|
Table of Content Volume 17 Issue 3 - March 2021
A case report of tubular duplication of descending colon in an adult
M D Abdul Salam Baba1*, K Venkat Ram Reddy2, G Rama Krishna Reddy3
1Junior Resident, 2Professor & HOD, 3Professor, Department of Radiodiagnosis, SVS Medical College and Hospital, Mahabubnagar, Telangana, INDIA. Email: shoebsalaam123@gmail.com
Abstract Background: Alimentary tract duplications are uncommon congenital anomalies that usually present during the first decade of life. Tubular duplication of colon is very rare and very difficult to diagnose preoperatively1. Knowledge of the spectrum of abdominal radiographs and CT features of tubular colonic duplication is important in making the correct diagnosis and potentially preventing the complications. Only a few cases have been reported in the literature1,2,3,. We report a case of 30-year-old male presenting with long history of chronic constipation, abdominal mass and repeated episodes of abdominal pain. The abdominopelvic CT scan showed segmental bowel wall thickening, dilatation and with stasis of intraluminal content. The provisional diagnosis were large colonic diverticulum/Trichobezoar. He was scheduled for exploratory laparotomy. However, 'T' shaped tubular colonic duplication of descending colon with impacted faecaloma was found intraoperatively. Keywords: Tubular duplication of colon, CT scan, Abdominal radiographs.
INTRODUCTION Gastrointestinal tract duplication is a rare congenital anomaly that can occur anywhere along the alimentary tract. Approximately 80% of duplications occur in the abdomen, with others occurring in the chest5. For digestive duplications, the ileum is the most common site (30%–35%) and the colon is the least common site (7%–20%)2,3. The duplication can widely vary in size and shape; it is cystic in more than 80% of patients and tubular in the rest7.Gastrointestinal tract duplication usually manifests during the neonatal period or childhood; most patients (67%–80%) are diagnosed before the age of 2 years2,3. CASE REPORT A 30-year-old male presenting with long history of chronic constipation since 2 years, abdominal pain since 10 days which was intermittent and colicky type. There was no history of fever, bloody stools, burning micturition. All routine investigations were within normal limits. Physical examination revealed a non tender soft mass in the right hypochondrial region. PLAIN ABDOMINAL FILM
FIGURE 1: Showing a large smooth walled, gas-filled, oval shaped radio-opaque mass in the right lower abdomen
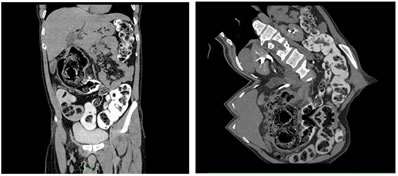
USG ABDOMEN: There were focal dilated bowel loops, with intraluminal contents and inflamed walls in right hypochondrium and right hypogastric region with no peristalsis. Other adjacent bowel loops were normal. CECT ABDOMEN: There was gas filled segmental dilatation with stasis of intraluminal contents with thickened walls and adjacent fat strandings, which was showing communication with the colon. The operative findings were concluded as a duplication part of descending colon. Then retrospectively coronal and sagittal multi planar reformatted (MPR) images were reconstructed which was showing large dilated structure having communication with the descending colon and receiving blood supply from the branches of inferior mesenteric artery (left colic artery).
Figure 2a: Oblique coronal mip image showing large blind end dilated bowel loop filled with faecal matter and directed toward right upper quadrant of abdomen; 2b: Oblique reformatted image showing T – Shaped duplicated colonic segment having communication with distal part of descending colo
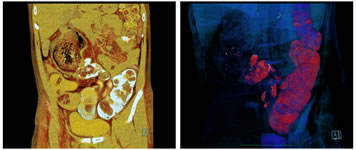
Figure 3D VRT images showing: 3a, 3b: 3D VRT images showing large T – Shaped duplicated colonic segment with impacted faecoloma
Figure 4: 3D VRT Images: 4a: Anterior view, 4b: Posterior view – Showing large T – Shaped duplicated colonic segment with impacted faecoloma having communication with distal descending colon.
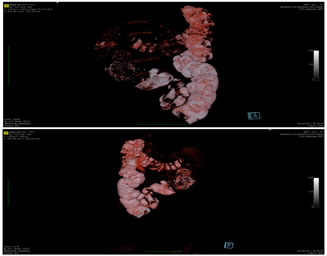
OPERATIVE FINDINGS Under general anaesthesia, exploratory laparotomy was performed showing a firm to hard, encapsulated mass of impacted faeces in retroperitoneal region, medial to distal part of ascending colon (hepatic flexure). The capsule was opened and hard faecal mass of size 8 x 5 cm was extracted. When the fibrous capsule was explored, lower end of the capsule was continuous with the tubular structure which was traced retroperitoneally and retromesenterically and was connecting with the distal part of descending colon. The tubular structure had mucosal folds similar to the colonic mucosal folds and since it was continuous with the descending colon, it was concluded as a duplicated part of descending colon. Segmental resection of descending colon including the duplicated part and end to end anastomosis was performed.
Figure 5: Grossly the duplicated segment measuring approximately 30 cm in length was connected to the native distal descending colon
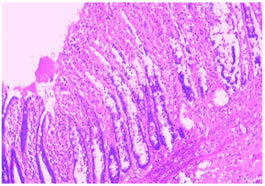
HISTOPATHOLOGY REPORT: Specimen was sent for histo-pathological study, which suggested a nonspecific colitis and ischaemic necrosis of colonic segment.
Figure 6: Microscopically, the duplication segment showing all 4 layers of the bowel wall with non specific colitis and ischemic necrosis of the segment
DISCUSSION Alimentary tract duplications are rare congenital lesions normally diagnosed in newborns and children (although in adulthood it occurs with the same frequency). They can occur anywhere from the mouth to the anus with a reported incidence of approximately 1 in 4500 live births2,3. They are rare anomalies, detected in 1 of every 4,500 autopsies, and a study in the largest number of cases analyzed 96 infants and children with 101 gastrointestinal (GI) duplications7. The most common site of GI duplication is the ileum (30%), followed by the ileocecal junctioin (30%), jejunum (8%), colon (6%–7%), and rectum (5%)4. The anatomical types of GI duplications include the cystic type (90%) and the tubular type (10%). The tubular type includes the double-barreled type (80%) and the Y- or T-shaped type (20%)8. Therefore, tubular colonic duplications in adults are very rare, and in our literature review, only 17 cases have been reported. Tubular and Y-shaped total colonic duplications in adults are extremely rare1,6, and we have not found any other cases. The clinical presentations are related to the location and size of the duplication, the presence of gastric mucosa or pancreatic tissue, and the anatomical type such as cystic or tubular type9. These anomalies are frequently encountered during laparotomy for other expected common diseases such as intussusception, appendicitis, GI bleeding, intestinal perforation and obstruction. Therefore, more than 67% of GI duplications are diagnosed within the first year of life9. However, if GI duplication is not accompanied by other anomalies such as imperforated anus, perineal abscess, and genitourinary malformation, it is occasionally diagnosed in adulthood because of silent symptoms4. Tubular type of colonic duplication has only one connection with the native bowel, and the other side is usually formed by blind ending pouch, or perianal and genitourinary fistula, and imperforated anus1. In this case, colonic duplication was noted with a blunt end. Because the distal end of the colonic duplication was too narrow to pass feces adequately for decades, it was asymptomatic for many years. GI tract duplications including colonic duplications are difficult to diagnose preoperatively regardless of their location. A radiologic study including a plain abdominal film, ultrasonography and CT can be helpful in detecting the cystic lesion of colonic duplication10. Technetium-99m scintigraphy can be used to detect heterotopic gastric mucosa in cases of bleeding9. Colonoscopy is a very useful diagnostic tool for double-barreled type and cystic type of colonic duplication1. However, in case of tubular type, it may not be diagnostic because in such cases, the distal orifice of the duplicated colon is very small or absent and it may appear similar to the diverticulum.
CONCLUSION Colonic duplication is a rare congenital anomaly that is usually diagnosed and treated during childhood. Some adults can harbour a silent duplication for many years until complications occur. The clinical presentation can include abdominal pain, an abdominal mass, bowel obstruction and diarrhoea. It is difficult to make the preoperative diagnosis of colonic duplication because of its rarity and differential symptomatology, awareness of its imaging features is significant. Plain radiography remains a useful tool for first line investigation due to its simplicity and widespread availability whereas CECT provides a definitive diagnosis.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Radiology (Print ISSN: 2579-0927) (Online ISSN: 2636-4689) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
Height, IVDL-Intervertebral Disc Length
Policy for Articles with Open Access
Authors who publish with MedPulse International Journal of Radiology(Print ISSN: 2579-0927) (Online ISSN: 2636 - 4689) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. |
|
 Home
Home