|
Table of Content - Volume 19 Issue 1 - July 2021
A comparative study of phenytoin dressing versus honey dressing in the treatment of cronic ulcers in tertiary care hospital
Sandesh M1*, Rithin Suvarna2
1,2Department of General Surgery, A.J institute of Medical Sciences, Kuntikan, Mangalore, INDIA. Email: sandytumkur76@gmail.com Abstract Background: Diabetic foot infections are the leading cause of hospitalization morbidity and mortality in diabetics worldwide In India it accounts for 20% of hospitalizations. honey has been investigated to treat ulcers like pressure ulcers, venous ulcers, diabetic ulcers, traumatic wounds and burns. Phenytoin is also now known to promote wound healing and can be an alternative to normal saline specifically in chronic wounds related to diabetes. The present study compares these two modalities in management of diabetic ulcers. Objective: To compare the efficacy of topical phenytoin vs topical honey in chronic diabetic ulcers in terms of rate of wound healing, granulation tissue formation and quality of graft bed for skin grafting. Methods: A comparative prospective study of 50 patients with chronic diabetic ulcers selected based on a predefined criteria divided into two groups: Group A (Phenytoin group) (n=25) and Group B (honey group) (n=25). Final wound area was measured on 30th day. Comparison between the wound size reduction among two groups done at end of 30th day. Outcome was measured in terms of wound reduction, granulation tissue formation and quality of bed for skin grafting between the two groups. Results: This study has shown faster rate of wound healing, better granulation tissue formation and quality graft bed for skin grafting in patients who received topical phenytoin dressing as compared to topical honey dressing. Key Words: Chronic Diabetic ulcer, topical phenytoin, topical honey
INTRODUCTION The problem of diabetes mellitus is a global one, worldwide diabetes mellitus affects more than 194 million people and the figure is expected to reach 333 million by the year 2025. India is the capital with the highest number of diabetic patients and is considered as the “diabetic capital of the world.” 1,2 With the maximum number of cases of diabetic foot in developing countries is due to staphylococcus aureus.3,4 Diabetic foot ulcer is one of the major complication of diabetes mellitus. It occurs in 15 percent of all patients with diabetes and precedes 84 percent of all lower leg amputations. 5 Diabetes mellitus impedes wound healing by prolonging the inflammatory phase. Increased glucose in the tissue precipitates infection. Diabetic microangiopathy which affects microcirculation. Increased glycosylated hemoglobin decreases the oxygen dissociation. Increased glycosylated tissue protein decreases the oxygen utilization. In recent years the technology of dressing has developed significantly, and several new products which reflect greater knowledge of tissue repair physiology have been produced and successfully used for the management of various types of chronic ulcers. However there is limited information to guide treatment of diabetic ulcers. It is well known that the basic cellular and molecular mechanisms that result in wound healing involve cell adhesion, migration, proliferation, differentiation, and apoptosis are impaired in diabetes mellitus. 6 Absolute or relative lack of insulin or insulin action is a hallmark of diabetes contributing to wound healing defects in diabetics.6,7 Insulin stimulates the growth and development of many cell types including keratinocytes, endothelial cells and fibroblasts. It also affects the proliferation, migration, and secretion of cytokines and chemokines by these cells. Wound healing is a complex biological process influenced by several agents such as insulin-like growth factor IGF and human acidic fibroblast growth factor. In vivo studies have shown that IGF can stimulate the proliferation and differentiation of endothelial cells and fibroblasts and promote granulation tissue regeneration to contribute to wound healing.6 Topical honey application appears to decrease bacterial growth by hydrogen peroxide activity and reduce inflammation and swelling, thereby enhancing healing of ulcer. Topical phenytoin sodium appears to enhance healing by promoting fibroblast proliferation, facilitation of collagen deposition, glucocorticoid antagonism and antibacterial activity.8 This study was done to investigate whether topical insulin application versus topical phenytoin application has a role in the process of wound healing. This would provide a clinically and economically beneficial method to accelerate the process of wound healing. Aim and objective: To compare the efficacy of topical phenytoin vs topical honey in chronic diabetic ulcers in terms of rate of wound healing, granulation tissue formation and quality of graft bed for skin grafting.
MATERIAL AND METHODS Present study was a prospective comparative study conducted in the department of General Surgery AJ Medical college Hospital, Bangalore between October 2018 to October 2020. Study population was 50 patients with chronic diabetic foot ulcers chosen by purposive sampling technique. Inclusion Criteria: Patients who had long standing chronic ulcers like diabetic ulcers, venous ulcers, pressure ulcer ( with slough, contamination, edema and foul smell). Exclusion Criteria: 1. Patients with Acute wounds like burns, abrasions, lacerations, clean and granulated ulcers Study was approved by ethical committee of the institute. A valid written consent was taken from the patients after explaining study to them. Data was collected with pretested questionnaire. A complete detailed history, physical evaluation relevant blood investigations, radiological investigations on patients were done and then grouped accordingly. Based on the envelop method, patients were divided into two groups of 25 patients each that is group A (topical honey) and group B (Phenytoin sodium ). Group A (Topical honey) Protocol: One ml of honey that is diluted with in 5ml of sterile normal saline to form a suspension. Sterile gauze was soaked in the suspension and placed over the wound at 20 mg/cm2 surface area. The dressing was changed everyday Group B (Phenytoin Sodium) Protocol: In Group B, one 100 mg Phenytoin sodium tablet is opened and placed in 5ml of sterile normal saline to form a suspension. Sterile gauze was soaked in the suspension and placed over the wound at 20 mg/cm2 surface area. The dressing was changed everyday. Ulcer thoroughly washed with saline to remove the slough and specimen was collected from the edge and sent to the lab where Gram staining was done, followed by culture in blood agar and after 24-48hrs organism was identified by colony morphology and appropriate antibiotics based on antibiotic sensitivity testing. After the initial assessment was complete, patients were divided into the Group A and Group B. The dressing was changed everyday in both groups. Whenever needed a through surgical debridement was done. GRBS was monitored so that the test group patient did not have hypoglycaemica. The ulcers in both the groups were inspected after removal of dressing and were analysed. Size of the wound calculated by multiplying the maximum perpendicular length by the maximum width of the wound bed by measuring tape after tracing the wound margins on a sterile paper and typically recorded in cm2. Presence or absence of slough and the type of slough was noted. The microbiological profile as to whether monomicrobial or polymicrobal was also studied. Outcome was measured in terms of wound reduction, granulation tissue formation between the two groups at the end of each week and recorded. Final wound area was measured on 30th day. Comparison between the wound size reductions among two groups was done at end of 30th day. Data was analysed using SPSS version 22.
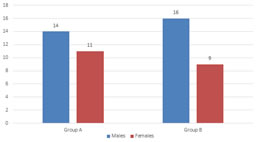
RESULTS The mean age in the Group A was 52.53 SD+ 12.57 years and in the Group B was 58.83 SD+ 12.5 years. In our study most common age group was of 61-70 years with 15 cases (50.00%). There was a positive co relation between the age of the patient and the incidence of ulcer, as the age increased There was increase in the number of ulcers, this was statistically significant with a p value 0.046, r=0.87. (table 1) Our study included 30 males and 20 females with a male to female ratio 1.5:1. Thus both the groups were comparable with respect to age and sex. (fig 1) The mean FBS in the Group A was 140.4 ±20.87 mg/dl and in the Group B was 137.60± 15.8 mg/dl. The mean PPBS in the Group A was 176.7 ± 32.59 mg/dl and in the Group B was 165.37± 24 .08 mg/dl. The mean HBA1C in the Group A was 8.11 ±1.2 mg/dl and in the Group B was 8.17±1.3 mg/dl. (table 1) There was no statistical significance between the two groups with growth of organism of the pus culture on day 0 with group A 23 cases were positive and group B 22 cases had a positive growth with a p value more than 0.05. (table 2) There was no statistical significance between the two groups with growth of organism of the pus culture on day 30 with group A (8 patients showed repeat positive culture ) and group B (7 cases showed repeat positive culture growth ) with a p value more than 0.05 hence the two groups are comparable . (table 2) There was no statistical significance between the two groups with size of the ulcer on day 0 with group A mean was 14.75 cms and group B 14.6 cms. (p>0.05) There was no statistical significance between the two groups with size of the ulcer on day 30 with group A mean was 9.33cms and group B 8.6 cms with a p value more than 0.05 hence the two groups are comparable. (table 3) There was no statistical significance between the two groups with percentage reduction size of the ulcer on day 30 with group A mean was 31.2 and group B 41.10 %. (p>0.05) (fig 2) Quality of ulcer bed was better in group A (20 patients had negative repeat pus culture) compared to group B (20 patients had negative repeat pus culture). (table 4,5)
Table 1: Distribution of patients according to group and parameters
Figure 1: Distribution of patients according to group and age
Table 2: Distribution of patients according to group and pus culture at day 0 and day 30
Table 3: Distribution of patients according to group and ulcer size at day 0 and day 30
Figure 2: reduction in ulcer size percentage in groups after 30 days Table 4: Distribution of patients according to group and ulcer bed status at day 0
Table 5: Distribution of patients according to group and ulcer bed status at day 30
DISCUSSION In the present study the age group ranged between 36 years and 80 years the most common age group was between the age of 61-70 years with 15 cases, 50.00%. there was a positive co relation between the age of the patient and the incidence of ulcer, as the age increased there was increase in the number of ulcers. Male to female ratio was 1.5:1. In Bansal et al.3, among those with diabetic foot ulcer, 56.31 percent were in the age group of 51-70 years, which is in agreement to our study in which the most common age group affected by diabetic ulcers is 51-70 years (50 %). Both the groups were comparable with respect to FBS, PPBS and HbA1C. There was no statistical significance between the two groups with growth of organism of the pus culture on day 0 and day 30. (p>0.05) Ramalingam et al. 8 stated that 43 of had good glycemic control among the remaining 7 subjects, 4 of them did not have proper glycemic control due to non-co-operative to the diabetic treatment. In our study statistical significance between the two groups with growth of organism of the pus culture on day 30 with group a (8 patients showed repeat positive culture) and group b (7 cases showed repeat positive culture growth). Siddharth P. Dubhash 9 stated there was no Methicillin-resistant Staphylococcus aureus (MRSA) was the most common organism isolated in the study (16 %) along with other organisms like Pseudomonas and Klebsiella. Eradication of infection was evident earlier in the honey-treated group (mean 8.4 days ± 1.71) and phenytoin-treated group (mean 9.28 days ± 2.03) as compared to the group treated with saline dressing (mean 14.94 days ± 2.56). In our study Group B showed more reduction in ulcer size percentage than group A, but the difference was not significant statistically. (p>0.05) Ramarao, et al.10 In this study among patients with group A significant reduction of mean ulcer area was observed (307.23±169.87 mm2) with higher mean percentage reduction (35.19 ± 19.00 percent) whereas in group B the mean percentage reduction was significantly less (18.82 ± 4.06 percent) with less reduction of mean final ulcer area (149.90 ± 64.45 mm2 ). the study showed a drastic significant reduction in the size of the ulcer. O M Oluwatosin et al.11 at the assigned 50 cases into three groups for honey, phenytoin/honey mixture, and phenytoin topical treatment. Mean percent reduction in size in the group treated with honey, 27.0 (36.9), was not significantly different (H = 0.26; 2 df; p = 0.88) from that of the mixture group, which was 25.9 (46.4), and from that of the phenytoin group which was 35.5 (53.2). This percent reduction in size was significantly greater, (H = 7.69; 2 df; P = 0.02), during the first week in the phenytoin group than in the other groups. Four of the cases progressed to complete healing at the end of four weeks with phenytoin. Siddharth P. Dubhash 9 included 150 patients, 3 groups of 50 each (group A, honey dressing; group B, phenytoin dressing; group C, saline dressing) There was significant reduction in the wound area at the end of 3 weeks of treatment in the honey- and phenytoin-treated groups compared to the saline-treated group. The percentage reduction of wound achieved at the end of 3 weeks was 20.66 % for the honey-treated group, 15.80 % for the phenytoin-treated group and 8.07 % for the saline-treated group. There is no significant difference between the two modalities of management in respect to quality of bed for skin grafting though honey had slightly better results. Siddharth P. Dubhash (81) stated there was no difference though honey had slightly better results in respect to quality of bed for skin grafting.
CONCLUSION Topical phenytoin is a more efficient and easily, readily available alternative to topical honey in patients with chronic non healing diabetic ulcers.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home