|
Table of Content - Volume 20 Issue 2 - November 2021
Prospective study of Diabetic foot Ulcer outcomes using Diabetic Ulcer Severity Score (DUSS)
Sadanad Nandihalli1*, Sanjay Karpur2, Sudhir Bhat3*
1,3Assistant Professor,2Professor, Department of Surgery, Belgavi Institute of Medical Sciences, Belgavi, INDIA. Email: drsudhirbhat@gmail.com
Abstract Background: In the years between 1958 and 1993, the number of people diagnosed with Diabetes multiplied five – fold.1 In 1994, 135 million patients world – wide were living with Diabetes Mellitus. By the year 2025, it is estimated that this figure would increase to more than 300 million .2 Currently 25 million Indians have diabetes. The loss of a limb or foot is one of the most feared complications of diabetes and yet foot problems remain the commonest reason for diabetic patients to be hospitalized. Diabetic foot ulcers precede almost 85% of amputations. Objectives: To predict the risk of amputation. Prognosticate diabetic foot ulcer healing and complications. Average length of Hospital stay(ALOS). Material and Methods: This is prospective study conducted in belgavi institute of medical sciences, Belgavi from 2018 till 2020. Total of 90 Diabetic patients with diabetic foot ulcers irrespective of their duration, attending surgical outpatient clinic or admitted into the Belgavi Institute of Medical Sciences, Belgavi were recruited into the study based on the inclusion and exclusion criteria. ulcers were followed up for a minimum period of 6 months. Once a patient’s ulcer had healed completely either by primary healing or skin grafting or a lower-limb amputation performed, the outcome was noted and the patient was deemed to have completed the study. Results and Interpretation: Most of the patients were male in the 5 n 6 decade, scoring done using duss score 11% requiring major ampuatation and 44 % minor ampuatation. With increases in DUSS score ampuatation chances are more. Conclusion: DUSS scoring system provides an easy diagnostic tool for predicting probability of healing or amputation by combining four clinically assessable wound based Parameters. Keywords: Ulcer Ampuatation Healing.
INTRODUCTION In the years between 1958 and 1993, the number of people diagnosed with Diabetes multiplied five – fold.1 In 1994, 135 million patients world – wide were living with Diabetes Mellitus. By the year 2025, it is estimated that this figure would increase to more than 300 million .2 Currently 25 million Indians have diabetes. The loss of a limb or foot is one of the most feared complications of diabetes and yet foot problems remain the commonest reason for diabetic patients to be hospitalized. Diabetic foot ulcers precede almost 85% of amputations. Foot ulcers are a common complication of Diabetes and represent a major source of morbidity. Fifteen percent of Diabetics develop foot ulcers during their life time with significant health related decrease in quality of life and consumption of a great deal of healthcare resources .3 A number of foot ulcer classification systems for example, the Wagner system and the University of Texas (UT) systems have been devised in an attempt to categorize ulcers more effectively and thereby, allow effective comparison of the outcome of routine management in different centers and treatment strategies. These systems are variously based on the site of ulcer, its depth, and presence or absence of neuropathy, infection and peripheral arterial disease and have been used to compare the outcomes. DUSS (Diabetic Ulcer Severity Score) is one of the latest wound based system of classification which is useful tool to measure outcomes of diabetic foot ulcers.
METHODOLOGY This is prospective study conducted in Belgavi Institute of Medical Sciences Belgavi From 2018 Till 2020. Total of 90 Diabetic patients with diabetic foot ulcers irrespective of their duration, attending surgical outpatient clinic or admitted into the Belgavi Institute of Medical Sciences, Belgavi were recruited into the study based on the inclusion and exclusion criteria. ulcers were followed up for a minimum period of 6 months. Once a patient’s ulcer had healed completely either by primary healing or skin grafting or a lower-limb amputation performed, the outcome was noted and the patient was deemed to have completed the study Total of 90 Diabetic patients with diabetic foot ulcers irrespective of their duration, attending surgical outpatient clinic or admitted into Belagavi institute of medical sciences, Belagavi were recruited into the study based on the inclusion and exclusion criteria mentioned below. The baseline demographic data which included age, sex, occupation, education status, habits, socioeconomic status and treatment history were taken. Ulcers were labelled infected if a purulent discharge was present with two of the local signs mentioned below. Wound depth was evaluated using a sterile blunt probe. The ability to probe to bone with the presence of local inflammation (warmth, erythema, lymphangitis, lymphadenopathy, edema, pain) or signs of systemic infection and suggestive radiological features provided a clinical diagnosis of osteomyelitis.47 Peripheral vascular disease was clinically detected by the absence of both pedal pulses, patients were categorized into groups having either single or multiple ulcerations on the same foot. In patients with multiple ulcers, the wound with the highest grading was selected for analysis. For wounds with identical grading, the larger wound was chosen. Unhealed ulcers were followed up for a minimum period of 6 months. Once a patient’s ulcer had healed completely either by primary healing or skin grafting or a lower-limb amputation performed, the outcome was noted and the patient was deemed to have completed the study.
DIABETIC ULCER SEVERITY SCORE (DUSS) Ulcers were scored by the below mentioned variables. Diabetic Ulcer Severity Score (DUSS) was calculated by adding these separate scored variables to a theoretical maximum of 4.
Table 4: DUSS scoring system
Table 5: Ulcer grading depending on depth
Ulcer grading done to assess depth of ulcer to detect the presence of osteomyelitis. Standard treatment care was given to all these patients, which included oral hypoglycemic or insulin for good control of Diabetes, health education, antibiotics and regular wound care. Figure 1
Blunt probe used to measure the depth of the wound Healing was defined as complete epithelization or healing after skin grafting. Amputation rate was defined as the percentage of patients undergoing either minor or major amputation within the observation period. Toe or forefoot amputations were taken as minor amputation and below- or above-knee amputation were taken as major amputation. Follow up: Dressings were done every day but, these patients were followed up in the surgical outpatient clinic for DUSS scoring once in fortnight for 1st month, then once in a month till the ulcer healed or for a minimum period of up to 6 months. Ulcer healing was assessed as mentioned earlier. Inclusion criteria: All patients aged >18 years admitted to the surgical department of Belagavi institute of medical sciences Belagavi with history of wound, with or without discharge from the wound, which were confined to foot (below ankle). Both type 1 and2 diabetes mellitus patients are included in the study Exclusion criteria: Venous stasis ulcers with Diabetes mellitus. Non diabetic neuropathic ulcers. Ulcers above the ankle. All non-Diabetics with foot ulcers. Gangrenous Toe and Foot. Recurrent ulcers of Foot. Statistical analysis: A descriptive statistics based on the study on “DUSS” considering the reduction in the chance of healing for 1 score point change in DUSS score (35%) was analyzed and expressed in percentages. Baseline characteristics were expressed as mean, median and inter quartile range. Kaplan-Meier method was used to calculate the probability of healing. Cox regression was used to find the correlation between DUSS and healing. Sample size for the present study was estimated to be 90 using nMaster software based on the study “DUSS” considering the reduction in the chance of healing for 1 score point change in DUSS score (35%). Here α error considered was 5% (95% confidence). OBSERVATIONS AND RESULTS Table 6: Age-wise distribution of study population
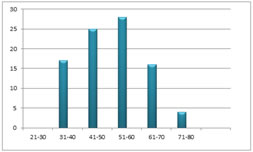
Figure 2: Bar diagram showing age-wise distribution of study populationMost common age group affected with Diabetic foot was between 51-60 years, Second group being between 41-50 years. Mean age group was 51.74 ±10.95 years. Median age was 51.0 year.
Table 7: Gender-wise distribution of study population
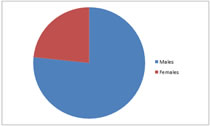
Figure 3: Pie diagram showing gender distribution of study populationMales were commonly affected by Diabetic foot ulcers accounting to 76.7% in our study.
Table 8: Distribution of DUSS score among study population
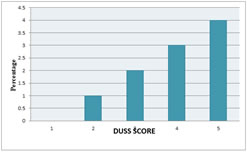
Most commonly ulcers were of DUSS score of 3 followed by Score 2. Mean score was 2.39. Median score of 2.00 (IQR= 2 to 3) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Amputation |
Total |
|
|
Number of patients |
Percentage(%) |
Done |
50 |
55.55 |
Not done |
40 |
44.44 |
Total |
90 |
100% |
Total 55.55% of patients underwent amputation in our study.
Table 10: Major amputation among the study population
|
No. of pts |
Percentage(%) |
Done |
10 |
11.11 |
Major amputation was done for 11.11% of patients in our study.
Table 11: Minor amputation among the study population
|
No Pts . |
% |
Done |
40 |
44.44 |
Minor amputation was done in 44.44% of patients in our study.
Table 12: Pattern of ulcer healing with DUSSscore-0 in each follow –up visit
DUSS sore |
Follow up visits |
Healed |
Amputation |
Not healed |
n (%) |
n (%) |
n (%) |
||
0 |
1 |
0 (0%) |
0 (0%) |
5 (100%) |
2 |
3 (60%) |
0 (0%) |
2 (40%) |
|
3 |
0 (0%) |
0 (0%) |
2 (100%) |
|
4 |
1 (50%) |
1 (50%) |
0 (0%) |
|
5 |
0(0%) |
0(0%) |
0(0%) |
|
6 |
0(0%) |
0(0%) |
0(0%) |
|
7 |
0(0%) |
0(0%) |
0(0%) |
Three out of 5(60%) ulcers got healed by 2nd follow up, one healed by 4th follow up and remaining one underwent amputation during 4th follow up.
Table 13: Pattern of ulcer healing with DUSS score 1 in each follow up visit
DUSS |
Follow up |
Healed |
Amputation |
Not healed |
n (%) |
n (%) |
n (%) |
||
0 |
1 |
0 (0%) |
0 (0%) |
16 (100%) |
2 |
0 (0%) |
0 (0%) |
16 (100%) |
|
3 |
9 (56.2%) |
0 (0%) |
07 (43.8%) |
|
4 |
4 (57.14%) |
0 (0%) |
03 (42.8%) |
|
5 |
1 (33%) |
1 (33%) |
1 (33%) |
|
6 |
1 (100%) |
0 (0%) |
0 (0%) |
|
7 |
0 (0%) |
0 (0%) |
0 (0%) |
9 (56.2%) healed by 3rd follow up. 4 (57.14) – healed by 4th follow up.
Majority of ulcers i.e. 09(56.2%) healed by 3rd follow up, 04 got healed by 4th follow up, 1 healed by 5th follow up and remaining 1 healed by 6th follow up, 1 underwent amputation during 5th follow up.
Table 14: Pattern of ulcer healing with DUSS score 2 in each follow up visit
DUSS |
Follow up |
Healed |
Amputation |
Not healed |
n (%) |
n (%) |
n (%) |
||
2. |
1 |
0 (0%) |
0 (0%) |
0 (0%) |
2 |
0 (0%) |
0 (0%) |
0 (0%) |
|
3 |
5 (20%) |
0 (0%) |
20 (80%) |
|
4 |
4 (20%) |
5 (25%) |
11 (55%) |
|
5 |
3 (27.27%) |
4 (36.36%) |
4 (36.36%) |
|
6 |
3 (75%) |
1 (25%) |
0 (0%) |
|
7 |
0(0%) |
0 (0%) |
0 (0%) |
Five ulcers out of 25(20%) healed by 3rd follow up, 04 healed by 4th follow up, 03 healed by 5th follow up,0 5 underwent amputation by 4th follow up, 04 underwent amputation by 5th follow up, 1 underwent amputation by 6th follow up.
Table 15: Pattern of ulcer healing with DUSS score 3 in each follow up visit
DUSS |
Follow up |
Healed |
Amputation |
Not healed |
n (%) |
n (%) |
n (%) |
||
3. |
1 |
0 (0%) |
0 (0%) |
27 (100%) |
2 |
0 (0%) |
0 (0%) |
27 (100%) |
|
3 |
0 (0%) |
0 (0%) |
27 (100%) |
|
4 |
1 (3.7%) |
7 (25.92) |
19(70.37%) |
|
5 |
2 (10.52%) |
8 (42.10%) |
09(47.36%) |
|
6 |
0 (0%) |
5 (55.55%) |
04(44.44%) |
|
7 |
0 (0%) |
4 (100%) |
0 (0%) |
One ulcer out of 27 healed by 4th follow up, 2 healed by 5th follow up, 07 underwent amputation by 4th follow up, 08 underwent amputation by 5th follow up, 05 underwent amputation by 6th follow up, 04 underwent amputation by 7th follow up.
Table 16: Pattern of ulcer healing with DUSS score 4 in each follow up visit
DUSS |
Follow up |
Healed |
Amputation |
Not healed |
n (%) |
n (%) |
n (%) |
||
4. |
1 |
0 (0%) |
0 (0%) |
17 (100%) |
2 |
0 (0%) |
0 (0%) |
17(100%) |
|
3 |
0 (0%) |
0 (0%) |
17 (100%) |
|
4 |
0 (0%) |
4 (23.52) |
13(76.47%) |
|
5 |
2 (15.38%) |
6 (46.15%) |
5 (38.46%) |
|
6 |
1 (20%) |
2 (40%) |
2 (40%) |
|
7 |
0 (0%) |
2 (100%) |
0 (0%) |
Most of the ulcers with score 4 underwent amputation, 04 of them by 4th follow up, 06 by 5th follow up, 02 by 6th follow up and 02 underwent amputation by 7th follow up. Remaining 02 healed by 5th and one healed by 6th follow up respectively. The above tables showed that ulcers with lower score healed earlier when compared to those ulcers with higher scores. Majority of ulcers with score 0 healed by the end of 2nd follow up, most ulcers with score 1 healed by 3rd or 4th follow up, most ulcers with score 2 healed by 3th and 4th follow up. Patients with Score 3, One healed and 07 underwent amputation by 4th follow up, 2 healed and 08 underwent amputation by 5th follow up, 05 underwent amputation by 6th follow up, 04 underwent amputation by 7th follow up. The patients with score 4, four of them by 4th follow up, 06 by 5th follow up, 02 by 6th follow up and 02 underwent amputation by 7th follow up. Remaining 2 by 5th and 1 by 6th follow up were healed.
Table 17: Comparison of DUSS score with amputation (major+minor)
DUSS Score |
Amputation |
|
|
Done |
Healed Ulcers |
|
n (%) |
n (%) |
0 |
1 (20%) |
4 (80%) |
1 |
1 (6.25%) |
15 (93.75%) |
2 |
10 (40%) |
15 (60%) |
3 |
24 (88.88%) |
03 (11.11%) |
4 |
14 (82.35) |
03 (17.64%) |
Total |
50 |
40 |
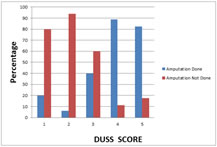
Contingency Coefficient=0.544, P<0.000
One (20.0%) out of 05people with score 0 had amputations, 1(6.25%) out of 16 people with score 1 had amputations, 10(40%) out of 25 people with score 2 had amputations, 24(88.88%) out of 27 people with score 3 had amputations, 14(82.35%) out of 17 people with score 4 had amputations. Overall 50 (55.55%) of 90 people had amputations.
Figure 5: Comparison of DUSS score with amputation(major+minor)
Table 18: Comparison of DUSS score with major amputation
DUSS Score |
Major Amputation |
|
|
Done |
Not Done |
|
n (%) |
n (%) |
0 |
0 (0%) |
05 (100%) |
1 |
0 (0%) |
16 (100%) |
2 |
0 (0%) |
25 (100%) |
3 |
4 (14.81) |
23 (85.18) |
4 |
6 (35.29) |
11 (64.70%) |
Total |
10 (11.11%) |
80 (88.88%) |
Contingency Coefficient=0.390, P<0.003
Total of 04 (14.81%) of 27 people with score 3 had major amputations; 06(35.29%) out of 17 people with score 4 had major amputations in our study. None of the patients with score 0, 1 and 2 had major amputation.
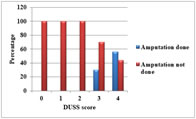
Figure 6: Comparison of DUSS score with major amputation
Table 19: Comparison of DUSS score with minor Amputation
DUSS Score |
Minor Amputation |
|
|
Done |
Not Done |
|
n (%) |
n (%) |
0 |
01(20%) |
04(80%) |
1 |
01(6.3%) |
15(93.8%) |
2 |
10(40%) |
15(60%) |
3 |
20(74.1) |
07(25.9) |
4 |
08(47.1) |
09(52.9) |
Total |
40(44.44%) |
50(55.55%) |
Contingency Coefficient=0.390, P<0.000
One (20%) of the patients with score 0 had minor amputation; 01(6.3%) of 16 patients with score 1 had minor amputation, 10(40%) of 25 patients had minor amputation, 20(74.1%) of 27 patients with score 3 had minor amputations, 08(47.1%) of 17 patients with score 4 had minor amputations. Minor Amputations were more common in patients with DUSS Score of 3 in our study.
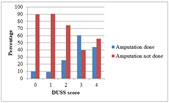
Figure 7: Comparison of DUSS score with minor amputation
Table 20: Comparison of DUSS score with types of Amputation
DUSS Score |
Toe amputation |
Fore foot amputation |
Above knee Amputation |
Below knee amputation |
|
Minor Amputation |
Major Amputation |
||
0 |
01 (20%) |
0 (0%) |
0 (0%) |
0 (%0 |
1 |
01 (6.25%) |
0 (0%) |
0 (0%) |
0(1%) |
2 |
08 (32%) |
02 (8%) |
0 (0%) |
0 (0%) |
3 |
15(55.55%) |
05 (18%) |
0 (0%) |
04 (14.81) |
4 |
03(17.64%) |
05 (29.41%) |
02 (11.76%) |
04(23.52%) |
Total |
28(31.11%) |
12(13.33%) |
02(2.22%) |
08(8.88%) |
Toe amputation was done in total of 28(31.11%) of patients. One (20.0%) patients with DUSS score 0, 01 (6.25%) patients with score 1, 08 (32%) of patients with DUSS score 2, 15 (55.55%) of patients with DUSS score 3, 3 (17.64%) of patients with score 4 had toe amputations. Fore foot amputation was done in total of 12 (13.33%) of patients. None of the patients with DUSS score 0 and 1 i.e., 0 (0.0%), 2 (8%) of patients with DUSS score 2, 05 (18%) of patients with DUSS score 3, 05 (29.41%) of patients with score 4 had forefoot amputations. Below knee amputation was done in total of 08 (8.88%) of patients. None of the patients with DUSS score 0, 1 and 2 i.e., 0 (0.0%), 04 (14.81%) of patients with DUSS score 3, 04 (23.52%) of patients with score 4 had below knee amputations. Above knee amputation was done in total of 02 (2.22%) of patients. None of the patients with DUSS score 0, 1 2and 3 i.e., 0 (0.0%), 02 (2.22%) of patients with DUSS score 4, had above knee amputations. There were no revision amputations in our study.
Table 21: Distribution of ulcers (DUSS score 0-4) with duration ofDiabetes
DUSS SCORE |
Duration in groups (in years) |
Total |
||||
1(1-5) |
2(6-10) |
3(11-15) |
4(16-20) |
5(>21) |
|
|
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
|
0 |
3(9.4.0%) |
2(5.0%) |
0(0.0%) |
0(0.0%) |
0(.0%) |
5(5.6%) |
1 |
10(31.3%) |
5(12.5%) |
1(8.3%) |
0(0.0%) |
0(.0%) |
16(17.8%) |
2 |
13(40.6%) |
8(20%) |
3(25%) |
1(33.3%) |
0(0.0%) |
25(27.8%) |
3 |
4(12.5%) |
18(45%) |
3(25%) |
1(33.3%) |
1(33.3%) |
27(30%) |
4 |
2(6.3%) |
7(17.5%) |
5(41.7%) |
1(33.3%) |
2(66.7%) |
17(18.9%) |
Total |
32(100%) |
40(100%) |
12(100%) |
3(100%) |
3(100%) |
90(100%) |
Contingency Coefficient=0.484, P<0.036
Majority of foot ulcers among study population with DUSS score 0(9.4%) and 1(31.3%) were with <5years of duration of Diabetes, ulcers with score 2(85%) were with <15 years of duration of Diabetes, ulcers with score 3(70%) and score 4(59%) were with duration of Diabetes between 6-20 years. This difference in the DUSS score among the duration groups was found to be statistically significant (P<0.036).
Table 22: Distribution of Ulcers (DUSS score 0-4) with study end points.
DUSS score |
End points |
|
|||
Primary healing |
Skin grafting |
Amputation |
Total |
||
0 |
4 (80%) |
0 (0%) |
1 (20%) |
05 (100%) |
|
1 |
12 (75%) |
03 (18.75%) |
1 (6.25%) |
16 (100%) |
|
2 |
11 (44%) |
04 (16%) |
10 (40%) |
25 (100%) |
|
3 |
03 (11.11%) |
00 (00%) |
24 (88.88) |
27 (100%) |
|
4 |
00 (00%) |
03(17.64%) |
14 (82.35%) |
17 (100%) |
|
|
30 (33.33%) |
10 (11.11%) |
50 (55.55%) |
90 (100%) |
|
Majority of foot ulcers among study population with DUSS score 0, 1 and 2 healed by primary intention or skin grafting i.e., 4 (80.0%), 12 (75%) and 11 (44%) respectively. However among those with score 3 and score 4 majority required amputation i.e., 24 (88.88%) and 14 (82.35%) respectively. This difference in the DUSS score among the three groups was found to be statistically significant (P<0.00).
Table 23: Comparison of DUSS score with ALOS
DUSS |
Patients |
Mean(days) |
Std. Deviation |
0 |
05 |
4.40 |
0.89 |
1 |
16 |
5.06 |
2.54 |
2 |
25 |
5.36 |
2.44 |
3 |
27 |
5.92 |
1.85 |
4 |
17 |
8.35 |
3.70 |
Total |
90 |
5.98 |
2.77 |
Fisher value=5.042, df=4, P<0.001
Above table shows the comparison between the DUSS score and the average length of hospital stay,where in here mean hospital stay for 0,1,2,3 and 4 are 4.4,5.0,5.36,5.92 and 8.35 respectively. There is significant (p=0.001) correlation between DUSS score and ALOS. So increase in DUSS score will increase the length of hospital stay.
Table 24: Multivariate analysis of parameters reducing chances for healing
95% CI |
||||
|
Significance (p) |
Odds ratio |
Lower |
Upper |
Multiple Ulcers |
0.01 |
3.094 |
1.293 |
7.404 |
Probing to Bone |
0.00 |
27.77 |
5.895 |
130.89 |
Location |
0.07 |
0.382 |
0.132 |
1.103 |
Non palpable pulses |
0.001 |
0.137 |
0.037 |
0.506 |
Above table shows by multivariate analysis that all four parameters had an independent impact on wound healing. Dividing patients into subgroups with the same DUSS, we were able to demonstrate significant differences for probability of healing.
Table 25: Kaplan –Meier analysis for DUSS scores
|
Case processing summary |
|||
DUSS score |
Total N |
N of events |
Censored |
|
N |
Percent |
|||
0 |
05 |
01 |
04 |
80% |
1 |
16 |
01 |
15 |
93.75% |
2 |
25 |
10 |
15 |
60% |
3 |
27 |
24 |
03 |
11.11% |
4 |
17 |
14 |
03 |
17.64% |
|
90 |
50 |
40 |
44.44% |
Probability of healing with score 0 was 80%, 93.75% with score 1,60% with score 2, 11.11% with score 3, 17.64% with score 4 In our study most common bacteria isolated was Streptococcus(n=37) followed by staphylococcus(n=33), klebsiella(n=10) and E.coli (n=06) respectively.
- DUSS scoring system provides an easy diagnostic tool for predicting probability of healing or amputation by combining four clinically assessable wound based Parameters.
- Study groups can be stratified depending on severity of ulcers and thus can help provide a simple, streamlined approach in clinical setting without need of any advanced investigative tool.
DISCUSSION
Total of 90 Diabetic patients with foot ulcers irrespective of duration of ulcers admitted into the Apollo BGS hospital, Mysore were recruited into the study based on the inclusion and exclusion criteria mentioned earlier. Most common age group affected with Diabetic foot was between 51-60 years, second group being between 41-50 years. Mean age group was 51.74 ±10.95 years. Median age was 51.0. A study undertaken in the USA in 2004 through the 2002 National Hospital Discharge Survey, evaluated 275,000 in patient records from 500 hospitals from 1996 onwards. This study revealed that elderly Diabetics had twice the risk of developing a foot ulcer, three times the risk of developing a foot abscess and four times the risk of developing osteomyelitis.48 Toe amputations comprise the majority of Diabetes-related lower limb amputations. The age-adjusted Lower extremity amputation rate (LEA) in year 2002 among persons with Diabetes was highest for toe level amputation (rate of 2.6 per 1,000 persons), followed by below-knee amputation (rate of 1.6 per 1,000 persons).Both the age adjusted Fore foot amputation rate and above-knee amputation rate was 0.8 per 1,000 persons. Generally, the Lower extremity amputation rate is 15 to 40 times higher in the diabetic versus non diabetic populations, and the amputation rate is at least 50% higher in men compared to women. Lower extremity amputation rate among diabetic men was 7.0 per 1,000 persons compared with the rate among diabetic women reported at 3.3 per 1000 persons.49 In our study Toe amputation was done in total of 31.11% of patients, fore foot amputation was done in total of 13.33% of patients, Below knee amputation was done in total of 8.88% of patients, Above knee amputation was done in total of 2.22% of patients. Other than the original study there are no studies done on DUSS scoring system done by Beckert et al.12 which was a prospective study done with 1000 patients with diabetic foot ulcers. Overall 50 (55.55%) of 90 people had amputations in our study. Major Amputation (below- or above-knee amputation) was done for 11.11% of patients in our study. Minor Amputation (toe or forefoot amputations) was done in 44.44% of patients in our study. In our study On Kaplan Meier analysis the probability of healing with score 0 was 80%, 93.75% with score 1, 60% with score 2, 11.11% with score 3, 17.64% with score 4. In our study there was 80% probability of healing for score 0, decreasing to 17.64% with score 4. Similar to as shown by the study conducted by Beckert et al.12 They noted that a lower DUSS score was strongly associated with healing. Although the DUSS system makes no distinction between neuropathic and neuroischemic ulcers. There was high probability of healing for uncomplicated ulcers (score 0), decreasing to 17% for ulcers with a severity score of 4 (P =0.0001) according to Kaplan Meier analysis. In our study most common bacteria isolated was Streptococcus(n=37) followed by staphylococcus(n=33), klebsiella(n=10) and E.coli (n=06) respectively. Beckert et al.12 Reported primarily healing of 74% (n=1,000), Prompers et al.50 77% (n=1,229), Oyibo et al.5165% (n=194), Jeffcoate et al.52 66% (n=449), and Gul et al.53 72% (n=200). In the more than 10-year follow-up study conducted by Margolis et al.54 a cohort of 24,616 individuals with a diabetic neuropathic foot ulcer treated within a multicenter wound care network were studied. Total of 1653 (6.7%) individuals had an amputation and 46.3% of these amputations were of a toe or ray (minor amputation). The percentage of those who had an amputation varied from 5.6% to 8.4%. Of those who had an amputation, the percentage that had a minor amputation increased over time from 4.0% in the earlier years to more than 60% in the later years of observation. When the DUSS score was compared with the proportion of individuals undergoing amputation it was noted that a total of 04(14.8%) of 27 people with score 3 had major amputations, 06 Out of 17 people (35.3%) with Score 4 had major amputations in our study. None of the patients with score 0, 1 and 2 had major amputation. One (20%) of the patients with score 0 had minor amputation; 1(6.3%) of 16 patients with score 1 had minor amputation, 10(40%) of 25 patients had minor amputation, 20(74.1%) of 27 patients with score 3 had minor amputations, 08(47.1%) of 17 patients with score 4 had minor amputations. Minor Amputations were more common in patients with DUSS Score of 3 in our study. Most commonly ulcers were of DUSS Score of 3 followed by Score 2. Mean score was 2.39. One out of 10 people with score 0 (20.0%) had amputations, 1(6.3%) out of 16 people with score 1 had amputations, 10(40%) out of 25 people with score 2 had amputations, 24(88.9%) out of 27 people with score 3 had amputations, 14(82.4%) out of 17 people with score 4 had amputations. In the original study by Beckert et al. Patients with a score of 0 had no risk of major amputation, while patients with a score of 1 had a 2.4%, patients with a score of 2 had a 7.7%, patients with a score of 3 had an 11.2%, and patients with a score of 4 had a 3.8%. In comparison in our present study none of the patients with score 0, 1 and 2 had major amputation, 04 (14.8%) of 27 people with score 3 had major amputations; 06(35.3%) out of 17 people with score 4 had major amputations.
REFERENCES
- Harris M. I.: Descriptive Epidemiology, In:Diabetes in America, 2nd edition, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, NIH Publication Nr. 95-1468, (1995), 1-13.
- King H, Aubert RE, Herman WH et al. Global Burden of Diabetes 1995-2025. Diabetes Care 1998 September;21(9):1414-31.
- The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997 July;20(7):1183-97.
- Pryce T. D.: Perforating ulcers of both feet associated with diabetes and ataxic symptoms, The Lancet (Juli 1887), 11-12.
- Joslin EP. The Menace of Diabetic Gangrene. The New England Journal of Medicine 1934 July;16:20.
- Most RS, Sinnock P. The Epidemiology of Lower Extremity Amputations in Diabetic Individuals. Diabetes Care 1983 January;6:87-91.
- Ward JD. The Cost of Diabetic Foot Problems, Pharmaco Economics 1995;8(Suppl.1):55-7.
- a Foster A.: Psychological aspects of treating the diabetic foot, Practical Diabetes International (March/April 1997), Vol. 14, Nr. 2, 56-8.
- Wagner FW. The Dysvascular Foot. A system for Diagnosis and Treatment, Foot and Ankle 1981;2(2):64-122.
- Lavery AL, Armstrong DG, Harkless L. Classification of Diabetic Foot Wounds. The journal of Foot and Ankle Surgery 1996;35(6)528-531.
- Jeffcoate WJ, Macfarlane RM, Fletcher EM. The Description and Classificaton of Diabetic Foot Lesions. Diabetic Medicine 1993;10:676-9.
- Armstrong DG, Lavery LA, Harkless LB. Who is at risk for diabetic foot ulcertation? Clinics in Podiatric Medicine and Surgery 1998 January;15(1):11-7
- Beckert S, Witte M, Wicke C, Ko¨ nigsrainer A, Coerper S. A new wound-based severity score for diabetic foot ulcers. Diabetes Care 2006;29:988–992.
- Lipsky BA. Osteomyelitis of the Foot in Diabetic Patients. Clinical Infectious Diseases 1997;25:1318-26.
- Rathur HM, Boulton AJM. Pathogenesis of foot ulcers. Hormonal Metabolism Research 2005;36:61-8.
- Jeffcoate W, Lima J, Nobrega L. The Charcot foot. Diabetic Medicine 2000;17:253-8.
- Tooke JE: European Consensus Document on Critical Limb Ischaemia. Implications for Diabetes. Diabetic Medicine 1990;7:544-6.
- Edmonds ME, Morrison, Laws JW et al. Medical arterial calcification and diabetic neuropathy. British Medical Journal 1982 March;284:929-930.
- Boulton A.J.M.: The Diabetic Foot: Neuropathic in Aetiology?, Diabetic Medicine (1990):7, 852-7.
- Pham H., C. Harvey, B.I. Rosenblum, et al.: Risk Factors for the Development of Foot Ulceration: One Year Prospective Follow-Up, Diabetes, (May 1998), 47, Suppl.1, A 19.
- Reiber GE, Smith DG, Vileikyte L et al. Causal Pathways for Incident Lower – Extremity Ulcers in Patients with Diabetes from Two Settings. Diabetes Care 1999 January;22(1):157-162.
- Das AK, Agarwal A. A precipitating factor in tropical diabetic foot ulcer in India, J. Assoc Physicians India 1991 May;39(5):426.
- Harding KG, Morris HC, Patel GD, Science, Medicine and the future: Healing chronic wounds. BMJ 2002;324:160-3.
- Portero - ottn M, Pamplona R, Bellmunt MJ et al. Advanced glycation end product precursors impair epidermal growth factor receptor signaling. Diabetes 2002;57:1535-42.
- Moore K, Ruge F, Harding KG. T lymphocytes and the lack of activated macrophages in wound margin biopsies from chronic leg ulcers, Br. J. Dermatol 1997;137:188 - 94.
- Harding KG, Morris HL, Patel GD. Science, Medicine and the future; Healing chronic wounds. BMJ 2002;324:160-3.
- Lavery A.L., D.G. Armstrong, L.B. Harkless: Classification of Diabetic Foot Wounds, The Journal of Foot and Ankle Surgery, (1996), Vol. 35, Nr. 6, 528-31.
- Boulton AJM,Gries FA, Jervell JA. Guidelines for diagnosis and outpatient management of diabetic peripheral neuropathy. Diabet Med June1998;15(6):508-514.
- Kreither KF, Kalden, Nenfang A et al. Diabetes and peripheral arterial occlusive disease diagnosis. Am. J. Roentgenol, 2000;174:171-179.
- Brash PD, Foster J,Vennar W et al. Magnetic resonance imaging techniques demonstrate soft tissue damage in the diabetic foot, Diabetic Medicine 1999; 16:55-61.
- Venkatesan P, Lawn S, Macfarlane RM et al. Conservative Management of Osteomyelitis in the Feet of Diabetic Patients. Diabetic Medicine 1997;14:487-490.
- Fleischli JG, Lavery LA, Vela SA et al. Comparison of Strategies for Reducing Pressure at the Site of Neuropathic Ulcers. Journal of the American Podiatric Medical Association 1997;87(10):466-472.
- Muller MJ, Diamond JE, Sinacore DR et al. Total Contact Casting in Treatment of Diabetic Plantar Ulcers. Diabetes Care 1989;12(6):384-8.
- Knowles EA, Boulton AJM. Do People with Diabetes Wear Their Prescribed Footwear? Diabetic Medicine 1996;13:1064-8.
- Thomas S, Andrews A, Jones M et al. Maggots are useful in treating infected or necrotic wounds. BMJ 1999;318(7186):807-8.
- a. Fisken R.A., M. Digby: Which dressing for diabetic foot ulcers?, Practical Diabetes International, (July/August1996), Vol. 13, Nr.4, 107-9.
- LoGerfo FW, Gibbons GW, Pomposelli FB et al. Evolving trends in the management of the diabetic foot. Arch.Surg 1992;127:617-21.
- Burgess,EM, Romano RL, Zettl JH et al. Amputations of the leg for peripheral vascular insufficiency. J Bone Joint Surgery 1971;53; 874-89.
- Edmonds M E, H Walters : Angioplasty and the diabetic foot, Vascular Medicine Review 1995;6:205-14.
- Pedersen AE, Bornefeldt Olsen B, Krasnik M et al. Halving the Number of Leg Amputations. The Influence of Infrapopliteal Bypass. Eur J. Vacs Surg 1994;8 :26-30.
- Edmonds ME, Foster AV, Mc.Colgan M. "Dermagraft".a New Treatment for Diabetic Foot Ulcers. Diabetic Medicine 1997;14:1010- 11.
- European Committee on Hyperbaric Medicine: Hyperbaric Oxygen in the Management of foot lesions in diabetic patients. Diab. Nutr. Metab 1999; 12:47-8.
- Wieman TJ, Smiell JM, Su Y. Efficacy and Safety of a Topical Gel Formulation of Recombinant Human Platelet - Derived Growth Factor -BB (Becaplermin) in Patients with Chronic Neuropathic Diabetic Ulcers. Diabetes Care 1998;21(5):822 - 7.
- Richard J, Bringer L, Richard PC et al. Effect of Topical Basic Fibroblast Growth Factor on the Healing of Chronic Diabetic Neuropathic Ulcers of the foot. Diabetes Care 1995;18(1):64-9.
- Gough A, Clapperton M, Ronaldo N et al. Granulocyte - colony -stimulating factor in diabetic foot infection. Lancet 1997;35:855 -9.
- Van Ross ERE. After Amputation - Rehabilitation of the Diabetic Amputee. J. Am. Podiatr Med. Assoc 1997;87(7):332 - 5.
- Moore TJ, Barron J, Jutchinson F et al. Prosthetic usage following major lower extremity amputation. Clin. Orthop1989;238:219 -224.
- Fletcher ER, MacFarlane, Jeffcoate W et al. Can foot ulcers be prevented by education? Diabetic Medicine 1992 ; 9(2):41.
- Jaegeblad G., J. Apelqvist, P.Nyberg, et al.:The diabetic foot: from ulcer to multidisciplinary team approach a process analysis, The Diabetic Foot, Third International Symposium, 5th– 8th May 1999, Nordwijkerhout, The Netherlands, p87
- Grayson ML, Gibbons GW, Balogh K et al. Probing to bone in infected pedal ulcers: a clinical sign of underlying osteomyelitis in diabetic patients. J Am Med Assoc 1995;273:721–3.
- Reed JF. An audit of lower extremity complication in patients with Diabetes mellitus. International Journal Lower Extremity Wounds, 2004;3:161-4.
- Centers for Disease Control and Prevention. Data and Trends: National Diabetes Surveillance System, Vol. 2006, National Center for Chronic Disease Prevention and Health Promotion, Atlanta, 2005.
- Prompers L, Schaper N, Apelqvist J et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The Eurodiale study. Diabetologia 2008;51:747–755
- Oyibo SO, Jude EB, Tarawneh I et al. The effects of ulcer size and site, patient’s age, sex and type and duration of Diabetes on the outcome of diabetic foot ulcers. Diabet Med 2001;18:133–8.
- Jeffcoate WJ, Chipchase SY, Ince P et al.Assessing the outcome of the management of diabetic foot ulcers using ulcer-related and person-related measures. Diabetes Care 2006;29:1784–7.
- Gul A, Basit A, Ali SM, Ahmadani MY et al. Role of wound classification in predicting the outcome of diabetic foot ulcer. J Pak Med Assoc 2006;56:444–7
- Margolis DJ, Allen-Taylor L, Hoffstad O et al. Diabetic neuropathic foot ulcers and amputation. Wound Repair Regen 2005;13:230 –6.
Policy for Articles with Open Access
Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms:
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
 Home
Home