|
Table of Content - Volume 20 Issue 2 - November 2021
Novel prognostic scoring system for emphysematous pyelonephritis - EPRO scoring system
Sivasankar M1, Griffin M2*, Dev Krishna Bharathi C3, Gaurav Chintaman Kulkarni4, V Kamaraj5, Muthulatha N6
1,5,6Professor, 2Associate Professor, 3Assistant Professor, 4Senior Resident, Department of Urology, Saveetha Medical College Hospital, Chennai, INDIA. Email: aureliusgriffin@gmail.com
Abstract Background: As emphysematous pyelonephritis is an urological emergency due to its severe and aggressive nature, prompt and effective diagnosis and management is most imperative and need of the hour. We studied all the possible risk factors in the patients in our study and developed a new prognostic scoring system in the patients of emphysematous pyelonephritis. Our retrospective study involved 40 patients from the Saveetha Medical College and Hospital, Chennai over a time period of over 2 years. Emphysematous pyelonephritis was diagnosed with the help of computed tomography and was classified accordingly. We studied the risk factors in all our patients and found out seven factors which were statistically significant and dominated the prognosis of the patient. We based our EPRO scoring system on these seven factors. Diagnosing the poor prognostic patients and managing them vigorously can improve the outcome in these patients. Keywords: Emphysematous Pyelonephritis, Percutaneous Nephrostomy, Nephrectomy, Double J Stenting.
INTRODUCTION Emphysematous Pyelonephritis is a rare, severe, acute, necrotizing infection of the kidney characterized by presence of gas within the renal parenchyma, collection system and perirenal tissue1,2. Kelly and McCallum reported in 1898 the index case of EPN. It had a high mortality rate during the 1980s when they were managed with non surgical means that eventually resulted in nephrectomies. However with the advent of radiological imaging and higher antibiotics, most the cases are being managed conservatively with a significant drop in the mortality rate. Special attention must be given to EPN due to life threatening septic complications associated with it. 40 cases of Emphysematous Pyelonephritis were managed at our Medical Institute. Aims And Objectives: To study the different prognostic factors in EPN. To device a prognostic scoring system for EPN.
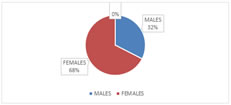
MATERIALS AND METHODS Type of study – Retrospective study. Period of study – September 2018 to December 2020. Location of study –Saveetha Medical College and Hospital, Chennai. Total cases – 40. The patients are admitted from the OPD or the Emergency Room. The diagnosis of EPN is done with the plain CT-KUB. After confirming the diagnosis, the patient is subjected to following investigations – complete blood count, renal function test, liver function test, random blood sugar and HBA1C, prothrombin time, serum electrolytes and proteins, urine analysis and culture, blood culture. Figure 1: GENDER PIE CHART
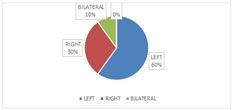
Figure 2: LATERALITY PIE CHART
Table 1.P value
RESULTS The mean age of the patients in our study was 54.9 ± 9.01 yrs. Out of 40 patients 27 were females and 13 were males(67.5%). Out of 40, 24 had pathology on the left side, 12 on the right side while 4 had bilateral disease. 36 patients were diabetic (90%).Out of 40, 6 patients were alcoholic ( 15% ). Hypertension was seen in 11 patients (27.5%). Cardiovascular accident was found in 1 patient (2.5%). Liver cirrhosis in 3 patients (7.5%). Urolithiasis was present in 21 patients (52.5%). 4 patients had thrombocytopenia (10%). Hypoalbuminemia in 5 patients (12.5%). 3 patients presented with shock (7.5%). 4 patients were on haemodialysis (10%). 12 patients presented with acute kidney injury (30%). 11 patients were found to have hyponatremia (27.5%). 7 patients had altered mental status (7.5%). 38 patients had pyuria (95%). Haematuria was present in 13 patients (32.5%). High HBA1C was found in 33 patients (82.5%). Alkaline phosphatase was elevated in 19 patients (47.5%). 6 patients were found to have polymicrobial infection (15%). E.coli was found inurinecultures of24 patients (63.15%). Proteus was found in 5 patients (13.15%). 4 patients had klebsiella infection (10.5%). 3 patients had pseudomonas infection (7.89%). Two patients had other infections than mentioned above. Blood culture showed E.coli infection in 3 patients (7.89%). One patient each had pseudomonas and klebsiella grown in blood culture (2.63% each). As per Huang classification, 9 patients fell in class 1 (22.5%), 15 patients were class 2 (37.5%), 7 patients were class 3A (17.5%), 4 patients were class 3B (10%) while 5 patients were class 4 (12.5%). 37 patients out of 40 recovered (92.5%) while 3 patients did not survive (7.5%).
DISCUSSION This study is a retrospective study done in our institute which includes 40 cases over a time period of two years. EPN is a urological emergency which needs upfront management due to its high complication rates. Our study focuses on all possible factors that are indicative of high mortality and poor outcome and figure out a trustworthy scoring system that indicates the poor prognosis in the cases of EPN. Most common risk factor was found out to be diabetes mellitus. Computed Tomography was used as the investigation of choice for diagnosing EPN. Based on its findings, patients were categorized as per Huang classification. 24 patients were managed solely with antibiotics, while 16 patients required surgical intervention in form of either percutaneous drainage or double J stents or nephrectomy along with antibiotics. Only four patients were found to have bilateral disease while one patient had EPN in solitary kidney. E.coli and Kleibsella turned out to be most common causative organisms. Out of 40 patients, 3 patients didn’t survive; one with solitary kidney and two with bilateral disease. Both these patients had common findings like alcoholic liver disease, thrombocytopenia, hypoalbuminemia, polymicrobial infections, and septic shock. Decision of surgical intervention was taken based upon their Huang classification, clinical presentation, failed medical management and progressive disease. Nephrectomy was required in two cases. Patients that were managed with antibiotics and PCD/DJ stenting had less mortality compared to nephrectomy. Thrombocytopenia, altered mental status and septic shock showed poor outcome2-6. Our study showed thrombocytopenia (p-0.005), shock (p-0.036) were contributing factors along with liver cirrhosis (p-0.03), hypoalbuminemia (p-0.01), bacteraemia (p-0.01), haemodialysis requirement (p-0.005) and polymicrobial infections (p-0.02). With the advancement of imaging technologies and efficient medical and surgical management, mortality has decreased considerably compared to older times when it used to be 50-60%7. Taking into consideration all the seven statistically significant factors five or more factors in a single patient is indicative of poor prognosis.
CONCLUSION EPN is no longer a high mortality disease like it used to be in the previous era, thanks to the radiological imaging and prompt management. Early diagnosis is possible and vigilant monitoring coupled with aggressive management is the need of the hour. Terminal treatment measure like nephrectomy is rarely required. Using the EPRO scoring system, poor prognosis can be effectively predicted and can be managed accordingly.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home