|
Table of Content Volume 17 Issue 3 - March 2021
Dyke–Davidoff–Masson syndrome: A rare cause of cerebral hemiatrophy in children
Surendar Penumuri1, Venkata Ram Reddy Kuchukulla2*, Rajaneesh Borugadda3, Rama Krishna Reddy Gaddam4
1Junior Resident, 2Professor & HOD, 4Professor, Department of Radiodiagnosis, SVS Medical College and Hospital, Mahabubnagar, Telangana, INDIA. 3Senior Resident, Government Medical College and Hospital, Mahabubnagar, Telangana, INDIA. Email: nagababu00799@gmail.com
Abstract Background: Dyke–Davidoff–Masson syndrome (DDMS) is an uncommon condition, in which the diagnosis is mainly done by various clinical presentations along with positive radiological findings. In this syndrome there is hemiatrophy or hypoplasia of unilateral cerebral hemisphere resulting from brain insult in foetal or early childhood period. The important radiological imaging features are cerebral hemiatrophy, with ipsilateral thickening of calvarium, ipsilateral hyperpneumatization of paranasal air sinuses, elevation of petrous ridge and associated parenchymal changes. A 17 year old female presented to our institute with few episodes of seizures, mental retardation and contralateral (right side) hemiparesis. The patient was referred to the radiology department for further investigational work up with skull radiographs, computed tomography and magnetic resonance imaging of the brain. The findings noted were unilateral atrophy of the right cerebral hemisphere with ex - vacuo dilatation of ipsilateral lateral ventricle, ipsilateral sulcal prominence, ipsilateral compensatory hypertrophy of the skull vault and enlarged right frontal sinus which suggest the diagnosis of DDMS. Key words: Cerebral hemiatrophy, Dyke–Davidoff–Masson syndrome, hemiparesis.
INTRODUCTION In 1933 Dyke-Davidson-Myke described plain skull radiographic and pnuematoencephalographic changes in a series of nine patients characterized by hemiparesis, mental retardation, facial asymmetry and seizures. DDMS is caused by cerebral insult that may occur in utero when the maturation of calvarium has not been completed or during early life due to brain damage (usually traumatic). The clinical findings may be of variable degree according to the extent of the brain injury1-3.
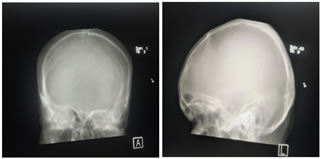
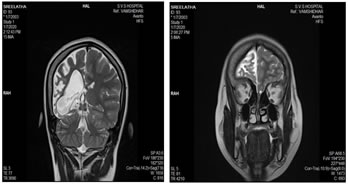
CASE REPORT A 17-year-old female child was brought for deteriorated mental status and a history of few episodes of left focal seizures with secondary generalization since 2½ years. There was no history of head trauma. The seizure episodes were followed by decreased movement of the left side of the body and occasionally drooling of saliva from the left side. Perinatal vs. birth history was uneventful. The patient did not attend school. On examination, the child was undernourished with very poor cognitive function. Vitals were normal. Positive clinical findings noted were – microcephaly, severe mental retardation with an intelligence quotient of 40 and left-sided facial palsy. Examination of the central nervous system revealed left hemiparesis. Examination of other systems was unremarkable. Radiographs of skull showed thickening of the right hemicalvarium [Figure 1]. Non-contrast computed tomography and magnetic resonance imaging (MRI) reveled unilateral atrophy of the right cerebral hemisphere and ex- vacuo dilatation of ipsilateral lateral ventricle with prominence of sulci [Figures 2 and 3]. Thickening of the right hemicalvarium was noted measuring 7-8 mm compared to 5 mm on the left side (in frontal region at level of lateral ventricles) and enlarged right frontal sinus. These findings were suggestive of DDMS.
Figure 1 Figure 2 Figure 3 Figure 1: Skull radiographs: Anterioposterior and lateral views showing thickening of the right hemicalvarium (asterisk *); Figure 2: Axial sections of non-contrast magnetic resonance imaging (T1) and computed tomography (brain window) of the brain showing diffuse atrophy of the right cerebral hemisphere with ex-vacuo dilatation of the right lateral ventricle and prominence of sulci over the right cerebral hemisphere. Compensatory thickening of the right hemicalvarium is also seen; Figure 3: Coronal (T2) Magnetic resonance imaging and axial computed tomography(bone window) of the brain showing diffuse atrophy of the right cerebral hemisphere with ex-vacuo dilatation of the right lateral ventricle and compensatory thickening of the right hemicalvarium
DISCUSSION The syndrome was first described by Dyke, Davidoff and Masson in 1933 on plain skull radiographs and pneumo-encephalograms in a series of nine patients. The clinical features depend on extent of brain injury and include hemiparesis or hemiplegia, seizures, mental retardation or learning disability, speech or language disorders and facial asymmetry. Rarely patients can also present with sensory symptoms and psychiatric disorders like schizophrenia. Nevertheless, seizures may appear months to years after the onset of hemiparesis and mental retardation is not seen in all cases2,3. It has been reported that DDMS is caused by cerebral insult that may occur in utero when the maturation of calvarium has not been completed, or during early life due to brain damage (usually traumatic)4. Prenatal causes include congenital abnormalities, cerebral infarction, vascular malformations, infections, and gestational vascular occlusion, primarily involving the middle cerebral vascular territory. Birth trauma, hypoxia, intracranial hemorrhage, tumors, infections, and prolonged febrile seizures after birth are important peri- and post-natal causes. It can also be due to decreased carotid artery blood flow due to coarctation of aorta. Cerebral atrophy in turn results due to reduction in the formation of brain derived neurotrophic factors by these causes5. There are two types of DDMS – congenital (infantile) and acquired6. In congenital hemiatrophy, when the insult occurs in utero, there is a shift of midline structures toward the side of the disease, and the sulcal prominence replacing the gliotic tissue is absent. This feature differentiates it from cerebral hemiatrophy which occurs in early life. The atrophied cerebral hemisphere will have prominent sulcal spaces if the insult occurs after birth or after the end of sulcation7. The clinical findings in DDMS may be of variable degree according to the extent of the brain injury: Seizures, facial asymmetry, contralateral hemiplegia or hemiparesis, mental retardation, and rarely, patients can also present with sensory symptoms and psychiatric disorders such as schizophrenia. The diagnosis is based on the typical radiological features on computed tomography (CT) and MRI scans which include cerebral hemiatrophy with dilated ipsilateral lateral ventricle. Also there is thickening of calvarium with enlargement of frontal, ethmoid and sphenoid sinuses and elevation of greater wing of sphenoid and petrous ridge. The osseous abnormalities can also be depicted on plain skull films5 ,7. When DDMS develops early in life (during the first 2 years), certain cranial changes such as ipsilateral hypertrophy of the skull and enlargement of sinuses occur, the elevations of the greater wing of sphenoid and the petrous ridge on the affected side and ipsilateral falcine displacement. The compensatory cranial changes occur to take up the relative vacuum created by the atrophied or hypoplastic cerebral hemisphere.8 Hageman et al. proposed the terms cerebral hemihypoplasia or unilateral cerebral hypoplasia for the primary (congenital) cerebral atrophy owing to the fact that there is a lack of cerebral development rather than atrophy9. An exhaustive clinical history and computed tomography (CT) or MRI gives the right diagnosis. In addition to CT findings described above, MRI demonstrates the gray-white matter loss with hyperintensities on T2-weighted images (diffuse cortical and subcortical atrophy) and asymmetry of the basal ganglia.7 MRI has the ability to reveal changes in the cerebral hemispheres as well as highlighting bony structures, thus differentiating between congenital and acquired types of DDMS8. Important differential diagnosis includes – Sturge–Weber Syndrome, basal cell germinoma, Fishman syndrome, Silver–Russell syndrome, linear nevus syndrome, and Rasmussen encephalitis. Rasmussen encephalitis does not show calvarial changes, and Sturge–Weber syndrome additionally shows enhancing pial angiomas and cortical calcifications10. The Management consists of control of seizures with appropriate anticonvulsants, as most patients with this disorder present with refractory seizures. Additionally, domiciliary physiotherapy, occupational and speech therapy have a crucial role. Hemispherectomy is indicated in patients with hemiplegia and intractable disabling seizures and is successful in 85% of the cases. Prognosis is poor in cases of prolonged or recurrent seizures and if hemiparesis occurs before two years of age. Hence, it is indeed very important for neurologists, paediatricians and radiologists to be familiar with this condition for its early diagnosis and treatment.10,11
ACKNOWLEDGEMENTS We are thankful to SVS medical collegeand hospital for their invaluable help and support.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Radiology (Print ISSN: 2579-0927) (Online ISSN: 2636-4689) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
Height, IVDL-Intervertebral Disc Length
Policy for Articles with Open Access
Authors who publish with MedPulse International Journal of Radiology(Print ISSN: 2579-0927) (Online ISSN: 2636 - 4689) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. |
|
 Home
Home