|
Table of Content - Volume 19 Issue 1 - July 2021
A study of clinical profile of patients with acute pancreatitis at a tertiary health care centre
Deepak Ramakant Patil1*, Sumit Raghunath Chaudhari2
1,2Assistant Professor, Department of General Medicine, Dr.Ulhas Patil Medical College, Jalgaon, Maharashtra, INDIA. Email: dr_deepakpatil@yahoo.com Abstract Background: Acute pancreatitis is one of the most common diseases affecting the exocrine pancreas. The incidence of acute pancreatitis has increased during the past 20 years. The overall mortality rate of acute pancreatitis ranges from 1% in mild acute pancreatitis to 30% in severe acute pancreatitis. Aim and objective: To study the clinical profile of patients with acute pancreatitis at a tertiary health care centre Methodology: Present study was a prospective study carried out on patients with acute pancreatitis admitted in department of surgery. Data collected was sociodemographic data, clinical history and clinical examination. All patients underwent biochemical investigations, Radiological investigations. All the patients were treated with conservative treatment. Results: Most commonly affected age group was 21-40 year males. Male to female ratio was 5:1. Most common etiological factor was alcohol 21(70%). 5(16.67%) patients had history of biliary tract disease. Epigastric pain (100%) was most common followed by Nausea vomiting (83.33%). Keywords: acute pancreatitis.
INTRODUCTION The pancreas has its first mention around 200 B.C., when it was referred to as the ‘finger of the liver’ in a literature by Talmud. Wirsung first demonstrated the ducts in human pancreas in 1642.1,2 Acute pancreatitis is an acute inflammatory process of the pancreas, with variable involvement of other regional tissues or remote organ systems.3 Pancreas being an integral organ in the digestive apparatus, inflammation of the pancreas results in profound metabolic derangements. The release of hydrolytic enzymes, cytokines and toxins promote a hypermetabolic state as manifested by increased resting energy expenditure (REE).4,5 The increased nutrient requirements occurring as a result of the increased REE are complicated by derangements in the metabolism of these nutrients in acute pancreatitis. Acute pancreatitis patient present with epigastric pain, vomiting, high fever, tachypnoea, mild jaundice, haematemesis/malaena, distension of abdomen and oliguria. Various scoring systems are used for classification of Acute pancreatitis and management of it. The scoring systems are Atlanta classification,3 Ranson’s Criteria, 6APACHE II scoring system (Acute Physiology and Chronic Health Evaluation)7. Depending on its severity, acute pancreatitis can have severe complications and high morbidity and mortality despite of treatment. While mild cases can be successfully treated by conservative management, severe cases often require admission to intensive care unit and even surgery. Management of acute pancreatitis is an aggressive medical management with analgesics for pain control, bowel rest, intravenous fluids to maintain hydration. Enteral nutrition is an important treatment modality. Advantages of enteral nutrition over total parentral nutrition are cost effective, less catheter-related complications, better maintenance of intestinal mucosal integrity and less alteration of intestinal mucosal barrier function and intestinal permeability. Present study was conducted to study the clinical profile of patients with acute pancreatitis at a tertiary health care centre. Aim and objective: To study the clinical profile of patients with acute pancreatitis at a tertiary health care centre MATERIAL AND METHODS Present study was a prospective study carried out at department of surgery at a tertiary health care centre. Study population was patients with acute pancreatitis admitted in department of surgery. Inclusion criteria: 1. All the patients diagnosed as acute pancreatitis. 2. Patients who were ready to follow up Exclusion criteria: 1. Patients with chronic pancreatitis. 2. Patients not willing to participate in the study Study was approved by ethical committee of the institute. Valid written consent was taken from the patients after explaining study to them. Datawas collected with pretested questionnaire. Data included sociodemgraphic data like age, sex. Detailed clinical history was noted. A through clinical examination was done. All patients underwent biochemical investigations including a total and differential WBC counts, serum amylase blood sugars, serum creatinine, serum electrolytes, serum calcium, liver function tests and ascitic fluid or pleural fluid amylase as and when required. Radiological investigations like plain X-ray abdomen AP view, X-ray chest PA view and USG were done in all patients. CT scan was done when required. All the patients were treated with conservative treatment. It included keeping patients NPO (nil per oral), i.v. fluids administration, nasogastric tube aspiration, i.v. analgesics, antibiotics along with injectible proton pump inhibitors. Injection octreotide was given to decrease pancreatic secretions. All patients were monitored closely with vital parameters, abdominal girth charting, intake/output monitoring and clinically assessed daily to monitor the response of conservative management. All patients who recovered were discharged and followed up on outpatient basis. Surgical/ Radiological intervention was done according to severity of disease and response to conservative management. Surgical interventions done were USG guided pigtail catheter insertion, Exploratory laparotomy with drainage of abscess with lavage, Open necrosectomy with closed drain placement and ICD insertion. Data was entered in excel sheet. Data was analysed with SPSS version 23.
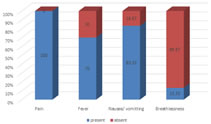
RESULTS We studied total 30 patients. Out of these 30 patients, majority of the patients were from the age group of 21-40 years (66.66%) followed by 41-60 years (20%). Patients below 20 years and above 60 years were 6.67% each. (table 1) In our study male (83.33%) predominated females (16.67%). Male to female ratio was 5:1. In our study we fund most common etiological factor was alcohol 21(70%). 5(16.67%) patients had history of biliary tract disease. Trauma was found in 2 (6.67%) patients. one patient had iatrogenic history and one had no etiological factor. Other factors are hyperlipidemia, drugd, infection and ischaemia but none of the patient had such history. (table 2) Fig 1 shows distribution of patients according to clinical features. In our study, all patients complained of pain. Epigastric pain was most common. Fever was seen in 70 % Of study population. Nausea vomiting was observed in 83.33% patients. Breathlessness was seen in 13.33% of study population. It was due to pleural effusion. Chest xray showed 6 patients had pleural effusion. Left pleural effusion was seen in 3 patients, right plural effusion was seen in 2 patients and bilateral pleural effusion was seen in 1 patient. Depending on the clinical features and investigations patients were classified according to Ranson’s score. Majority of the patients (63-34%) had Ranson’s score of 0-2. Ranson’s score of 3-4 and 5-6 were seen in 13.33% and 10% patients respectively. out of 30 patients score of 7-8 was observed in 4(13.33%) patients. In our study, pleural effusion was seen in 6(20%) population. Acute necrotising pancreatitis was seen in 01 (3.33%) patients. Pancreatic pseudocyst , pancreatic abscess were seen in one patient each. Acute renal failure was seen in one patient and acute respiratory distress syndrome was observed in 1 patient. (table 4) In our study, 26 patients were managed by conservative management and 4 needed surgical intervention. In 2 patients Open necrosectomy with closed drain placement was done. Exploratory laparotomy with drainage of abscess with lavage and closed drain placement was done in 1 patient. One patient with pleural effusion was treated with ICD insertion. In our study, 28 (93.33%) out of 30 patients responded well to the treatment and discharged while 2 (6.67%) patients died.
Table 1: Distribution of patients according to age group
Table 2: Distribution of patients according to etiological factors
Figure 1: Distribution of patients according to clinical features
Table 3: Distribution of patients according to Ranson’s score
Table 4: Complications in patients with acute pancreatitis
DISCUSSION We studied total 30 patients. Out of these 30 patients, majority of the patients were from the age group of 21-40 years (66.66%) followed by 41-60 years (20%). Baig SJ34 et al. from Kolkata found that the mean age was 40 years In our study male (83.33%) predominated females (16.67%). Male to female ratio was 5:1. Baig SJ et al.8 Kolkata, found in their study of 45 patients, 33 were men (73%) and 12 were women (27%). Another study by Wig JD et al.9 showed that out of 161 patients, 127were men (77%) and 37(33%) were women. The higher incidence of women in their study was probably due to gall stones. In our study we found most common etiological factor was alcohol 21(70%). 5(16.67%) patients had history of biliary tract disease. Trauma was found in 2 (6.67%) patients. one patient had iatrogenic history and one had no etiological factor. Other factors are hyper lipidemia, drugs, infection and ischaemia but none of the patient had such history. In a study by Baig SJ et al.8 from Kolkata found alcoholism in 41%, gallstones in 23.5%, trauma in 17.6%, and idiopathic in 11.7%. Another study by F. Anderson et al.37, found alcohol as the aetiology in two thirds (66%) of the admissions and gall stones in 17%, while 5% were idiopathic. 10 Fig 1 shows distribution of patients according to clinical features. In our study, all patients complained of pain. Epigastric pain was most common. Fever was seen in 70 % Of study population. Nausea vomiting was observed in 83.33% patients. Breathlessness was seen in 13.33% of study population. It was due to pleural effusion. Chest Xray showed 6 patients had pleural effusion. Left pleural effusion was seen in 3 patients, right plural effusion was seen in 2 patients and bilateral pleural effusion was seen in 1 patient. In our study, serum amylase was within the normal range in only 10% of the patients whereas it was raised in 90% of the patients. Serum lipase was raised in 28 (93.33%) of the patients. Agrawal et al. 11 observed a high sensitivity of serum amylase in the diagnosis of pancreatitis of 95-100%. Depending on the clinical features and investigations patients were classified according to Ranson’s score. Majority of the patients (63-34%) had Ranson’s score of 0-2. Ranson’s score of 3-4 and 5-6 were seen in 13.33% and 10% patients respectively. out of 30 patients score of 7-8 was observed in 4(13.33%) patients. Marco Simoesa et al. found a sensitivity of 91.2 % and specificity of 74.4% related to degree of sensitivity and Ranson’s score 3 or above.
CONCLUSION Acute pancreatitis is a disease with male predominance. Alcohol is the most common etiological factor. Conservative management is the mainstay of treatment in acutepancreatitis.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home