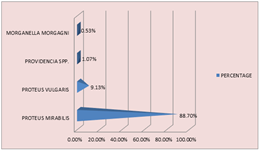
Virulence characters of UPEC Isolates: The incidence of in vitro biofilm formation by E. coli was 63.93%. Of the 61 isolates, biofilm formation was detected in 39 isolates by all the three methods for biofilm detection. 32.30% isolates showed biofilm formation by Tube method, 53.84% by CRA method and 27.69% by TCP method. Haemolysin production was seen in 25 isolates (40.98%) and 49.18% of the isolates were positive for ESBL detection. Figure 1 Figure 2 Figure 3 Figure 1: Positive biofilm formation; Figure 2: Biofilm formation on Congo red agar by tube adherence method; Figure 3: Positive biofilm formation by Tissue culture plate method.
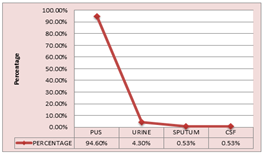
Antimicrobial profile of the isolates: All isolates showed the highest resistance to the antibiotic Ampicillin (96.72%), followed by Amoxicillin- clavulanic acid (62.29%), Cefuroxime (55.73%) and Ceftriaxone (54.09%). E. coli isolates which formed biofilm displayed a significant increase in the resistance pattern to all the antibiotics and proved to be statistically significant. Table 3 displays the multi-drug resistant pattern of the UPEC E. coli. Details included are for both the biofilm producing and non-producing bacteria. The data clearly shows similarity in the sensitivity pattern of all the E. coli isolates. The isolates were sensitive to broad spectrum antibiotics like Imipenem (100%), Piperacillin-tazobactam (93.44%), Nitrofurantoin (90.16%), and to the drugs Chloramphenicol and Gentamicin (83.60%). Further, unpaired t test analysis indicated that the difference in the resistance pattern of biofilm and non-biofilm forming isolates against the 11 different antibiotics which were tested was statistically significant (p <0.031)Table 3: Antibiotic susceptibility pattern of the biofilm producing and non-producing Uropathogenic E. coli
* Significant at p< 0.05. R= Resistant S= Sensitive.
DISCUSSION Urinary tract infection (UTI) is the foremost bacterial infections among pregnant women.25 During pregnancy, women tend to have shorter urethra. This results in colonization of the peri-urethral area by pathogens that ascend from the gastro-intestinal tract and colonize the urinary bladder or kidneys.26 Pregnant women are more prone to UTI than non-pregnant women. The fundamental differences in the prevalence of UTI among the pregnant population is based on the following factors: age, parity, gestation age and level of education.27 The primary causative organisms for UTI in pregnant women are gram-positive and gram-negative bacteria, as well as yeast. Our study was designed to understand the prevalence rate of UTI due to E. coli among pregnant women of Bidar district. In addition, the virulence characteristics and antibiotic profile were investigated. Our study revealed a higher incidence rate (43.33%) of UTI among females in the second and third trimester of pregnancy. According to our results, the prevalence of UTI is high in north Karnataka region as compared to other parts of Karnataka with commonest isolated pathogen as E. coli.28 Annie Rajaratnam et al... conducted a similar study in coastal Karnataka and recorded an overall low prevalence of 13.2%.29 Our study revealed the highest infection rate of UTI in pregnant women and among the age group of 20-25 years, in agreement with the findings documented by Kasinathan A, Thirumal and Chandel, Lata R., et al.30,31 In this region, phenotypic traits of UPEC isolates are not well known. In addition, the association of these traits with antibiotic resistance patterns needs to be determined among the pregnant women with UTI Furthermore, no documented studies are available. The effectiveness of antibiotic treatment depends on the analysis of virulence factors and antimicrobial resistance pattern of uropathogens responsible for UTI. Antimicrobial prophylaxis for women with recurrent UTI includes β-lactam drugs and Cephalosporins. Since there is emergence of drug resistance in UTI, we aimed to study the sensitivity pattern of E. coli, which is the predominant pathogen causing UTI. When the microbes were tested against various antimicrobials to determine their susceptibility, isolates showed high resistance to the β-lactam group of antimicrobials. This fact is a matter of concern because this group of drugs is traditionally used in UTI therapy. Similar accounts of resistance to the extended spectrum of β-lactamases among the general population infected with urinary pathogens have been reported.32,33 In our study, we found significant correlation between the virulence factor biofilm and antibiotic resistance. Biofilm forming UPEC isolates showed maximum resistance to the antibiotics than non-biofilm producers. Isolates showed increased resistance to the drugs Ampicillin, Cefuroxime, Ceftriaxone, Ciprofloxacin and Aminopenicillins, which are considered to be safe in pregnancy and are the commonly used antibiotics to treat UTI. Similar findings were reported in a study performed by Tajbakhsh, Elahe, et al.. in Iran.34 Among other antibiotics, carbapenems such as Imipenem is the most competent against all UPEC strains (100%), especially for the extended-spectrum beta lactamase (ESBL) strains. 35 The other proven proficient antibiotics include Nitrofurantoin (97.43%), Piperacillin–tazobactem (94.87%), Amikacin (87.17%) and Gentamicin (84.61%). UPEC strains were moderately susceptible to Norfloxacin. Studies by ME Terlizzi et al... and Chakraborty et al... concur to these finding. Their work consented to a significant correlation between virulence factors and antimicrobial resistance. In addition, they showed a high resistance of the isolates to the antibiotics generally used in UTI therapy.36,37] Screening for antimicrobial sensitivity must be scheduled along with the other standard tests and scans for pregnant women. Such measures could help prescribe safe and effective drugs so that appropriate therapy may be initiated. These measures help in controlling the associated complications. Prescribing antibiotics for UTI treatment without bacterial characterization could trigger enhanced resistance among uropathogens. In addition, it restricts the choice of drugs available for the treatment of UTI. Hence, our study showed that the drugs Imipenem, Nitrofurantoin, and PIT are recommended for the treatment of suspected UTI among pregnant women. In our study’s setting, these drugs would help avoid further complications.
CONCLUSION The association between virulence factors and antibiogram was perceived in our study. Hence, screening for virulence factors and antimicrobial sensitivity must be scheduled along with the other standard tests for pregnant women. In addition, routine urine cultures would help in timely detection of UTI. Such measures could help prescribe safe and effective drugs so that appropriate therapy may be initiated. Further, periodic studies are recommended, especially among the pregnant population, to screen changes in the susceptibility pattern of UPEC. Our study assists in understanding the local antibiotic resistance rate and virulence pattern of E. coli, which a clinician needs take into consideration when deciding on therapy.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home