|
Table of Content - Volume 17 Issue 2- February 2021
Changing trends of antimicrobial susceptibility pattern of salmonella typhi isolates in a tertiary care hospital, Ahmedabad
Rosy Parmar1, Palak Rao2*, Sachin Patel3, Parul Patel4
1,2,3,4M.D, Department of Microbiology, GMERS Medical College, Sola, Ahmedabad, Gujrat, INDIA. Email: palakbhatia99@yahoo.com
Abstract Background: Enteric fever is endemic in India caused by Salmonella typhi and Paratyphi strains. Though Antibiotic therapy is available for its treatment, resistance to commonly used antimicrobials poses a very big hindrance in proper treatment. So this study aims to observe the changing trends in antimicrobial resistance pattern of Salmonella typhi isolates over a duration of five years to help in standardizing treatment protocols for enteric fever. Materials and Methods:All blood culture samples received in Dept. of Microbiology, GMERS Medical College and Hospital Sola, over the duration of five years i.e from January 2015 to December 2019 were included in the study. All blood cultures were processed by Automated blood culture system and in those Salmonella typhi was isolated, antimicrobial susceptibility testing was done as per CLSI guidelines for Ampicillin, Chloramphenicol, Cotrimoxazole, Ciprofloxacin, Levofloxacin and Ceftriaxone. Results: It was seen that there was an increase in resistance to fluoroquinolones every year and surprisingly the first line drugs i.e Ampicillin, Chloramphenicol and Cotrimoxazole were found sensitive in most of the cases. Ceftriaxone resistance was also seen in only one isolate. Conclusion: Increasing resistance to fluoroquinolones suggests to limit its use and reintroduce first line medication in treatment of enteric fever. Also periodic study of antimicrobial resistant pattern of Salmonella isolates is must to rationalize treatment protocols and prevent emergence of resistance to newer antimicrobials. Key words: Salmonella, resistance, treatment
INTRODUCTION Enteric fever or Typhoid fever is endemic in India caused by Salmonella typhi and paratyphi strains. These pathogens are transmitted by oral route, through contaminated food or water.1,2 Typhoid fever remains an important public health problem in developing countries with majority of population belonging to low socioeconomic status and living under conditions of limited resources and constrained sanitation infrastructure. Typhoid fever has been estimated to cause 13000-220000 deaths each year in Asia as per recent study which is significant number , so proper treatment is a need.3 Antibiotic therapy remains the mainstay of treatment for enteric fever. However, it depends on susceptibility of strains. After emergence of Multidrug resistant Salmonella typhi (i.e resistant to Chloramphenicol, Ampicillin and cotrimoxazole) in 1980’s, fluoroquinolones became the drug of choice. In 1990’s due to increased use of fluoroquinolones to treat MDR strains, reduced susceptibility of ciprofloxacin was seen in India, other regions of southern Asia and Sub-saharan Africa. Resistance to ceftriaxone has also been reported recently. Interestingly, it is noticed that many strains reverted susceptible to the olden day drugs as they were not in use for long time.2,4 The present study was carried out to observe the changing trends of antimicrobial susceptibility pattern of Salmonella typhi isolated from blood culture samples in a tertiary care hospital, Ahmedabad during the period of five years (2015 to 2019).
MATERIALS AND METHODS This study was conducted in Department of Microbiology over a span of five years in a tertiary care hospital of Ahmedabad. All Blood culture samples received in the laboratory from January-2015 to December-2019 were included in the study. All samples were processed by automated blood culture system-BACTEC-9050(Becton Dickinson). The positive blood culture samples were cultured on Nutrient Agar, Mac Conkey Agar and Sheep Blood Agar. Identification of Salmonella typhi was done by conventional methods and was confirmed by using Salmonella sp. Polyvalent ‘O’ and “O9” antisera (5). Antimicrobial susceptibility testing was done by Kirby- Bauer Disk Diffusion method using antibiotic discs for Ampicillin (10µg), Chloramphenicol (30 µg), Ciprofloxacin (5 µg), Cotrimoxazole (1.25/23.75µg) and Ceftriaxone (30 µg). Minimum Inhibitory Concentration was determined by E-test method for Levofloxacin. This was done as per CLSI guidelines for the respective year(6,7,8,9,10). All media and Antibiotic discs were procured from Hi media, Ahmedabad.
RESULTS In this five year duration i.e form 2015 to 2019, total 5778 blood culture samples were received in the Dept. of Microbiology. Of these samples, 1448 (25%) blood culture samples were positive. From the various isolates, Salmonella typhi was isolated from 143 samples. An increasing prevalence of Salmonella typhi was observed in five years. Total 15,21,22,31 and 54 S.typhi were isolated in the year 2015,2016,2017,2018 and 2019 respectively. (Fig:1)
Figure 1: Salmonella typhi isolates from Blood culture year wise The antimicrobial resistance pattern of S.typhi isolates to the Antimicrobials tested as per CLSI guidelines year-wise was as follows( Table:1): Table 1: Antimicrobial resistance patter year wise
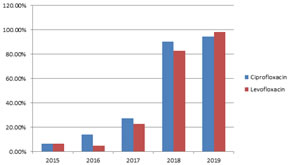
This shows there was a sudden peak seen in resistance to Fluoroquinolones in the year 2018 and 2019. The resistance to Ampicillin, Cotimoxazole and chloramphenicol was seen in very few isolates and Ceftriaxone resistance was seen only in one isolate. Fig: 2 here shows us the trends of Fluoroquinolone resistance in Salmonella typhi isolates.
Figure 2: Trend of Fluoroquinolone resistance
DISCUSSION Enteric fever is a growing concern in developing countries like India. The variation in the antibiotic susceptibility pattern as seen in our study is really a matter of concern. In our study, The Multidrug Resistance (i.e resistance to Ampicillin, Chloramphenicol and cotrimoxazole) was seen only 2% of Salmonella typhi isolates which is very less compared to the previous years. This was also seen in one study conducted at Banaras Hindu University in the year 2011-2013. They also found decrease in Multi-drug resistant Salmonella typhi isolates from 79.6% in 1980-1998 to 24.6% in 2011-2013. It was also observed that there was a surge in fluoroquinolone resistance in the last two years of study. It rose from 6-7% in 2015 to 80-90% in 2019. This finding was comparable to the other studies as shown in Table 2.
Table 2: Comparison with other studies regarding Fluoroquinolone resistance
This suggests that as seen in our study, similar trend of increasing resistant to fluoroquinolones was also seen in other studies conducted at different centers. This increasing resistance to fluoroquinolones observed in present study is most probably due to indiscriminate use for enteric fever as well as for other infections. It is also associated with re-emergence of susceptibility to the first line drugs previously used like Ampicillin, Cotrimoxazole and Chloramphenicol due to their restricted use.2,11,12,13 Now in current situation, third generation cephalosporins have now become the drug of choice for treatment of enteric fever. Though in our study, resistance to Cephalosporin was seen in negligible amount, some studies have reported increasing MICs of third generation cephalosporins also4,14, 15,16. On the basis of above observations, it may be suggested that the conventional drugs which have shown very low resistance in Salmonella typhi isolates should also be prescribed, so that we can prevent resistance to third generation cephalosporins due to its excessive use. Also, we can hope for re-emergence of sensitivity to fluoroquinolones if its use is limited.
CONCLUSION Our study showed the changing trend of antibiotic susceptibility of Salmonella typhi isolates in the period of five years which is expected to change time to time. So, it is a necessity that continuous surveillance of antibiograms of Salmonella isolates should be done to rationalize enteric fever treatment protocols and to prevent further emergence of resistance to the newer drugs. Acknowledgement We would like to acknowledge our staff members and head of the department for their support. REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home `
`